Abstract
Purpose
To determine predictors of chronic pain and disability among patients with distal radius fractures (DRF) treated conservatively with closed reduction and cast immobilization.
Methods
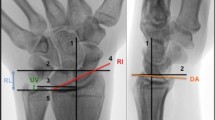
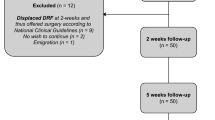
This was a prospective cohort study. Information on patient characteristics, post-reduction radiographic parameters, finger and wrist range of motion, psychological status (Hospital Anxiety and Depression Scale or HADS), pain (Numeric Rating Scale or NRS), and self-perceived disability (Disabilities of the Arm, Should, and Hand or DASH) were taken at baseline, cast removal, and 24 weeks. Differences in outcomes between time points were determined using analysis of variance. Multiple linear regressions were used to determine predictors of pain and disability at 24 weeks.
Results
One hundred forty patients with DRF (70% women, age: 67.0 ± 17.9) completed 24 weeks of follow-up and were included in the analysis. NRS (off-cast), range of ulnar deviation (off-cast), and greater occupational demands were significant predictors of pain at week 24 (adjusted R2 = 0.331, p < 0.001). Significant predictors of perceived disability at week 24 were HADS (off cast), sex (female), dominant-hand injury, and range of ulnar deviation (off cast) (adjusted R2 = 0.265, p < 0.001).
Conclusions
Off-cast NRS and HADS scores are important modifiable predictors of patient-reported pain and disability at 24 weeks in patients with DRF. These factors should be targeted in the prevention of chronic pain and disability post-DRF.

Similar content being viewed by others
Data availability
Data are available upon request.
Code availability
Not applicable. No custom written code/program was used. SPSS (version 26, IBM Corp., Armonk, NY, USA) is commercially available software. G*Power (version 3.1.2, Franz Faul, University of Kiel, Germany) is freely available open source software.
References
Wakefield AE, McQueen MM (2000) The role of physiotherapy and clinical predictors of outcome after fracture of the distal radius. J Bone Joint Surg Br 82:972–976. https://doi.org/10.1302/0301-620X.82B7.0820972
Chung KC, Shauver MJ, Birkmeyer JD (2009) Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am 91:1868–1873. https://doi.org/10.2106/JBJS.H.01297
Chung KC, Spilson SV (2001) The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am 26:908–915. https://doi.org/10.1053/jhsu.2001.26322
MacDermid JC, Roth JH, Richards RS (2003) Pain and disability reported in the year following a distal radius fracture: a cohort study. BMC Musculoskelet Disord 4:24. https://doi.org/10.1186/1471-2474-4-24
Moore CM, Leonardi-Bee J (2008) The prevalence of pain and disability one year post fracture of the distal radius in a UK population: a cross sectional survey. BMC Musculoskelet Disord 9:129. https://doi.org/10.1186/1471-2474-9-129
Grewal R, MacDermid JC, Pope J, Chesworth BM (2007) Baseline predictors of pain and disability one year following extra-articular distal radius fractures. Hand (N Y) 2:104–111. https://doi.org/10.1007/s11552-007-9030-x
Lindau T, Arner M, Hagberg L (1997) Intraarticular lesions in distal fractures of the radius in young adults: a descriptive arthroscopic study in 50 patients. J Hand Surg Br 22:638–643. https://doi.org/10.1016/S0266-7681(97)80364-6
Van Son MAC, De Vries J, Roukema JA, Den Oudsten BL (2013) Health status and (health-related) quality of life during the recovery of distal radius fractures: a systematic review. Qual Life Res 22:2399–2416. https://doi.org/10.1007/s11136-013-0391-z
