Abstract
Study design
Retrospective study.
Purpose
The aim of this study was to develop a predictive model for determining perioperative blood transfusion in tuberculous spondylitis patients undergoing posterior decompression and instrumentation.
Background
Tuberculous spondylitis is a common infection found in the spine. This condition may result in the need of surgical treatment, especially when there is a delay in diagnosis with inadequate antituberculosis drug treatment. The procedure results in high amount of bleeding on many occasions, leading to the higher rate of intraoperative transfusion. We develop a predictive model that can be used to determine blood transfusion requirement in spinal tuberculosis surgery.
Methods
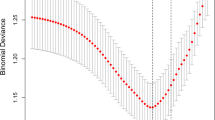
We reviewed the medical records of 83 tuberculous spondylitis patients who underwent posterior decompression and instrumentation. The clinical characteristics of the patients were analyzed using bivariate and multivariate regression test. The impact and strength of these variables was assessed to predict the probability of intraoperative red blood cell transfusion presence based on unstandardized beta, standard error, receiver operating characteristic, and confluence of sensitivity and specificity curve analyses. Furthermore, validation of this newly proposed predictive scoring system was performed using a set of 45 patients.
Results
The factors that significantly affect the need of blood transfusion during posterior spondylitis tuberculosis surgery were BMI (p = 0.005), pre-operative Hb (p < 0.001), number of affected segments (p = 0.042), and duration of surgery (p = 0.003). Our predictive model showed good sensitivity and specificity values based on a large area under the curve (0.913) and strong Pearson’s r testing (correlation coefficient of 0.752). Validation set also resulted a large area under the curve (0.905) and strong correlation coefficient of 0.713.
Conclusion
BMI, pre-operative Hb, number of affected segments, and duration of surgery became the significant factors which correlated to the presence of red blood cell transfusion in patients undergoing posterior spondylitis tuberculosis surgery. This predictive scoring system can be used to further adjust blood matching and inventory, determine intraoperative blood management, and ensure the safety of surgery in a comprehensive manner.


Similar content being viewed by others
Data availability
All the data are available can be accessed via corresponding email after clearly stating the intention and permission to conduct research that requires our data.
Code availability
Data are available upon requests.
References
Rasouli MR, Mirkoohi M, Vaccaro AR et al (2012) Spinal tuberculosis: diagnosis and management. Asian Spine J 6:294–308. https://doi.org/10.4184/asj.2012.6.4.294
Ahuja K, Ifthekar S, Mittal S et al (2021) Defining mechanical instability in tuberculosis of the spine: a systematic review. EFORT Open Rev 6:202–210. https://doi.org/10.1302/2058-5241.6.200113
Zou H, Li Z, Sheng H et al (2015) Intraoperative blood loss, postoperative drainage, and recovery in patients undergoing lumbar spinal surgery. BMC Surg 15:76. https://doi.org/10.1186/s12893-015-0062-9
Islam NC, Wood KB, Transfeldt EE et al (2001) Extension of fusions to the pelvis in idiopathic scoliosis. Spine (Phila Pa 1976) 26:166–173. https://doi.org/10.1097/00007632-200101150-00011
Liu Z, Liu J, Peng A et al (2014) One-stage posterior debridement and transpedicular screw fixation for treating monosegmental thoracic and lumbar spinal tuberculosis in adults. Sci World J 2014:137106. https://doi.org/10.1155/2014/137106
Droz NM, Lin J, Beach J et al (2021) Decreased transfusion requirements with use of acute normovolemic hemodilution in open aortic aneurysm repair. J Vasc Surg 74:1885–1893. https://doi.org/10.1016/J.JVS.2021.05.030
Pennington Z, Ehresman J, Molina CA et al (2020) A novel predictive model of intraoperative blood loss in patients undergoing elective lumbar surgery for degenerative pathologies. Spine J 20:1976–1985. https://doi.org/10.1016/j.spinee.2020.06.019
Noticewala MS, Nyce JD, Wang W et al (2012) Predicting need for allogeneic transfusion after total knee arthroplasty. J Arthroplasty 27:961–967. https://doi.org/10.1016/J.ARTH.2011.10.008
Wang M, Chen M, Ao H et al (2017) The effects of different BMI on blood loss and transfusions in Chinese patients undergoing coronary artery bypass grafting. Ann Thorac Cardiovasc Surg 23:83. https://doi.org/10.5761/ATCS.OA.16-00219
Ramos RD la G, Nakhla J, Nasser R et al (2017) Effect of body mass index on surgical outcomes after posterior spinal fusion for adolescent idiopathic scoliosis. Neurosurg Focus 43:E5. https://doi.org/10.3171/2017.7.FOCUS17342
Bashaireh K, Aljararhih O, Alawneh K (2020) Impact of body mass index on hemoglobin level and blood transfusion in total knee arthroplasty: a retrospective case control study. Ann Med Surg (Lond) 55:180–184. https://doi.org/10.1016/J.AMSU.2020.05.028
Salido JA, Marín LA, Gómez LA et al (2002) Preoperative hemoglobin levels and the need for transfusion after prosthetic hip and knee surgery: analysis of predictive factors. J Bone Joint Surg Series A 84:216–220+Adv78. https://doi.org/10.2106/00004623-200202000-00008
