Abstract
Purpose
To evaluate the efficacy and safety of negative pressure wound therapy (NPWT) for post-operative deep surgical site infection (SSI) after posterior instrumented spinal surgery.
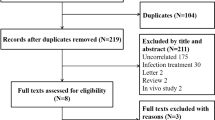
Methods
We retrospectively compared the clinical outcomes of NPWT with standard debridement for deep SSI after posterior instrumented spinal surgery from 2012 to 2020 in our department. The primary outcomes were peri-operative characteristics including positive organism results, duration of fever, and visual analogue scale (VAS) pain scores three days after re-operation. The secondary outcomes were post-operative characteristics including implant infection recurrence, implant retention rate, duration of hospitalization, and VAS at discharge. Pearson's chi-squared analysis (categorical) and Student’s t test (continuous) were used to determine the differences.
Results
Thirty-four patients were included, of which 19 underwent NPWT, and 15 underwent standard debridement. Patients in the NPWT group all significantly improved primary outcomes including duration of fever after re-operation (0.95 ± 1.13 vs 4.07 ± 5.35, P = 0.001), positive organism results (14 of 19 vs 2 of 15, P < 0.01), and VAS at 3 days after re-operation (2.58 ± 0.69 vs 3.40 ± 1.06, P < 0.05). Patients in NPWT group exhibited significant decrease in implant infection recurrence (0 of 19 vs 5 of 15, P < 0.01), implant retention rate (19 of 19 vs 10 of 15, P < 0.01), duration of hospitalization (27.74 ± 10.95 vs 37.67 ± 13.67, P < 0.01).
Conclusions
NPWT is a feasible and safe treatment option for deep SSI after posterior instrumented spinal surgery.


Similar content being viewed by others
Data availability
All data analyzed during this study are included in the manuscript. The datasets used in this article are available from the corresponding author (Z.Q.C.) on reasonable request.
References
Abdul-Jabbar A, Takemoto S, Weber MH, Hu SS, Mummaneni PV, Deviren V, Ames CP, Chou D, Weinstein PR, Burch S, Berven SH (2012) Surgical site infection in spinal surgery: description of surgical and patient-based risk factors for postoperative infection using administrative claims data. Spine (Phila Pa 1976) 37:1340–1345. https://doi.org/10.1097/BRS.0b013e318246a53a
Shoji H, Hirano T, Watanabe K, Ohashi M, Mizouchi T, Endo N (2018) Risk factors for surgical site infection following spinal instrumentation surgery. J Orthop Sci 23:449–454. https://doi.org/10.1016/j.jos.2018.02.008
Edwards JR, Peterson KD, Mu Y, Banerjee S, Allen-Bridson K, Morrell G, Dudeck MA, Pollock DA, Horan TC (2009) National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control 37:783–805. https://doi.org/10.1016/j.ajic.2009.10.001
Anderson DJ, Kaye KS, Classen D, Arias KM, Podgorny K, Burstin H, Calfee DP, Coffin SE, Dubberke ER, Fraser V, Gerding DN, Griffin FA, Gross P, Klompas M, Lo E, Marschall J, Mermel LA, Nicolle L, Pegues DA, Perl TM, Saint S, Salgado CD, Weinstein RA, Wise R, Yokoe DS (2008) Strategies to prevent surgical site infections in acute care hospitals. Infect Control Hosp Epidemiol 29(Suppl 1):S51-61. https://doi.org/10.1086/591064
de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, Vaughn BB (2009) Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control 37:387–397. https://doi.org/10.1016/j.ajic.2008.12.010
Fei Q, Li J, Lin J, Li D, Wang B, Meng H, Wang Q, Su N, Yang Y (2016) Risk factors for surgical site infection after spinal surgery: a meta-analysis. World Neurosurg 95:507–515. https://doi.org/10.1016/j.wneu.2015.05.059
