Abstract
Objective
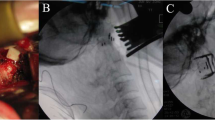
Investigate a novel method for treating irreducible atlantoaxial dislocation (IAAD) or with basilar invagination (BI) by bony deformity osteotomy, remodeling, releasing, and plate fixating through transoral approach.
Method
From March 2015 to December 2019, 213 consecutive patients diagnosed as IAAD/BI were treated with transoral bony deformity remodeling and releasing combined with plate fixation. The main clinical symptoms include neck pain, headache, numbness of the limbs, weakness, unstable walking, inflexible hand-held objects, and sphincter dysfunction. The bony factors that impact reduction were divided into as follows: type A1 (sloping of upper facet joint in C2), type A2 (osteophyte in lateral mass joints between C1 and C2), type A3 (ball-and-socket deformity of lateral mass joint), type A4 (vertical interlocking between lateral mass joints of C1–C2), type A5 (regional bone fusion in lateral mass joints), type B1 (bony factor hindering reduction between the atlas-dens gap), type B2 (uncinate odontoid deformity), and type B3 (hypertrophic odontoid deformity). All of them were treated with bony deformity osteotomy, remodeling, and releasing techs.
Result
The operation time was 144 \(\pm\) 25 min with blood loss of 102 \(\pm\) 35 ml. The average pre-operative ADI improved from 7.5 \(\pm\) 3.2 mm pre-surgery to 2.5 \(\pm\) 1.5 mm post-surgery (p < 0.05). The average VDI improved from 12.3 \(\pm\) 4.8 mm pre-surgery to 3.3 \(\pm\) 2.1 mm post-surgery (p < 0.05). The average pre-operative CMA improved from 115 \(\pm\) 25° pre-surgery to 158 \(\pm\) 21° post-surgery (p < 0.05); the pre-operative CAA changed from 101 \(\pm\) 28° pre-surgery to 141 \(\pm\) 10° post-surgery. After the operation, the clinic symptoms improved, and the JOA score improved from 9.3 \(\pm\) 2.8 pre-operatively to 13.8 \(\pm\) 2.5 in the sixth months of follow-up.
Conclusion
In addition to soft tissue factors, bony obstruction was another important factor impeding atlantoaxial reduction. Transoral bony deformity osteotomy, remodeling, releasing combined with plate fixating was effective in treating IAAD/BI with bony obstruction factors.










Similar content being viewed by others
References
Wang S, Wang C, Yan M, Zhou H, Dang G (2013) Novel surgical classification and treatment strategy for atlantoaxial dislocations[J]. Spine (Phila Pa 1976) 38(21):E1348–E1356
Mingsheng T, Long G, Ping Y, Feng Y, Xiangsheng T, Haoning M, Qinying H (2020) New classification and its value evaluation for atlantoaxial dislocation. Orthop Surg 12(4):1199–1204
Xu J, Yin Q, Xia H, Wu Z, Ma X, Zhang K, Wang Z, Yang J, Ai F, Wang J, Liu J, Mai X (2013) New clinical classification system for atlantoaxial dislocation. Orthopedics 36(1):e95-100
Yang SY, Boniello AJ, Poorman CE, Chang AL, Wang S, Passias PG (2014) A review of the diagnosis and treatment of atlantoaxial dislocations. Global Spine J 4(3):197–210
Behari S, Bhargava V, Nayak S, Kiran Kumar MV, Banerji D, Chhabra DK, Jain VK (2002) Congenital reducible atlantoaxial dislocation: classification and surgical considerations. Acta Neurochir (Wien) 144(11):1165–77
Yin QS, Wang JH (2015) Current trends in management of atlantoaxial dislocation. Orthop Surg 7(3):189–199
Liu T, Li F, Xiong W, Du X, Fang Z, Shang H, Chen A (2010) Video-assisted anterior transcervical approach for the reduction of irreducible atlantoaxial dislocation. Spine (Phila Pa 1976) 35(15):1495–501