Karnezis IA, Panagiotopoulos E, Tyllianakis M, Megas P, Lambiris E (2005) Correlation between radiological parameters and patient-rated wrist dysfunction following fractures of the distal radius. Injury 36:1435–1439. https://doi.org/10.1016/j.injury.2005.09.005
Wilcke MKT, Abbaszadegan H, Adolphson PY (2007) Patient-perceived outcome after displaced distal radius fractures: a comparison between radiological parameters, objective physical variables, and the DASH score. J Hand Ther 20:290–299. https://doi.org/10.1197/j.jht.2007.06.001
Brogren E, Hofer M, Petranek M, Dahlin LB, Atroshi I (2011) Fractures of the distal radius in women aged 50 to 75 years: natural course of patient-reported outcome, wrist motion and grip strength between 1 year and 2–4 years after fracture. J Hand Surg Eur Vol 36:568–576. https://doi.org/10.1177/1753193411409317
Kumar S, Penematsa S, Sadri M, Deshmukh SC (2008) Can radiological results be surrogate markers of functional outcome in distal radial extra-articular fractures? Int Orthop 32:505–509. https://doi.org/10.1007/s00264-007-0355-4
Nelson GN, Stepan JG, Osei DA, Calfee RP (2015) The impact of patient activity level on wrist disability after distal radius malunion in older adults. J Orthop Trauma 29:195–200. https://doi.org/10.1097/BOT.0000000000000235
Golkari S, Teunis T, Ring D, Vranceanu A-M (2015) Changes in depression, health anxiety, and pain catastrophizing between enrollment and 1 month after a radius fracture. Psychosomatics 56:652–657. https://doi.org/10.1016/j.psym.2015.03.008
Ring D, Kadzielski J, Fabian L, Zurakowski D, Malhotra LR, Jupiter JB (2006) Self-reported upper extremity health status correlates with depression. J Bone Joint Surg Am 8:1983–1988. https://doi.org/10.2106/JBJS.E.00932
Gong HS, Lee JO, Huh JK, Oh JH, Kim SH, Baek GH (2011) Comparison of depressive symptoms during the early recovery period in patients with a distal radius fracture treated by volar plating and cast immobilisation. Injury 42:1266–1270. https://doi.org/10.1016/j.injury.2011.01.005
US Department of Labor (1991) Dictionary of occupational titles, 4th edn. US Department of Labor, Washington DC
Mehta SP, MacDermid JC, Richardson J, MacIntyre NJ, Grewal R (2015) Baseline pain intensity is a predictor of chronic pain in individuals with distal radius fracture. J Orthop Sports Phys Ther 45:119–127. https://doi.org/10.2519/jospt.2015.5129
MacDermid JC, Roth JH, McMurtry R (2007) Predictors of time lost from work following a distal radius fracture. J Occup Rehabil 17:47–62. https://doi.org/10.1007/s10926-007-9069-0
Dietrich M, Wasmer M, Platz A, Spross C (2014) Return-to-work following open reduction and internal fixation of proximal humerus fractures. Open Orthop J 8:281–287. https://doi.org/10.2174/1874325001408010281
Chung KC, Kotsis SV, Kim HM (2007) Predictors of functional outcomes after surgical treatment of distal radius fractures. J Hand Surg Am 32:76–83. https://doi.org/10.1016/j.jhsa.2006.10.010
MacDermid JC, Donner A, Richards RS, Roth JH (2002) Patient versus injury factors as predictors of pain and disability six months after a distal radius fracture. J Clin Epidemiol 55:849–854. https://doi.org/10.1016/S0895-4356(02)00445-6
Amadio PC, Botte MJ (1987) Treatment of malunion of the distal radius. Hand Clin 3:541–561
Bu J, Patterson RM, Morris R, Yang J, Viegas SF (2006) The effect of radial shortening on wrist joint mechanics in cadaver specimens with inherent differences in ulnar variance. J Hand Surg Am 31:1594–1600. https://doi.org/10.1016/j.jhsa.2006.09.004
Jenkins NH, Mintowt-Czyz WJ (1988) Mal-union and dysfunction in colles’ fracture. J Hand Surg Br 13:291–293. https://doi.org/10.1016/0266-7681_88_90090-3
McQueen M, Caspers J (1988) Colles fracture: does the anatomical result affect the final function? J Bone Joint Surg Br 70:649–651. https://doi.org/10.1302/0301-620X.70B4.3403617
