Abstract
Purpose
This study aimed to investigate the efficacy and safety of autologous platelet-rich plasma (PRP) and bone marrow mononuclear cells (BMMCs) grafting combined with core decompression (CD) in the treatment of Association Research Circulation Osseous (ARCO) II–IIIA stage non-traumatic osteonecrosis of the femoral head (ONFH).
Methods
The clinical data of 44 patients (44 hips) with non-traumatic ONFH from December 2018 to December 2019 were retrospectively reviewed. Twenty-four patients underwent CD combined with autologous PRP and BMMCs grafting (PRP+BMMCs group), and 20 patients underwent core decompression alone (CD group). During a minimum follow-up of 36 months, radiographic outcomes were evaluated using X-ray, radiographic failure rates were compared, and Harris hip score (HHS) and visual analog scale (VAS) were selected to evaluate clinical outcomes. The percentage of patients with minimal clinically important difference (MCID) in both groups was analyzed. Clinical failure was defined as further total hip arthroplasty (THA) with Kaplan-Meier survival analysis. Surgical complications were recorded.
Results
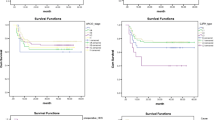
All patients had well healed wounds, and no complications such as infection and thrombosis occurred. HHS and VAS scores in both the PRP+BMMCs and CD groups were better than those preoperatively (P<0.05). At the last follow-up, the HHS and VAS scores of the PRP+BMMCs group were significantly better than those of the CD group (P<0.05). In ARCO II–IIIA stage, 66.7% of the PRP+BMMCs group and 30.0% of the CD group achieved the MCID (P<0.05). The clinical and imaging failure rates in the PRP+BMMCs group were 12.5% and 20.8%, respectively, compared with 40.0% and 50.0% in the CD group (P<0.05). In ARCO II stage, the MCID, clinical and imaging failure rates of PRP+BMMCs group and CD group were 66.7% and 33.3% (P<0.05), 4.8% and 33.3% (P<0.05), 14.3% and 44.4% (P<0.05), respectively. The PRP+BMMCs group had better hip survival rate compared with CD group (P<0.05).
Conclusion
CD combined with autologous PRP and BMMCs grafting is a safe and effective method for the treatment of ARCO II–IIIA stage non-traumatic ONFH, especially for ARCO II stage, effectively reducing the collapse rate of the femoral head and delaying or even avoiding THA.



Similar content being viewed by others
References
Schroer WC (1994) Current concepts on the pathogenesis of osteonecrosis of the femoral head. Orthop Rev 23:487–497
Mont MA, Cherian JJ, Sierra RJ, Jones LC, Lieberman JR (2015) Nontraumatic osteonecrosis of the femoral head: where do we stand today? A ten-year update. J Bone Joint Surg Am 97:1604–1627
Lee HR, Park KM, Joung YK, Park KD, Do SH (2012) Platelet-rich plasma loaded hydrogel scaffold enhances chondrogenic differentiation and maturation with up-regulation of CB1 and CB2. J control release 159:332–337
Marker DR, Seyler TM, McGrath MS, Delanois RE, Ulrich SD, Mont MA (2008) Treatment of early stage osteonecrosis of the femoral head. J bone joint surg am 90(Suppl 4):175–187
Rackwitz L, Eden L, Reppenhagen S, Reichert JC, Jakob F, Walles H, Pullig O, Tuan RS, Rudert M, Nöth U (2012) Stem cell- and growth factor-based regenerative therapies for avascular necrosis of the femoral head. Stem Cell Res Ther 3:7
Arora NS, Ramanayake T, Ren YF, Romanos GE (2009) Platelet-rich plasma: a literature review. Implant dent 18:303–310
Sampson S, Gerhardt M, Mandelbaum B (2008) Platelet rich plasma injection grafts for musculoskeletal injuries: a review. Curr rev musculoske 1:165–174
Henrich D, Verboket R, Schaible A, Kontradowitz K, Oppermann E, Brune JC, Nau C, Meier S, Bonig H, Marzi I, Seebach C (2015) Characterization of bone marrow mononuclear cells on biomaterials for bone tissue engineering in vitro. Biomed res int 2015:762407
Sugano N, Atsumi T, Ohzono K, Kubo T, Hotokebuchi T, Takaoka K (2002) The 2001 revised criteria for diagnosis, classification, and staging of idiopathic osteonecrosis of the femoral head. J orthop sci 7:601–605
Xian H, Luo D, Wang L, Cheng W, Zhai W, Lian K, Lin D (2020) Platelet-rich plasma-incorporated autologous granular bone grafts improve outcomes of post-traumatic osteonecrosis of the femoral head. J arthroplasty 35:325–330
Wang D, Wang G, Liu M, Sun L, Zong W, Jiang H, Zhang H, Li H, Gong J, Sun S (2014) A novel animal model of osteonecrosis of the femoral head induced using a magnetic resonance imaging-guided argon-helium cryotherapy system. Exp ther med 7:1525–1528
Liang D, Pei J, Zhang L, Ling H, Liu Y, Chen X (2021) Treatment of pre-collapse non-traumatic osteonecrosis of the femoral head through Orthopdische Chirurgie München approach combined with autologous bone mixed with β-tricalcium phosphate porous bioceramic bone graft: a retrospective study of mid-term results. J Orthop Surg Res 16:492
