Abstract
Purpose
We conducted a comprehensive analysis of possible perioperative complications following all-inside anterior cruciate ligament reconstruction (ACLR). Additional techniques and tips are proposed to prevent and manage complications.
Methods
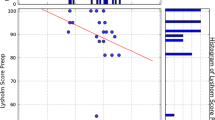
Complications following all-inside ACLR performed between December 2015 and December 2020 were retrospectively analysed. Altogether, 348 operations were performed and 275 patients were enrolled with a minimum 12-month follow-up period. Only semitendinosus autograft was utilised in most patients, and semitendinosus–gracilis autograft and allograft were used in five and 31 patients, respectively. Simultaneous meniscal repair, partial meniscectomy, and chondral surgery were performed in 29.5%, 21.1%, and 4.4% of patients, respectively. Complications were observed based on the patient’s clinical condition, plain film, and magnetic resonance imaging. Clinical outcomes were assessed pre-operatively and at 12 months post-operatively, using the International Knee Documentation Committee form, Lysholm and Tegner activity scores, and KT1000 side-to-side difference.
Results
Intraoperative and post-operative complications developed in 65 patients (23.6%). The most common complication was cortical button malposition on the femoral side (19.3%). Intra-operative breakage of the retrograde drill was found in two cases (0.73%), with three cases (1.1%) of over-drilling with destruction of the outer cortex. Post-operatively, four (1.5%), 13 (4.7%), and 16 (5.8%) cases of infection, full-thickness re-rupture, and loss of extension, respectively, were recorded. Functional outcome scales showed significant post-operative improvement.
Conclusion
Cortical button malposition was the most common but easily preventable complication. All-inside ACLR could be safe and promising after the suggested additional operative techniques and proper perioperative management which decrease complication rates and improve favourable outcomes.





Similar content being viewed by others
References
Robin BN, Jani SS, Marvil SC, Reid JB, Schillhammer CK, Lubowitz JH (2015) Advantages and disadvantages of transtibial, anteromedial portal, and outside-in femoral tunnel drilling in single-bundle anterior cruciate ligament reconstruction: a systematic review. Arthroscopy 31:1412–1417. https://doi.org/10.1016/j.arthro.2015.01.018
Morgan CD (1995) The all-inside ACL reconstruction. In: Morgan CD (ed.) Operative technique manual. Arthrex, Naples.
Lubowitz JH, Schwartzberg R, Smith P (2013) Randomized controlled trial comparing all-inside anterior cruciate ligament reconstruction technique with anterior cruciate ligament reconstruction with a full tibial tunnel. Arthroscopy 29:1195–1200. https://doi.org/10.1016/j.arthro.2013.04.009
Schurz M, Tiefenboeck TM, Winnisch M et al (2016) Clinical and functional outcome of all-inside anterior cruciate ligament reconstruction at a minimum of 2 years’ follow-up. Arthroscopy 32:332–337. https://doi.org/10.1016/j.arthro.2015.08.014
Mayr R, Smekal V, Koidl C et al (2020) ACL reconstruction with adjustable-length loop cortical button fixation results in less tibial tunnel widening compared with interference screw fixation. Knee Surg Sports Traumatol Arthrosc 28:1036–1044. https://doi.org/10.1007/s00167-019-05642-9
Yasen SK, Borton ZM, Eyre-Brook AI et al (2017) Clinical outcomes of anatomic, all-inside, anterior cruciate ligament (ACL) reconstruction. Knee 24:55–62. https://doi.org/10.1016/j.knee.2016.09.007
Lubowitz JH, Schwartzberg R, Smith P (2015) Cortical suspensory button versus aperture interference screw fixation for knee anterior cruciate ligament soft-tissue allograft: a prospective, randomized controlled trial. Arthroscopy 31:1733–1739. https://doi.org/10.1016/j.arthro.2015.03.006
de Sa D, Shanmugaraj A, Weidman M et al (2018) All-inside anterior cruciate ligament reconstruction—a systematic review of techniques, outcomes, and complications. J Knee Surg 31:895–904. https://doi.org/10.1055/s-0038-1627446
Connaughton AJ, Geeslin AG, Uggen CW (2017) All-inside ACL reconstruction: how does it compare to standard ACL reconstruction techniques? J Orthop 14:241–246. https://doi.org/10.1016/j.jor.2017.03.002