Richards RS, Bennett JD, Roth JH, Milne K (1997) Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg Am 22:772–776. https://doi.org/10.1016/S0363-5023(97)80068-8
Palmer AK, Werner FW (1984) Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res 187:26–35
Isa AD, McGregor ME, Padmore CE, Langohr DG, Johnson JA, King GJW, Suh N (2019) Effect of radial lengthening on distal forearm loading following simulated in vitro radial shortening during simulated dynamic wrist motion. J Hand Surg Am 44:556-563.e555. https://doi.org/10.1016/j.jhsa.2019.03.017
Bhandari M, Busse JW, Hanson BP, Leece P, Ayeni OR, Schemitsch EH (2008) Psychological distress and quality of life after orthopedic trauma: an observational study. Can J Surg 51:15–22
Crichlow RJ, Andres PL, Morrison SM, Haley SM, Vrahas MS (2006) Depression in orthopaedic trauma patients: prevalence and severity. J Bone Joint Surg Am 8:1927–1933. https://doi.org/10.2106/JBJS.D.02604
Edwards BJ, Song J, Dunlop DD, Fink HA, Cauley JA (2010) Functional decline after incident wrist fractures--study of osteoporotic fractures: prospective cohort study. BMJ (Clinical research ed.) 341:c3324. https://doi.org/10.1136/bmj.c3324
Souza MA, Dias JF, Ferreira FR, Mancini MC, Kirkwood RN, Sampaio RF (2016) Characteristics and functional demands of patients at a local rehabilitation network: analysis from first contact. Cien Saude Colet 21:3277–3286. https://doi.org/10.1590/1413-812320152110.11192016
Karacan I, Sariyildiz MA, Bahadir C (2010) Effect of bone tissue on vibration-induced electrical activity of muscles. Turkiye Klinikleri Tip Bilimleri Dergisi 30:1346–1356
Beaulé P-E, Dervin GF, Giachino AA, Rody K, Grabowski J, Fazekas A (2000) Self-reported disability following distal radius fractures: the influence of hand dominance. J Hand Surg Am 25:476–482. https://doi.org/10.1016/S0363-5023(00)70027-X
Lalone E, MacDermid J, Grewal R, King G (2017) Patient reported pain and disability following a distal radius fracture: a prospective study. Open Orthop J 11:589–599. https://doi.org/10.2174/1874325001711010589
Acknowledgements
This research did not receive any specific grants from funding agencies in the public, commercial, or non-profit sectors. Support of manpower and infrastructure were provided by Queen Elizabeth Hospital.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. Material preparation, data collection, and analysis were performed by May Lai Mei Luk, Andy Chi Ming Chan, Jocelyn Sau Yee Cho, Daisy Mei Ting Ng, Isa Chui Yi Lam, Edmund Leung Kai Yau, Tiev Miller, and Marco Yiu Chung Pang. The initial manuscript was drafted by May Lai Mei Luk. Subsequent versions of the manuscript were drafted by Tiev Miller and Marco Yui Chung Pang. All authors commented on previous versions and have approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was granted by the Hong Kong Polytechnic University Research Committee (HSEARS20160624002) and the Kowloon Central Cluster/Kowloon East Cluster Research Ethics Committee (KC/KE-16–0208/ER-3).
Consent to participate
Informed consent was obtained from all participants prior to data collection.
Consent to publish
Not applicable. No names, photographs, or identifying information were disclosed.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luk, M.L.M., Chan, A.C.M., Cho, J.S.Y. et al. Predictors of chronic pain and disability in patients treated conservatively after distal radius fracture: a prospective cohort study. International Orthopaedics (SICOT) 47, 1535–1543 (2023). https://doi.org/10.1007/s00264-023-05785-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05785-y