Abstract
Purpose
The aim of this study was to assess the difference between flexion and extension contact forces—gap balance—after Oxford mobile-bearing medial unicompartmental knee arthroplasty (UKA) performed by surgeons with varying levels of experience.
Methods
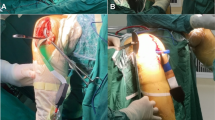
Surgeons in a training programme performed UKAs on fresh frozen cadaveric specimens (n = 60). Contact force in the medial compartment of the knee was measured after UKA during extension and flexion using a force sensor, and values were clustered using an unsupervised machine learning (k-means algorithm). Univariate analysis was performed with general linear regression models to identify the explanatory variable.
Results
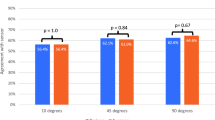
The level of experience was predictive of gap balance; surgeons were clustered into beginner, mid-level and experienced groups. Experienced surgeons’ mean difference between flexion and extension contact force was 83 N, which was significantly lower (p < 0.05) than that achieved by mid-level (215 N) or beginner (346 N) surgeons.
Conclusion
We found that the lowest mean difference between flexion and extension contact force after UKA was 83 N, which was achieved by surgeons with the most experience; this value can be considered the optimal value. Beginner and mid-level surgeons achieved values that were significantly lower. This study also demonstrates that machine learning can be used in combination with sensor technology for improving gap balancing judgement in UKA.



Similar content being viewed by others
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
Code availability
The software and custom code of the current study are available from the corresponding author and author Chen Yang on reasonable request.
References
Arias-de la Torre J, Valderas JM, Evans JP, Martín V, Molina AJ, Muñoz L, Pons-Cabrafiga M, Espallargues M (2019) Differences in risk of revision and mortality between total and unicompartmental knee arthroplasty. The influence of hospital volume. J Arthroplasty 34:865–871
Henkel C, Mikkelsen M, Pedersen AB, Rasmussen LE, Gromov K, Price A, Troelsen A (2019) Medial unicompartmental knee arthroplasty: increasingly uniform patient demographics despite differences in surgical volume and usage-a descriptive study of 8,501 cases from the Danish Knee Arthroplasty Registry. Acta Orthop 90:354–359
Mohammad HR, Matharu GS, Judge A, Murray DW (2020) The effect of surgeon caseload on the relative revision rate of cemented and cementless unicompartmental knee replacements: an analysis from the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. J Bone Joint Surg Am 102:644–653
Hamilton TW, Rizkalla JM, Kontochristos L, Marks BE, Mellon SJ, Dodd CAF, Pandit HG, Murray DW (2017) The interaction of caseload and usage in determining outcomes of unicompartmental knee arthroplasty: a meta-analysis. J Arthroplasty 32:3228–3237
Liddle AD, Pandit H, Judge A, Murray DW (2016) Effect of surgical caseload on revision rate following total and unicompartmental knee replacement. J Bone Joint Surg Am 98:1–8
Schraknepper J, Dimitriou D, Helmy N, Hasler J, Radzanowski S, Flury A (2020) Influence of patient selection, component positioning and surgeon’s caseload on the outcome of unicompartmental knee arthroplasty. Arch Orthop Trauma Surg 140:807–813
Hamilton WG, Ammeen D, Engh CA Jr, Engh GA (2010) Learning curve with minimally invasive unicompartmental knee arthroplasty. J Arthroplasty 25:735–740
Bae JH, Kim JG, Lee SY, Lim HC, In Y, Lee S, Ji JH, Lee JH, Kim JM, Kim KI (2020) Epidemiology of bearing dislocations after mobile-bearing unicompartmental knee arthroplasty: multicenter analysis of 67 bearing dislocations. J Arthroplasty 35:265–271
Sun X, Liu P, Lu F, Wang W, Guo W, Zhang Q (2021) Bearing dislocation of mobile bearing unicompartmental knee arthroplasty in East Asian countries: a systematic review with meta-analysis. J Orthop Surg Res 16:28
Ro KH, Heo JW, Lee DH (2018) Bearing dislocation and progression of osteoarthritis after mobile-bearing unicompartmental knee arthroplasty vary between Asian and Western patients: a meta-analysis. Clin Orthop Relat Res 476:946–960
Heyse TJ, Slane J, Peersman G, Dworschak P, Fuchs-Winkelmann S, Scheys L (2017) Balancing mobile-bearing unicondylar knee arthroplasty in vitro. Knee Surg Sports Traumatol Arthrosc 25:3733–3740. https://doi.org/10.1007/s00167-016-4241-8
Heyse TJ, El-Zayat BF, De Corte R, Scheys L, Chevalier Y, Fuchs-Winkelmann S, Labey L (2016) Balancing UKA: overstuffing leads to high medial collateral ligament strains. Knee Surg Sports Traumatol Arthrosc 24:3218–3228. https://doi.org/10.1007/s00167-015-3848-5
Hernigou P, Deschamps G (2004) Alignment influences wear in the knee after medial unicompartmental arthroplasty. Clinical orthopaedics and related research:161–165.