Fontanals M, O’Leary JD, Zaarour C et al (2019) Preoperative anemia increases the risk of red blood cell transfusion and prolonged hospital length of stay in children undergoing spine arthrodesis surgery. Transfusion (Paris) 59:492–499. https://doi.org/10.1111/trf.15055
Litvinov RI, Weisel JW (2017) Role of red blood cells in haemostasis and thrombosis. ISBT Sci Ser 12:176–183. https://doi.org/10.1111/VOXS.12331
Fowler AJ, Ahmad T, Phull MK et al (2015) Meta-analysis of the association between preoperative anaemia and mortality after surgery. Br J Surg 102:1314–1324
Carson JL, Noveck H, Berlin JA, Gould SA (2002) Mortality and morbidity in patients with very low postoperative Hb levels who decline blood transfusion. Transfusion (Paris) 42:812–818. https://doi.org/10.1046/j.1537-2995.2002.00123.x
Raman T, Vasquez-Montes D, Varlotta C et al (2020) Decision tree-based modelling for identification of predictors of blood loss and transfusion requirement after adult spinal deformity surgery. Int J Spine Surg 14:87–95. https://doi.org/10.14444/7012
Zhao C, Luo L, Liu L et al (2020) Surgical management of consecutive multisegment thoracic and lumbar tuberculosis: anterior-only approach vs. posterior-only approach. J Orthop Surg Res 15:343. https://doi.org/10.1186/S13018-020-01876-3
Zheng F, Cammisa FP, Sandhu HS et al (2002) Factors predicting hospital stay, operative time, blood loss, and transfusion in patients undergoing revision posterior lumbar spine decompression, fusion, and segmental instrumentation. Spine (Phila Pa 1976) 27:818–824. https://doi.org/10.1097/00007632-200204150-00008
Dong Y, Tang N, Wang S et al (2021) Risk factors for blood transfusion in adolescent patients with scoliosis undergoing scoliosis surgery: a study of 722 cases in a single center. BMC Musculoskelet Disord 22:1–8. https://doi.org/10.1186/S12891-020-03869-Z/TABLES/6
Cristante AF, Alvim Borges P, Roberto Barbosa A et al (2014) Predictive factors for perioperative blood transfusion in surgeries for correction of idiopathic, neuromuscular or congenital scoliosis. Clinics (Sao Paulo) 69:672–676. https://doi.org/10.6061/CLINICS/2014(10)04
Wang H, Wang K, Lv B et al (2021) Establishment and assessment of a nomogram for predicting blood transfusion risk in posterior lumbar spinal fusion. J Orthop Surg Res 16:39. https://doi.org/10.1186/S13018-020-02053-2
Ristagno G, Beluffi S, Tanzi D et al (2018) Red blood cell transfusion need for elective primary posterior lumbar fusion in a high-volume center for spine surgery. J Clin Med 7:19. https://doi.org/10.3390/jcm7020019
Lenoir B, Merckx P, Paugam-Burtz C et al (2009) Individual probability of allogeneic erythrocyte transfusion in elective spine surgery: the predictive model of transfusion in spine surgery. Anesthesiology 110:1050–1060. https://doi.org/10.1097/ALN.0b013e31819df9e0
Durand WM, Depasse JM, Daniels AH (2018) Predictive modeling for blood transfusion after adult spinal deformity surgery. Spine (Phila Pa 1976) 43:1058–1066. https://doi.org/10.1097/BRS.0000000000002515
Mathai KM, Kang JD, Donaldson WF et al (2012) Prediction of blood loss during surgery on the lumbar spine with the patient supported prone on the Jackson table. Spine J 12:1103–1110. https://doi.org/10.1016/j.spinee.2012.10.027
Han IH, Son DW, Nam KH et al (2012) The effect of body mass index on intra-abdominal pressure and blood loss in lumbar spine surgery. J Korean Neurosurg Soc 51:81–85. https://doi.org/10.3340/jkns.2012.51.2.81
Carabini LM, Zeeni C, Moreland NC et al (2014) Development and validation of a generalizable model for predicting major transfusion during spine fusion surgery. J Neurosurg Anesthesiol 26:205–215. https://doi.org/10.1097/ANA.0000000000000014
Hu SS (2004) Blood loss in adult spinal surgery. Eur Spine J 13:S3. https://doi.org/10.1007/S00586-004-0753-X
Liu J, Wan L, Long X et al (2015) Efficacy and safety of posterior versus combined posterior and anterior approach for the treatment of spinal tuberculosis: a meta-analysis. World Neurosurg 83:1157–1165
Author information
Authors and Affiliations
Contributions
S. Dohar A. L. Tobing: conception and design, visualization, drafting revision.
Dody Kurniawan: drafting the article, analysis, interpretation of data.
Anissa Feby Canintika: drafting the article, interpretation of data.
Fajar Defian: drafting the article, drafting revision.
Muhammad Labib Luqman Zufar: project administration, drafting revision.
Corresponding author
Ethics declarations
Ethical approval
This research has received ethical approval from The Ethics Committee of the Faculty of Medicine, Universitas Indonesia – Cipto Mangunkusumo Hospital (Protocol Number 20–02-0145).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
All authors give consent to publish this manuscript and take responsibility of all included data.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tobing, S.D.A.L., Kurniawan, D., Canintika, A.F. et al. A novel predictive model of perioperative blood transfusion requirement in tuberculous spondylitis patients undergoing posterior decompression and instrumentation. International Orthopaedics (SICOT) 47, 1545–1555 (2023). https://doi.org/10.1007/s00264-023-05744-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05744-7