Abstract
Purpose
The neutrophil-to-lymphocyte ratio (NLR) has recently been found to be closely associated with the severity of trauma. This study aimed to analyze the correlation between the imaging severity of isolated tibial plateau fractures (TPFs) and the NLR in the blood.
Methods
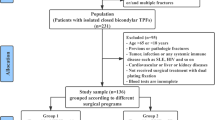
A total of 223 patients with isolated TPFs were enrolled in this retrospective study over five years. The data at hospital admission were extracted from an electronic database. Schatzker classification was performed according to the imaging data by two experienced orthopaedic surgeons. All patients were divided into two groups: group 1 included patients with mild-to-moderate fractures (Schatzker types I–IV), and group 2 included patients with severe fractures (Schatzker types V–VI). The NLR levels at hospital admission were statistically compared between the two groups.
Results
The blood NLR, hemoglobin level, red blood cell count, neutrophil count, platelet count, time from injury to admission, total protein, and Na+ levels were significantly different among the two groups. According to the receiver operating characteristic (ROC) curve, the cutoff for the NLR was 5.8. ROC curve analysis showed that the sensitivity of an NLR ≥ 5.8 to predict severe TPFs was 53.4%, and the specificity was 70.7%. In the multivariate analysis, NLR ≥ 5.8 and haemoglobin < lower limit appeared to be independent predictors of severe TPFs.
Conclusions
Our study is the first to demonstrate that the NLR level appears to be a useful biomarker for predicting the severity of isolated TPFs in young and middle-aged adults.




Similar content being viewed by others
References
Liu Y, Liao Z, Shang L, Huang W, Zhang D, Pei G (2017) Characteristics of unilateral tibial plateau fractures among adult patients hospitalized at an orthopaedic trauma Centre in China. Sci Rep 7:40647. https://doi.org/10.1038/srep40647
Ollivier M, Turati M, Munier M, Lunebourg A, Argenson JN, Parratte S (2016) Balloon tibioplasty for reduction of depressed tibial plateau fractures: preliminary radiographic and clinical results. Int Orthop 40:1961–1966. https://doi.org/10.1007/s00264-015-3047-5
Hoekstra H, Kempenaers K, Nijs S (2017) A revised 3-column classification approach for the surgical planning of extended lateral tibial plateau fractures. Eur J Trauma Emerg Surg 43:637–643. https://doi.org/10.1007/s00068-016-0696-z
Zhang BB, Sun H, Zhan Y, He QF, Zhu Y, Wang YK, Luo CF (2019) Reliability and repeatability of tibial plateau fracture assessment with an injury mechanism-based concept. Bone Joint Res 8:357–366. https://doi.org/10.1302/2046-3758.88.Bjr-2018-0331.R1
Manidakis N, Dosani A, Dimitriou R, Stengel D, Matthews S, Giannoudis P (2010) Tibial plateau fractures: functional outcome and incidence of osteoarthritis in 125 cases. Int Orthop 34:565–570. https://doi.org/10.1007/s00264-009-0790-5
Berger PE, Ofstein RA, Jackson DW, Morrison DS, Silvino N, Amador R (1989) MRI demonstration of radiographically occult fractures: what have we been missing? Radiographics 9:407–436. https://doi.org/10.1148/radiographics.9.3.2727354
Dirschl DR, Dawson PA (2004) Injury severity assessment in tibial plateau fractures. Clin Orthop Relat Res:85–92. https://doi.org/10.1097/01.blo.0000132626.13539.4b
Schatzker J, McBroom R, Bruce D (1979) The tibial plateau fracture. The Toronto experience 1968--1975. Clin Orthop Relat Res:94–104
Alexandru L, Haragus H, Deleanu B, Timar B, Poenaru DV, Vlad DC (2019) Haematology panel biomarkers for humeral, femoral, and tibial diaphyseal fractures. Int Orthop 43:1567–1572. https://doi.org/10.1007/s00264-019-04305-1