Fu CW, Chen WC, Lu YC (2020) Is all-inside with suspensory cortical button fixation a superior technique for anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. BMC Musculoskelet Disord 21:445. https://doi.org/10.1186/s12891-020-03471-3
Zamarra G, Fisher MB, Woo SL, Cerulli G (2010) Biomechanical evaluation of using one hamstrings tendon for ACL reconstruction: a human cadaveric study. Knee Surg Sports Traumatol Arthrosc 18:11–19. https://doi.org/10.1007/s00167-009-0911-0
Lubowitz JH, Ahmad CS, Anderson K (2011) All-inside anterior cruciate ligament graft-link technique: second-generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy 27:717–727. https://doi.org/10.1016/j.arthro.2011.02.008
Papaloucas N (2018) All-inside technique for ACL-reconstruction using a FlipCutter® and the TightRope® system. Surg Technol Int 32:337–345
Desai VS, Anderson GR, Wu IT et al (2019) Anterior cruciate ligament reconstruction with hamstring autograft: a matched cohort comparison of the all-inside and complete tibial tunnel techniques. Orthop J Sports Med 7:2325967118820297. https://doi.org/10.1177/2325967118820297
Kouloumentas P, Kavroudakis E, Charalampidis E, Kavroudakis D, Triantafyllopoulos GK (2019) Superior knee flexor strength at 2 years with all-inside short-graft anterior cruciate ligament reconstruction vs a conventional hamstring technique. Knee Surg Sports Traumatol Arthrosc 27:3592–3598. https://doi.org/10.1007/s00167-019-05456-9
Kawaguchi K, Kuribayashi S, Nakayama S, Nakazato K, Fukubayashi T, Okinaga S (2016) Lateral knee pain after outside-in anatomic double-bundle anterior cruciate ligament reconstruction using the TightRope RT. Knee Surg Relat Res 28:83–87. https://doi.org/10.5792/ksrr.2016.28.1.83
Wilson AJ, Yasen SK, Nancoo T, Stannard R, Smith JO, Logan JS (2013) Anatomic all-inside anterior cruciate ligament reconstruction using the translateral technique. Arthrosc Tech 2:e99–e104. https://doi.org/10.1016/j.eats.2012.12.002
Osti M, Krawinkel A, Ostermann M, Hoffelner T, Benedetto KP (2015) Femoral and tibial graft tunnel parameters after transtibial, anteromedial portal, and outside-in single-bundle anterior cruciate ligament reconstruction. Am J Sports Med 43:2250–2258. https://doi.org/10.1177/0363546515590221
Lubowitz JH, Konicek J (2010) Anterior cruciate ligament femoral tunnel length: cadaveric analysis comparing anteromedial portal versus outside-in technique. Arthroscopy 26:1357–1362. https://doi.org/10.1016/j.arthro.2010.02.014
Barbosa NC, Guerra-Pinto F, Cabeleira C, Beja da Costa P (2017) Hamstring graft biological preparation for anterior cruciate ligament reconstruction. Arthrosc Tech 6:e245–e248. https://doi.org/10.1016/j.eats.2016.09.031
Smith PA, Stannard JP, Pfeiffer FM, Kuroki K, Bozynski CC, Cook JL (2016) Suspensory versus interference screw fixation for arthroscopic anterior cruciate ligament reconstruction in a translational large-animal model. Arthroscopy 32:1086–1097. https://doi.org/10.1016/j.arthro.2015.11.026
Kang SG, Lee YS (2017) Arthroscopic control for safe and secure seating of suspensory devices for femoral fixation in anterior cruciate ligament reconstruction using three different techniques. Knee Surg Relat Res 29:33–38. https://doi.org/10.5792/ksrr.16.053
Mae T, Kuroda S, Matsumoto N et al (2011) Migration of EndoButton after anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy 27:1528–1535. https://doi.org/10.1016/j.arthro.2011.06.024
O’Brien DF, Fones L, Stoj V, Edgar C, Coyner K, Arciero RA (2021) Confirming proper button deployment of suspensory fixation during ACL reconstruction. Orthop J Sports Med 9:2325967120974349. https://doi.org/10.1177/2325967120974349
Mistovich RJ, O’Toole PO, Ganley TJ (2014) Pediatric anterior cruciate ligament femoral fixation: the trans-iliotibial band endoscopic portal for direct visualization of ideal button placement. Arthrosc Tech 3:e335–e338. https://doi.org/10.1016/j.eats.2014.01.015
Nag HL, Gupta H (2012) Seating of TightRope RT button under direct arthroscopic visualization in anterior cruciate ligament reconstruction to prevent potential complications. Arthrosc Tech 1:e83–e85. https://doi.org/10.1016/j.eats.2012.03.003
