Abstract
Background
In settings with limited access to specialist services, differentiating septic arthritis—a surgical emergency—from non-infectious atraumatic arthropathy in paediatric patients is challenging, especially in a setting with a high burden of tuberculosis (TB). We aimed to investigate the aetiologies of swollen, painful joints in an urban setting in South Africa and determine how clinical and laboratory findings varied with diagnosis.
Patients and methods
A retrospective review of patients aged 12 or younger presenting to a paediatric hospital in Cape Town, South Africa, with atraumatic swollen, painful joints was conducted over a two year period from 2013 to 2015. Children were excluded if they did not have tissue culture or analysis conducted at our facility. Aetiology was classified as non-infectious, TB septic arthritis, or pyogenic arthritis from other bacterial causes.
Results
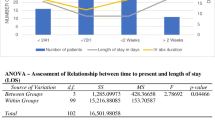
One hundred and four children met inclusion criteria. Arthritis was classified as non-infectious in 43 (41%), TB in 15 (14%), and pyogenic in 40 (38%), with six (6%) patients never receiving a final diagnosis. Mean C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and white blood cell count (WCC) were all significantly higher in pyogenic infectious arthritis compared with TB and non-infectious arthritis. There were no significant differences in these parameters between non-infectious and TB arthritis. Using cut-point analysis, thresholds were identified predictive of the presence of pyogenic arthritis versus TB or non-infectious arthritis; these included the presence of fever, CRP > 50 mg/L, ESR > 65 mm/h and WCC > 12x109/L. The absence of all of these criteria resulted in a negative predictive value of 100% for pyogenic infection; the presence of three to four criteria resulted in a positive predictive value of 71%.
Conclusions
Despite insignificant differences in their clinical presentation compared with non-infectious arthidities, 15% of children were diagnosed with tissue-confirmed TB infection. Predictive values of clinical criteria are reduced in our population due to elevated levels of inflammatory markers in all patients. Synovial biopsy to rule out TB is recommended in all patients in a high-burden setting given clinical similarity to non-infectious aetiologies.




Similar content being viewed by others
References
Dodwell ER (2013) Osteomyelitis and septic arthritis in children. Curr Opin Pediatr 25:58–63. https://doi.org/10.1097/mop.0b013e32835c2b42
Branson J, Vallejo JG, Flores AR et al (2017) The contemporary microbiology and rates of concomitant osteomyelitis in acute septic arthritis. Pediatr Infect Dis J 36:267–273. https://doi.org/10.1097/inf.0000000000001417
Maharajan K, Patro DK, Menon J et al (2013) Serum procalcitonin is a sensitive and specific marker in the diagnosis of septic arthritis and acute osteomyelitis. J Orthop Surg Res 8:1–7. https://doi.org/10.1186/1749-799x-8-19
Roberts J, Schaefer E, Gallo RA (2014) Indicators for detection of septic arthritis in the acutely swollen joint cohort of those without joint prostheses. Orthopedics 37:e98–e102. https://doi.org/10.3928/01477447-20140124-09
Carrol ED, Clark JE, Cant AJ (2001) Non-pulmonary tuberculosis. Paediatr Respir Rev 2:113–119. https://doi.org/10.1053/prrv.2001.0118
Harries AD (1990) Tuberculosis and human immunodeficiency virus infection in developing countries. Lancet 335:387–390
Malaviya AN, Kotwal PP (2003) Arthritis associated with tuberculosis. Best Pract Res Clin Rheumatol 17:319–343. https://doi.org/10.1016/s1521-6942(02)00126-2
Esposito S, Tagliabue C, Bosis S (2013) Tuberculosis in children. Mediterr J Hematol Infect Dis 5:2013064–2013068. https://doi.org/10.4084/mjhid.2013.064
Al-Matar MJ, Cabral DA, Petty RE (2001) Isolated tuberculous monoarthritis mimicking oligoarticular juvenile rheumatoid arthritis. J Rheumatol 28:204–206
Kim B, Punaro M (2008) A 13-month-old with persistent right knee swelling. Pediatr Infect Dis J 27(1039):1044–1045. https://doi.org/10.1097/inf.0b013e31817d877a
Kocher MS, Mandiga R, Zurakowski D et al (2004) Validation of a clinical prediction rule for the differentiation between septic arthritis and transient synovitis of the hip in children. J Bone Joint Surg A:1–7
Kocher MS, Zurakowski D, Kasser JR (1999) Differentiating between septic arthritis and transient synovitis of the hip in children: an evidence-based clinical prediction algorithm. J Bone Joint Surg A 81-A:1662–1670
Singhal R, Perry DC, Khan FN et al (2011) The use of CRP within a clinical prediction algorithm for the differentiation of septic arthritis and transient synovitis in children. J Bone Joint Surg Br Vol 93-B:1556–1561. https://doi.org/10.1302/0301-620x.93b11
Held M, Laubscher M, Mears S et al (2016) Diagnostic accuracy of the Xpert MTB/RIF assay for extrapulmonary tuberculosis in children with musculoskeletal infections. Pediatr Infect Dis J 35:1165–1168. https://doi.org/10.1097/inf.0000000000001271
Held M, Laubscher M, Zar HJ, Dunn RN (2014) GeneXpert polymerase chain reaction for spinal tuberculosis. Bone Joint J 96-B:1366–1369. https://doi.org/10.1302/0301-620x.96b10
Team RC (n.d.) R: a language and environment for statistical computing
Farer LS, Lowell AM, Meador MP (1979) Extrapulmonary tuberculosis in the United States. Am J Epidemiol 109:205–217
Peto HM, Pratt RH, Harrington TA et al (2009) Epidemiology of extrapulmonary tuberculosis in the United States, 1993–2006. Clin Infect Dis 49:1350–1357. https://doi.org/10.1086/605559
Rieder HL, Snider DE, Cauthen GM (1990) Extrapulmonary tuberculosis in the United States. Am Rev Respir Dis 141:347–351
Ceroni D, Cherkaoui A, Ferey S et al (2010) Kingella Kingae osteoarticular infections in young children: clinical features and contribution of a new specific real-time PCR assay to the diagnosis. J Pediatr Orthop 30:301–304
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of evidence: III
Rights and permissions
About this article
Cite this article
Upfill-Brown, A., Bruins, MF., Dix-Peek, S. et al. A clinical decision tool for septic arthritis in children based on epidemiologic data of atraumatic swollen painful joints in South Africa. International Orthopaedics (SICOT) 44, 2645–2652 (2020). https://doi.org/10.1007/s00264-020-04815-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04815-3