Abstract
Purpose
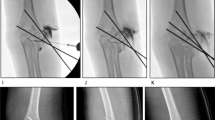
The management of type 3 lateral condyle fractures (LCFs) remains controversial. The main goal of this study was to evaluate the feasibility of closed reduction and percutaneous pinning (CRPP) in patients with type 3 LCFs and to assess the outcome of such injuries according to the type of treatment, CRPP, or open reduction and internal fixation (ORIF).
Methods
This is a retrospective review of prospectively enrolled children with type 3 LCF managed by CRPP or ORIF between 2018 and 2021. All patients were followed for at least 12 months. Patients were divided into two groups according to the type of treatment, CRPP or ORIF. Demographic characteristics were recorded for all patients.
Standard radiographs were used to identify, evaluate, and classify each fracture and to detect the presence of other concomitant bone lesions. The clinical outcome was assessed according to the Hardacre et al. criteria.
Results
Seventy-eight children with type 3 LCF were included; 42 were treated by CRPP (53.8%) and 36 by ORIF (46.2%); the mean follow-up time was 17.7 months (range, 12.3–40.9). The baseline characteristics did not differ between the two groups of patients. Overall, successful CRPP could be achieved in 39 out of 42 patients (92.9%). The mean surgical time was 63.4 and 84.5 min in patients treated by CRPP and ORIF, respectively (p = 0.01). Fluoroscopy time was significantly shorter in patients managed by ORIF than in those treated by CRPP (12 versus 40 s, respectively; p < 0.001).
Clinical outcome according to the Hardacre et al. criteria was excellent in 37 out of 39 (94.4%) and in 35 out of 36 patients (97.2%) treated by CRPP and ORIF, respectively (p = 0.09).
Conclusions
CRPP management of paediatric type 3 LCF has clinical and radiographic outcomes similar to ORIF; if satisfactory reduction cannot be achieved by CRPP, conversion to ORIF should be considered.



Similar content being viewed by others
Data availability
The data will be available upon reasonable request.
References
Wirmer J, Kruppa C, Fitze G (2012) Operative treatment of lateral humeral condyle fractures in children. Eur J Pediatr Surg 22:289–294. https://doi.org/10.1055/s-0032-1308709
Li WC, Xu RJ (2012) Comparison of Kirschner wires and AO cannulated screw internal fixation for displaced lateral humeral condyle fracture in children. Int Orthop 36:1261–1266. https://doi.org/10.1007/s00264-011-1452-y
Landin LA, Danielsson LG (1986) Elbow fractures in children. An epidemiological analysis of 589 cases. Acta Orthop Scand 57:309–312. https://doi.org/10.3109/17453678608994398
Canavese F, Marengo L, Tiris A, Mansour M, Rousset M, Samba A, Andreacchio A, Dimeglio A (2017) Radiological, clinical and functional evaluation using the quick disabilities of the arm, shoulder and hand questionnaire of children with medial epicondyle fractures treated surgically. Int Orthop 41:1447–1452. https://doi.org/10.1007/s00264-017-3442-1
Zorrilla SdNJ, Prada-Cañizares A, Marti-Ciruelos R, Pretell-Mazzini J (2015) Supracondylar humeral fractures in children: current concepts for management and prognosis. Int Orthop 39:2287–2296. https://doi.org/10.1007/s00264-015-2975-4
Foster DE, Sullivan JA, Gross RH (1985) Lateral humeral condylar fractures in children. J Pediatr Orthop 5:16–22. https://doi.org/10.1097/01241398-198501000-00004
Song KS, Kang CH, Min BW, Bae KC, Cho CH, Lee JH (2008) Closed reduction and internal fixation of displaced unstable lateral condylar fractures of the humerus in children. J Bone Joint Surg Am 90:2673–2681. https://doi.org/10.2106/jbjs.G.01227
Silva M, Cooper SD (2015) Closed reduction and percutaneous pinning of displaced pediatric lateral condyle fractures of the humerus: a cohort study. J Pediatr Orthop 35:661–665. https://doi.org/10.1097/bpo.0000000000000376
Pennock AT, Salgueiro L, Upasani VV, Bastrom TP, Newton PO, Yaszay B (2016) Closed reduction and percutaneous pinning versus open reduction and internal fixation for type II lateral condyle humerus fractures in children displaced >2 mm. J Pediatr Orthop 36:780–786. https://doi.org/10.1097/bpo.0000000000000570
Gendi K, Livermore A, Browne J, Machurick M, Halanski MA, Noonan KJ (2019) Open Vs. Closed reduction in type 2 lateral condyle fractures. Iowa Orthop J 39:51–55