Elmallah RK, Mistry JB, Cherian JJ, Chughtai M, Bhave A, Roche MW, Mont MA (2016) Can we really “feel” a balanced total knee arthroplasty? J Arthroplasty 31:102–105
Gustke KA, Golladay GJ, Roche MW, Jerry GJ, Elson LC, Anderson CR (2014) Increased satisfaction after total knee replacement using sensor-guided technology. Bone Joint J 96-b:1333–1338. https://doi.org/10.1302/0301-620x.96b10.34068
van der Linde JA, Beath KJ, Leong AKL (2018) The reliability of sensor-assisted soft tissue measurements in primary total knee arthroplasty. J Arthroplasty 33:2502-2505.e2512
Ettinger M, Zoch JM, Becher C, Hurschler C, Stukenborg-Colsman C, Claassen L, Ostermeier S, Calliess T (2015) In vitro kinematics of fixed versus mobile bearing in unicondylar knee arthroplasty. Arch Orthop Trauma Surg 135:871–877
Jaeger S, Helling A, Bitsch RG, Seeger JB, Schuld C, Clarius M (2012) The influence of the femoral force application point on tibial cementing pressure in cemented UKA: an experimental study. Arch Orthop Trauma Surg 132:1589–1594
Su Z, Wang Z, Chen H (2019) A force line trajectory measuring system and algorithms for unicondylar knee replacement surgery. Annu Int Conf IEEE Eng Med Biol Soc 2019:2217–2221. https://doi.org/10.1109/embc.2019.8857007
Brimacombe JM, Wilson DR, Hodgson AJ, Ho KC, Anglin C (2009) Effect of calibration method on Tekscan sensor accuracy. J Biomech Eng 131:034503
Wilson DC, Niosi CA, Zhu QA, Oxland TR, Wilson DR (2006) Accuracy and repeatability of a new method for measuring facet loads in the lumbar spine. J Biomech 39:348–353
Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR (2014) Primary TKA patients with quantifiably balanced soft-tissue achieve significant clinical gains sooner than unbalanced patients. Adv Orthop 2014:628695
Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR (2014) A new method for defining balance: promising short-term clinical outcomes of sensor-guided TKA. J Arthroplasty 29:955–960
Nodzo SR, Franceschini V, Gonzalez Della Valle A (2017) Intraoperative load-sensing variability during cemented, posterior-stabilized total knee arthroplasty. J Arthroplasty 32:66–70
Meneghini RM, Ziemba-Davis MM, Lovro LR, Ireland PH, Damer BM (2016) Can intraoperative sensors determine the “target” ligament balance? Early outcomes in total knee arthroplasty. J Arthroplasty 31:2181–2187
Manning WA, Blain A, Longstaff L, Deehan DJ (2019) A load-measuring device can achieve fine-tuning of mediolateral load at knee arthroplasty but may lead to a more lax knee state. Knee Surg Sports Traumatol Arthrosc 27:2238–2250. https://doi.org/10.1007/978-981-13-1396-7_25
Acknowledgements
We thank Kelly Zammit, BVSc, and Coren Walters-Stewart, PhD, from Liwen Bianji, Edanz Editing China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript. We thank Zimmer Biomet for providing the instruments in the cadaveric surgical training programme.
Funding
This study was funded by Beijing Municipal Science and Technology Commission (grant number Z171100001017209), the National Natural Science Foundation of China (grant numbers 81972130, 81703896, 81972107, 81902203, 82072494), National Key Research and Development Program of China (grant number 2017YFC0108102) and the Capital Health Research and Development of Special (grant number 2020–2-4067).
Author information
Authors and Affiliations
Contributions
Xiaowei Sun and Wanshou Guo contributed to the conception and design. Xiaowei Sun and Yang Chen designed and produced the force sensor. Xiaowei Sun and Philippe Hernigou did the analysis and interpretation. Qidong Zhang and Weiguo Wang did the data collection. Xiaowei Sun wrote the article. Philippe Hernigou, Nianfei Zhang and Wanshou Guo did the revision of the article.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the ethics committee of the China-Japan Friendship Hospital, which was also the initiator of this series of UKA cadaveric surgical training programme. The approved number was 2020–50-k28.
Consent to participate
Informed consent was obtained from all training participants included in the study.
Consent for publication
The surgeons who participate in the training programme had consented to the submission of the report to the journal.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sun, X., Hernigou, P., Zhang, Q. et al. Sensor and machine learning–based assessment of gap balancing in cadaveric unicompartmental knee arthroplasty surgical training. International Orthopaedics (SICOT) 45, 2843–2849 (2021). https://doi.org/10.1007/s00264-021-05176-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05176-1