Lubowitz JH, Akhavan S, Waterman BR, Aalami-Harandi A, Konicek J (2013) Technique for creating the anterior cruciate ligament femoral socket: optimizing femoral footprint anatomic restoration using outside-in drilling. Arthroscopy 29:522–528. https://doi.org/10.1016/j.arthro.2012.10.007
Herbort M, Heletta S, Raschke MJ et al (2012) Accidental perforation of the lateral femoral cortex in ACL reconstruction: an investigation of mechanical properties of different fixation techniques. Arthroscopy 28:382–389. https://doi.org/10.1016/j.arthro.2011.10.028
Mitchell JJ, Chahla J, Dean CS et al (2016) Posterior wall blowout during anterior cruciate ligament reconstruction: suspensory cortical fixation with a screw and washer post. Arthrosc Tech 5:e551–e555. https://doi.org/10.1016/j.eats.2016.02.003
Noll S, Garrison JC, Bothwell J, Conway JE (2015) Knee extension range of motion at 4 weeks is related to knee extension loss at 12 weeks after anterior cruciate ligament reconstruction. Orthop J Sports Med 3:2325967115583632. https://doi.org/10.1177/2325967115583632
Mauro CS, Irrgang JJ, Williams BA, Harner CD (2008) Loss of extension following anterior cruciate ligament reconstruction: analysis of incidence and etiology using IKDC criteria. Arthroscopy 24:146–153. https://doi.org/10.1016/j.arthro.2007.08.026
Panisset JC, Pailhé R, Schlatterer B et al (2017) Short-term complications in intra- and extra-articular anterior cruciate ligament reconstruction. Comparison with the literature on isolated intra-articular reconstruction. A multicenter study by the French Arthroscopy Society. Orthop Traumatol Surg Res 103:S231–S236. https://doi.org/10.1016/j.otsr.2017.09.006
Nauth A (2012) Gilbart MK Knee stiffness after ACL reconstruction. Techniques in Knee Surgery 11:26–33
Robertson GAJ, Coleman SGS, Keating JF (2009) Knee stiffness following anterior cruciate ligament reconstruction: the incidence and associated factors of knee stiffness following anterior cruciate ligament reconstruction. Knee 16:245–247. https://doi.org/10.1016/j.knee.2008.12.014
Pinto FG, Thaunat M, Daggett M et al (2017) Hamstring contracture after ACL reconstruction is associated with an increased risk of cyclops syndrome. Orthop J Sports Med 5:2325967116684121. https://doi.org/10.1177/2325967116684121
Rice DA, McNair PJ (2010) Quadriceps arthrogenic muscle inhibition: neural mechanisms and treatment perspectives. Semin Arthritis Rheum 40:250–266. https://doi.org/10.1016/j.semarthrit.2009.10.001
Delaloye JR, Murar J, Sánchez MG et al (2018) How to rapidly abolish knee extension deficit after injury or surgery: a practice-changing video pearl from the Scientific anterior cruciate ligament Network International (SANTI) Study Group. Arthrosc Tech 7:e601–e605. https://doi.org/10.1016/j.eats.2018.02.006
Acknowledgements
The authors wish to thank the staff members of the Orthopaedic Department at the MacKay Memorial Hospital for their expert assistance with data collection and professional advice.
Author information
Authors and Affiliations
Contributions
Conceptualization: Yung-Chang Lu, Tsung-Yu Lin; methodology: Tsung-Yu Lin, Cheng-Chun Chung; formal analysis and investigation: Tsung-Yu Lin, Cheng-Chun Chung; writing—original draft preparation: Yung-Chang Lu, Tsung-Yu Lin, Cheng-Chun Chung; writing—review and editing: Tsung-Yu Lin, Cheng-Chun Chung, Wei-Cheng Chen, Che-Wei Su, Hsu-Wei Fang, Yung-Chang Lu; resources: Tsung-Yu Lin, Wei-Cheng Chen, Che-Wei Su, MD, Hsu-Wei Fang, Yung-Chang Lu; supervision: Yung-Chang Lu. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval was obtained from the ethics committee of our institution.
IRB number: 21MMHIS217e.
MacKay Memorial Hospital Institutional Review Board.
All patients provided informed consent, including for publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, TY., Chung, CC., Chen, WC. et al. Complications following all-inside anterior cruciate ligament reconstruction. International Orthopaedics (SICOT) 46, 2569–2576 (2022). https://doi.org/10.1007/s00264-022-05515-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05515-w