Shaerf DA, Vanhegan IS, Dattani R (2018) Diagnosis, management and complications of distal humerus lateral condyle fractures in children. Shoulder Elbow 10:114–120. https://doi.org/10.1177/1758573217701107
Song KS, Shin YW, Oh CW, Bae KC, Cho CH (2010) Closed reduction and internal fixation of completely displaced and rotated lateral condyle fractures of the humerus in children. J Orthop Trauma 24:434–438. https://doi.org/10.1097/BOT.0b013e3181de014f
Xie LW, Wang J, Deng ZQ, Zhao RH, Chen W, Kang C, Ye JJ, Liu X, Zhou Y, Shen H (2020) Treatment of pediatric lateral condylar humerus fractures with closed reduction and percutaneous pinning. BMC Musculoskelet Disord 21:707. https://doi.org/10.1186/s12891-020-03738-9
Xie LW, Deng ZQ, Zhao RH, Wang J, Liu X, Zhou Y, Zhang H (2021) Closed reduction and percutaneous pinning vs open reduction and internal fixation in pediatric lateral condylar humerus fractures displaced by > 4 mm: an observational cross-sectional study. BMC Muscoloskelet Disord 22(1):985. https://doi.org/10.1186/s12891-021-04880-8
Hardacre JA, Nahigian SH, Froimson AI, Brown JE (1971) Fractures of the lateral condyle of the humerus in children. J Bone Joint Surg Am 53:1083–1095
Jakob R, Fowles JV, Rang M, Kassab MT (1975) Observations concerning fractures of the lateral humeral condyle in children. J Bone Joint Surg Br 57:430–436
Sullivan JA (2006) Fractures of the lateral condyle of the humerus. J Am Acad Orthop Surg 14:58–62. https://doi.org/10.5435/00124635-200601000-00010
Hausman MR, Qureshi S, Goldstein R, Langford J, Klug RA, Radomisli TE, Parsons BO (2007) Arthroscopically-assisted treatment of pediatric lateral humeral condyle fractures. J Pediatr Orthop 27:739–742. https://doi.org/10.1097/BPO.0b013e3181558ac5
Badelon O, Bensahel H, Mazda K, Vie P (1988) Lateral humeral condylar fractures in children: a report of 47 cases. J Pediatr Orthop 8:31–34. https://doi.org/10.1097/01241398-198801000-00008
Launay F, Leet AI, Jacopin S, Jouve JL, Bollini G, Sponseller PD (2004) Lateral humeral condyle fractures in children: a comparison of two approaches to treatment. J Pediatr Orthop 24:385–391
Pribaz JR, Bernthal NM, Wong TC, Silva M (2012) Lateral spurring (overgrowth) after pediatric lateral condyle fractures. J Pediatr Orthop 32:456–460. https://doi.org/10.1097/BPO.0b013e318259ff63
Koh KH, Seo SW, Kim KM, Shim JS (2010) Clinical and radiographic results of lateral condylar fracture of distal humerus in children. J Pediatr Orthop 30:425–429. https://doi.org/10.1097/BPO.0b013e3181df1578
Skak SV, Olsen SD, Smaabrekke A (2001) Deformity after fracture of the lateral humeral condyle in children. J Pediatr Orthop B 10:142–152
Author information
Authors and Affiliations
Contributions
Yanhan Liu: study design; acquisition of data, analysis of data, interpretation of data, drafting of the work, final approval of the version to be published.
Weizhe Shi: acquisition of data, final approval of the version to be published.
Hai Zhao: acquisition of data, final approval of the version to be published.
Yiqiang Li: acquisition of data, statistical analysis, final approval of the version to be published.
Jingchun Li: acquisition of data, final approval of the version to be published.
Fuxin Xun: acquisition of data, stastistical analysis, final approval of the version to be published.
Federico Canavese: study design; analysis of data, interpretation of data, drafting of the work, final approval of the version to be published.
Hongwen Xu: interpretation of data, final approval of the version to be published.
All the authors contributed towards the literature search, critical review, data analysis, and manuscript preparation.
Corresponding author
Ethics declarations
Ethics approval
The Medical Ethics Committee of Guangzhou Women and Children’s Medical Center approved this retrospective review of prospectively enrolled patients. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from the parents.
Consent for publication
All authors listed have approved this manuscript. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, Y., Shi, W., Zhao, H. et al. Closed reduction and percutaneous pinning versus open reduction and internal fixation for Jakob type 3 lateral condyle fractures in children. International Orthopaedics (SICOT) 46, 2291–2297 (2022). https://doi.org/10.1007/s00264-022-05476-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05476-0