Pesenti S, Pannu T, Andres-Bergos J, Lafage R, Smith JS, Glassman S, de Kleuver M, Pellise F, Schwab F, Lafage V, Scoliosis Research S (2018) What are the risk factors for surgical site infection after spinal fusion? A meta-analysis. Eur Spine J 27:2469–2480. https://doi.org/10.1007/s00586-018-5733-7
Peng XQ, Sun CG, Fei ZG, Zhou QJ (2019) Risk factors for surgical site infection after spinal surgery: a systematic review and meta-analysis based on twenty-seven studies. World Neurosurg 123:e318–e329. https://doi.org/10.1016/j.wneu.2018.11.158
Mok JM, Guillaume TJ, Talu U, Berven SH, Deviren V, Kroeber M, Bradford DS, Hu SS (2009) Clinical outcome of deep wound infection after instrumented posterior spinal fusion: a matched cohort analysis. Spine (Phila Pa 1976) 34:578–583. https://doi.org/10.1097/BRS.0b013e31819a827c
Garner BH, Anderson DJ (2016) Surgical site infections: an update. Infect Dis Clin North Am 30:909–929. https://doi.org/10.1016/j.idc.2016.07.010
Jones GA, Butler J, Lieberman I, Schlenk R (2007) Negative-pressure wound therapy in the treatment of complex postoperative spinal wound infections: complications and lessons learned using vacuum-assisted closure. J Neurosurg Spine 6:407–411. https://doi.org/10.3171/spi.2007.6.5.407
Ploumis A, Mehbod AA, Dressel TD, Dykes DC, Transfeldt EE, Lonstein JE (2008) Therapy of spinal wound infections using vacuum-assisted wound closure: risk factors leading to resistance to treatment. J Spinal Disord Tech 21:320–323. https://doi.org/10.1097/BSD.0b013e318141f99d
Rohmiller MT, Akbarnia BA, Raiszadeh K, Raiszadeh K, Canale S (2010) Closed suction irrigation for the treatment of postoperative wound infections following posterior spinal fusion and instrumentation. Spine (Phila Pa 1976) 35:642–646. https://doi.org/10.1097/BRS.0b013e3181b616eb
Weinstein MA, McCabe JP, Cammisa FP Jr (2000) Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. J Spinal Disord 13:422–426. https://doi.org/10.1097/00002517-200010000-00009
Zeng J, Sun X, Sun Z, Guan J, Han C, Zhao X, Zhang P, Xie Y, Zhao J (2019) Negative pressure wound therapy versus closed suction irrigation system in the treatment of deep surgical site infection after lumbar surgery. World Neurosurg 127:e389–e395. https://doi.org/10.1016/j.wneu.2019.03.130
Akhter AS, McGahan BG, Close L, Dornbos D 3rd, Toop N, Thomas NR, Christ E, Dahdaleh NS, Grossbach AJ (2021) Negative pressure wound therapy in spinal fusion patients. Int Wound J 18:158–163. https://doi.org/10.1111/iwj.13507
Lian XF, Xu JG, Zeng BF, Liu XK, Li H, Qiu ML, Yang EZ (2014) Continuous irrigation and drainage for early postoperative deep wound infection after posterior instrumented spinal fusion. J Spinal Disord Tech 27:E315-317. https://doi.org/10.1097/BSD.0000000000000122
Shah A, Sumpio BJ, Tsay C, Swallow M, Dash B, Thorn SL, Sinusas AJ, Koo A, Hsia HC, Au A (2019) Incisional negative pressure wound therapy augments perfusion and improves wound healing in a swine model pilot study. Ann Plast Surg 82:S222–S227. https://doi.org/10.1097/SAP.0000000000001842
Dyck BA, Bailey CS, Steyn C, Petrakis J, Urquhart JC, Raj R, Rasoulinejad P (2019) Use of incisional vacuum-assisted closure in the prevention of postoperative infection in high-risk patients who underwent spine surgery: a proof-of-concept study. J Neurosurg Spine 31:430–439. https://doi.org/10.3171/2019.2.SPINE18947
Bible JE, Biswas D, Devin CJ (2011) Postoperative infections of the spine. Am J Orthop (Belle Mead NJ) 40:E264-271
Meredith DS, Kepler CK, Huang RC, Brause BD, Boachie-Adjei O (2012) Postoperative infections of the lumbar spine: presentation and management. Int Orthop 36:439–444. https://doi.org/10.1007/s00264-011-1427-z