Ren X, Gao F, Li S, Yang J, Xi Y (2019) Treatment of irreducible atlantoaxial dislocation using one-stage retropharyngeal release and posterior reduction. J Orthop Surg (Hong Kong) 27(3):2309499019870465
Kingdom TT, Nockels RP, Kaplan MJ (1995) Transoral-transpharyngeal approach to the craniocervical junction. Otolaryngol Head Neck Surg 113(4):393–400
Yin QS, Ai FZ, Zhang K, Mai XH, Xia H, Wu ZH (2010) Transoral atlantoaxial reduction plate internal fixation for the treatment of irreducible atlantoaxial dislocation: a 2- to 4-year follow-up. Orthop Surg 2(2):149–155
Xia H, Yin Q, Ai F, Ma X, Wang J, Wu Z, Zhang K, Liu J, Xu J (2014) Treatment of basilar invagination with atlantoaxial dislocation: atlantoaxial joint distraction and fixation with transoral atlantoaxial reduction plate (TARP) without odontoidectomy. Eur Spine J 23(8):1648–1655
Zou X, Ouyang B, Yang H, Wang B, Ge S, Chen Y, Ni L, Zhang S, Xia H, Yang J, Ma X (2020) Surgical treatment for basilar invagination with irreducible atlantoaxial dislocation: transoral atlantoaxial reduction plate fixation vs occipitocervical fixation. BMC Musculoskelet Disord 21(1):825
Yin Q, Ai F, Zhang K, Chang Y, Xia H, Wu Z, Quan R, Mai X, Liu J (2005) Irreducible anterior atlantoaxial dislocation: one-stage treatment with a transoral atlantoaxial reduction plate fixation and fusion. Report of 5 cases and review of the literature. Spine (Phila Pa 1976) 30(13):E375-81
Srivastava SK, Aggarwal RA, Nemade PS, Bhosale SK (2016) Single-stage anterior release and posterior instrumented fusion for irreducible atlantoaxial dislocation with basilar invagination. Spine J 16(1):1–9
Wang Q, Mao K, Wang C, Mei W (2017) Transoral atlantoaxial release and posterior reduction by occipitocervical plate fixation for the treatment of basilar invagination with irreducible atlantoaxial dislocation. J Neurol Surg A Cent Eur Neurosurg 78(4):313–320
Hao D, He B, Zheng Y, Zhang Z (2016) Single-stage anterior release and sequential posterior fusion for irreducible atlantoaxial dislocation. Clin Spine Surg 29(5):E240-5
Hao DJ, He BR, Wu QN (2009) One-stage anterior release and reduction with posterior fusion for treatment of irreducible atlantoaxial dislocation. Orthop Surg 1(4):305–10
Ma H, Dong L, Liu C, Yi P, Yang F, Tang X, Tan M (2016) Modified technique of transoral release in one-stage anterior release and posterior reduction for irreducible atlantoaxial dislocation. J Orthop Sci 21(1):7–12
Wang C, Yan M, Zhou HT, Wang SL, Dang GT (2006) Open reduction of irreducible atlantoaxial dislocation by transoral anterior atlantoaxial release and posterior internal fixation. Spine 31(11):E30606lan
Ma F, He H, Liao Y, Tang Q, Tang C, Yang S, Wang Q, Zhong D (2020) Classification of the facets of lateral atlantoaxial joints in patients with congenital atlantoaxial dislocation. Eur Spine J 29(11):2769–2777
Salunke P, Sharma M, Sodhi HB et al (2011) Congenital atlantoaxial dislocation: a dynamic process and role of facets in irreducibility[J]. J Neurosurg Spine 15(6):678–685
Yin YH, Yu XG, Zhou DB et al (2012) Three-dimensional configuration and morphometric analysis of the lateral atlantoaxial articulation in congenital anomaly with occipitalization of the atlas[J]. Spine (Phila Pa 1976) 37(3):E170–E173
Yin YH, Yu XG (2015) The severity of basilar invagination and atlantoaxial dislocation correlates with sagittal joint inclination, coronal joint inclination, and craniocervical tilt: a description of new indices for the craniovertebral junction[J]. Neurosurgery 76(2):E233–E235