Templeton AJ, McNamara MG, Seruga B, Vera-Badillo FE, Aneja P, Ocana A, Leibowitz-Amit R, Sonpavde G, Knox JJ, Tran B, Tannock IF, Amir E (2014) Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst 106:dju124. https://doi.org/10.1093/jnci/dju124
Kim SC, Sun KH, Choi DH, Lee YM, Choi SW, Kang SH, Park KH, Song H (2016) Prediction of long-term mortality based on neutrophil-lymphocyte ratio after percutaneous coronary intervention. Am J Med Sci 351:467–472. https://doi.org/10.1016/j.amjms.2015.12.022
Temiz A, Ersozlu S (2019) Admission neutrophil-to-lymphocyte ratio and postoperative mortality in elderly patients with hip fracture. Ulus Travma Acil Cerrahi Derg 25:71–74. https://doi.org/10.5505/tjtes.2018.94572
Taşoğlu Ö, Bölük H, Şahin Onat Ş, Taşoğlu İ, Özgirgin N (2016) Is blood neutrophil-lymphocyte ratio an independent predictor of knee osteoarthritis severity? Clin Rheumatol 35:1579–1583. https://doi.org/10.1007/s10067-016-3170-8
Lattanzi S, Cagnetti C, Provinciali L, Silvestrini M (2016) Neutrophil-to-lymphocyte ratio predicts the outcome of acute Intracerebral hemorrhage. Stroke 47:1654–1657. https://doi.org/10.1161/STROKEAHA.116.013627
Lumsdaine W, Easton RM, Lott NJ, White A, Malmanche TL, Lemmert K, Weber DG, Balogh ZJ (2014) Neutrophil oxidative burst capacity for peri-operative immune monitoring in trauma patients. Injury 45:1144–1148. https://doi.org/10.1016/j.injury.2014.04.019
Zahorec R (2001) Ratio of neutrophil to lymphocyte counts--rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy 102:5–14
Kfuri M, Schatzker J (2018) Revisiting the Schatzker classification of tibial plateau fractures. Injury 49:2252–2263. https://doi.org/10.1016/j.injury.2018.11.010
Dilektasli E, Inaba K, Haltmeier T, Wong MD, Clark D, Benjamin ER, Lam L, Demetriades D (2016) The prognostic value of neutrophil-to-lymphocyte ratio on mortality in critically ill trauma patients. J Trauma Acute Care Surg 81:882–888. https://doi.org/10.1097/ta.0000000000000980
Fisher A, Srikusalanukul W, Fisher L, Smith P (2016) The neutrophil to lymphocyte ratio on admission and short-term outcomes in orthogeriatric patients. Int J Med Sci 13:588–602. https://doi.org/10.7150/ijms.15445
Morell V, Lundgren E, Gillott A (1993) Predicting severity of trauma by admission white blood cell count, serum potassium level, and arterial pH. South Med J 86:658–659. https://doi.org/10.1097/00007611-199306000-00014
Balta S, Ozturk C, Yildirim AO, Erdogan S, Celik T (2016) The neutrophil-lymphocyte ratio and atherosclerosis. Expert Rev Cardiovasc Ther 14:885. https://doi.org/10.1080/14779072.2016.1194199
Forget P, Moreau N, Engel H, Cornu O, Boland B, De Kock M, Yombi JC (2015) The neutrophil-to-lymphocyte ratio (NLR) after surgery for hip fracture (HF). Arch Gerontol Geriatr 60:366–371. https://doi.org/10.1016/j.archger.2014.11.008
Oh SJ, Lee JK, Shin OS (2019) Aging and the immune system: the impact of immunosenescence on viral infection, immunity and vaccine immunogenicity. Immune Netw 19:e37. https://doi.org/10.4110/in.2019.19.e37
Park JM (2017) Neutrophil-to-lymphocyte ratio in trauma patients. J Trauma Acute Care Surg 82:225–226. https://doi.org/10.1097/ta.0000000000001266
Smith GH, Tsang J, Molyneux SG, White TO (2011) The hidden blood loss after hip fracture. Injury 42:133–135. https://doi.org/10.1016/j.injury.2010.02.015
Acknowledgements
The authors acknowledge Dr. Jialiang Guo and Dr. Wei Chen.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Z., Tian, S., Zhao, K. et al. Neutrophil to lymphocyte ratio and fracture severity in young and middle-aged patients with tibial plateau fractures. International Orthopaedics (SICOT) 44, 2769–2777 (2020). https://doi.org/10.1007/s00264-020-04793-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04793-6