Deng H, Chan AK, Ammanuel S, Chan AY, Oh T, Skrehot HC, Edwards S, Kondapavulur S, Nichols AD, Liu C, Yue JK, Dhall SS, Clark AJ, Chou D, Ames CP, Mummaneni PV (2019) Risk factors for deep surgical site infection following thoracolumbar spinal surgery. J Neurosurg Spine 32:292–301. https://doi.org/10.3171/2019.8.SPINE19479
Barker FG 2nd (2002) Efficacy of prophylactic antibiotic therapy in spinal surgery: a meta-analysis. Neurosurgery 51:391–400 (discussion 400-391)
Brown MD, Brookfield KF (2004) A randomized study of closed wound suction drainage for extensive lumbar spine surgery. Spine (Phila Pa 1976) 29:1066–1068. https://doi.org/10.1097/00007632-200405150-00003
De la Garza-Ramos R, Abt NB, Kerezoudis P, McCutcheon BA, Bydon A, Gokaslan Z, Bydon M (2016) Deep-wound and organ-space infection after surgery for degenerative spine disease: an analysis from 2006 to 2012. Neurol Res 38:117–123. https://doi.org/10.1080/01616412.2016.1138669
Canavese F, Gupta S, Krajbich JI, Emara KM (2008) Vacuum-assisted closure for deep infection after spinal instrumentation for scoliosis. J Bone Joint Surg Br 90:377–381. https://doi.org/10.1302/0301-620X.90B3.19890
Labler L, Keel M, Trentz O, Heinzelmann M (2006) Wound conditioning by vacuum assisted closure (V.A.C.) in postoperative infections after dorsal spine surgery. Eur Spine J 15:1388–1396. https://doi.org/10.1007/s00586-006-0164-2
Mylona E, Samarkos M, Kakalou E, Fanourgiakis P, Skoutelis A (2009) Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin Arthritis Rheum 39:10–17. https://doi.org/10.1016/j.semarthrit.2008.03.002
Mendonca DA, Papini R, Price PE (2006) Negative-pressure wound therapy: a snapshot of the evidence. Int Wound J 3:261–271. https://doi.org/10.1111/j.1742-481X.2006.00266.x
Vuerstaek JD, Vainas T, Wuite J, Nelemans P, Neumann MH, Veraart JC (2006) State-of-the-art treatment of chronic leg ulcers: a randomized controlled trial comparing vacuum-assisted closure (V.A.C.) with modern wound dressings. J Vasc Surg 44:1029–1037. https://doi.org/10.1016/j.jvs.2006.07.030 (discussion 1038)
Blumberg TJ, Woelber E, Bellabarba C, Bransford R, Spina N (2018) Predictors of increased cost and length of stay in the treatment of postoperative spine surgical site infection. Spine J 18:300–306. https://doi.org/10.1016/j.spinee.2017.07.173
Acknowledgements
We thank Associate Professor Li Jianhua for his help with the English writing of our manuscript.
Author information
Authors and Affiliations
Contributions
J.M.W. and Z.Q.C. made substantial contributions to acquisition, analysis, and interpretation of data. Z.Q.C. was responsible for the conception and design of the study and the drafting and writing of this manuscript. Y.Y., W.Q.X., and J.M.W. were a surgical assistant. All authors confirm the authenticity of all the raw data.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been approved by the 960th hospital of PLA. Each author certifies that all investigations were conducted in accordance with ethical principles. The participant involved in the study gave their informed consent and signed an informed consent form.
Consent for publication
Written consent to publish this article was obtained from study participants. Proof of consent to publish from study participants can be requested at any time.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, J., Yang, Y., Xing, W. et al. Safety and efficacy of negative pressure wound therapy in treating deep surgical site infection after lumbar surgery. International Orthopaedics (SICOT) 46, 2629–2635 (2022). https://doi.org/10.1007/s00264-022-05531-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05531-w