Sarat Chandra P, Bajaj J, Singh PK, Garg K, Agarwal D (2019) Basilar invagination and atlantoaxial dislocation: reduction, deformity correction and realignment using the DCER (distraction, compression, extension, and reduction) technique with customized instrumentation and implants. Neurospine 16(2):231–250
Chandra PS, Prabhu M, Goyal N, Garg A, Chauhan A, Sharma BS (2015) Distraction, compression, extension, and reduction combined with joint remodelling and extra-articular distraction: description of 2 new modifications for its application in basilar invagination and atlantoaxial dislocation: prospective study in 79 cases. Neurosurgery 77(1):67–80 (discussion 80)
Laheri V, Chaudhary K, Rathod A, Bapat M (2015) Anterior transoral attlantoaxial release and posterior instrumented fusion for irreducible congenital basilar invagination. Eur spine J 24(12):2977–2985
Yuan SL, Xu HM, Fu LC, Cao J, Yang JK, Xi YM (2018) Sagittal atlantoaxial joint inclination and reduction index values for diagnosis and treatment of irreducible atlantoaxial dislocation. Indian J Orthop 52(2):190–195
Chandra PS, Goyal N, Chauhan A, Ansari A, Sharma BS, Garg A (2014) The severity of basilar invagination and atlantoaxial dislocation correlates with sagittal joint inclination, coronal joint inclination, and craniocervical tilt: a description of new indexes for the craniovertebral junction. Neurosurgery 10(Suppl 4):621–629
Hong Lee SW, Son BC et al (2008) Analysis of anatomical variations of bone and vascular structures around the posterior atlantal arch using three-dimensional computed tomography angiography [J]. J Neurosurg Spine 8(3):230–236
Xu S, Ruan S, Song X, Yu J, Xu J, Gong R (2018) Evaluation of vertebral artery anomaly in basilar invagination and prevention of vascular injury during surgical intervention: CTA features and analysis. Eur Spine J 27:1286lurnal
Yamazaki M, Okawa A, Furuya T, Sakuma T, Takahashi H, Kato K, Fujiyoshi T, Mannoji C, Takahashi K, Koda M (2012) Anomalous vertebral arteries in the extra- and intraosseous regions of the craniovertebral junction visualized by 3-dimensional computed tomographic angiography: analysis of 100 consecutive surgical cases and review of the literature. Spine 37:1389ure
Wang J, Xia H, Ying Q et al (2013) An anatomic consideration of C2 vertebrae artery groove variation for individual screw implantation in axis. Eur Spine J 22(4):154747 15
Yin Q, Xia H, Wu Z, Ma X, Ai F, Zhang K, Wang J, Zhang T, Bai Z, Wang Z (2016) Surgical site infections following the transoral approach: a review of 172 consecutive cases. Clin Spine Surg 29:E502SurgS
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Jianhua Wang, Hong Xia, Xiang yang Ma, Kai Zhang, SuoChao Fu, and Qiang Tu. The first draft of the manuscript was written by Jianhua Wang, Junjie Xu, HongLei Yi, and Changrong Zhu. And all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of General Military Hospital of Southern Theatre Command of People Liberation Army (date January 1/2018).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The authors affirm that this manuscript did not contain any individual person’s data or images which need to provide informed consent for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, J., Xia, H., Ma, X.y. et al. Treatment of irreducible atlantoaxial dislocation by bony deformity osteotomy, remodeling, releasing, and plate fixating through transoral approach. International Orthopaedics (SICOT) 47, 209–224 (2023). https://doi.org/10.1007/s00264-022-05604-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05604-w