Lieberman JR, Engstrom SM, Meneghini RM, SooHoo NF (2012) Which factors influence preservation of the osteonecrotic femoral head? Clin orthop relat r 470:525–534
Marker DR, Seyler TM, Ulrich SD, Srivastava S, Mont MA (2008) Do modern techniques improve core decompression outcomes for hip osteonecrosis? Clin orthop relat r 466:1093–1103
Oryan A, Alidadi S, Moshiri A (2016) Platelet-rich plasma for bone healing and regeneration. Expert opin biol th 16:213–232
Boswell SG, Cole BJ, Sundman EA, Karas V, Fortier LA (2012) Platelet-rich plasma: a milieu of bioactive factors. Arthroscopy 28:429–439
Latalski M, Elbatrawy YA, Thabet AM, Gregosiewicz A, Raganowicz T, Fatyga M (2011) Enhancing bone healing during distraction osteogenesis with platelet-rich plasma. Injury 42:821–824
Kitoh H, Kitakoji T, Tsuchiya H, Mitsuyama H, Nakamura H, Katoh M, Ishiguro N (2004) Transplantation of marrow-derived mesenchymal stem cells and platelet-rich plasma during distraction osteogenesis--a preliminary result of three cases. Bone 35:892–898
Hakimi M, Jungbluth P, Sager M, Betsch M, Herten M, Becker J, Windolf J, Wild M (2010) Combined use of platelet-rich plasma and autologous bone grafts in the treatment of long bone defects in mini-pigs. Injury 41:717–723
Bowen-Pope DF, Vogel A, Ross R (1984) Production of platelet-derived growth factor-like molecules and reduced expression of platelet-derived growth factor receptors accompany transformation by a wide spectrum of agents. P natl acad sci USA 81:2396–2400
Wu PI, Diaz R, Borg-Stein J (2016) Platelet-rich plasma. Phys med reh clin n 27:825–853
Wang BL, Sun W, Shi ZC, Zhang NF, Yue DB, Guo WS, Xu SQ, Lou JN, Li ZR (2010) Treatment of nontraumatic osteonecrosis of the femoral head with the implantation of core decompression and concentrated autologous bone marrow containing mononuclear cells. Arch orthop traum su 130:859–865
D'Asta F, Halstead F, Harrison P, Zecchi Orlandini S, Moiemen N, Lord J (2018) The contribution of leucocytes to the antimicrobial activity of platelet-rich plasma preparations: a systematic review. Platelets 29:9–20
Hernigou P, Habibi A, Bachir D, Galacteros F (2006) The natural history of asymptomatic osteonecrosis of the femoral head in adults with sickle cell disease. J bone joint surg am 88:2565–2572
Nam KW, Kim YL, Yoo JJ, Koo KH, Yoon KS, Kim HJ (2008) Fate of untreated asymptomatic osteonecrosis of the femoral head. J bone joint surg am 90:477–484
Dean MT, Cabanela ME (1993) Transtrochanteric anterior rotational osteotomy for avascular necrosis of the femoral head. Long-term results. J bone joint surg br 75:597–601
Hernigou P, Poignard A, Zilber S, Rouard H (2009) Cell therapy of hip osteonecrosis with autologous bone marrow grafting. Indian j orthop 43:40–45
Gangji V, De Maertelaer V, Hauzeur JP (2011) Autologous bone marrow cell implantation in the treatment of non-traumatic osteonecrosis of the femoral head: five year follow-up of a prospective controlled study. Bone 49:1005–1009
Piuzzi NS, Chahla J, Schrock JB, LaPrade RF, Pascual-Garrido C, Mont MA, Muschler GF (2017) Evidence for the use of cell-based therapy for the treatment of osteonecrosis of the femoral head: a systematic review of the literature. J arthroplasty 32:1698–1708
Nally FJ, Zanotti G, Buttaro MA, Diaz Dilernia F, Mansilla IG, Comba FM, Piccaluga F (2018) THA conversion rate comparing decompression alone, with autologous bone graft or stem cells in osteonecrosis. Hip int 28:189–193
Availability of data and materials
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable
Funding
This study was supported by the special subject of scientific research on traditional Chinese medicine in Henan Province (20-21ZY2085).
Author information
Authors and Affiliations
Contributions
Dawei Liang contributed significantly to analysis and wrote the manuscript. Jia Pei and Xiantao Chen performed the data analyses. Xiaohui Zhang helped perform the analysis with constructive discussions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the medical Ethics Committee of the Luoyang Orthopedic-Traumatological Hospital of Henan Province (Henan Provincial Orthopedic Hospital) institution.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The manuscript is approved by all authors for publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liang, D., Pei, J., Zhang, X. et al. Clinical outcomes of autologous platelet-rich plasma and bone marrow mononuclear cells grafting combined with core decompression for Association Research Circulation Osseous II–IIIA stage non-traumatic osteonecrosis of the femoral head. International Orthopaedics (SICOT) 47, 2181–2188 (2023). https://doi.org/10.1007/s00264-023-05779-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05779-w