Abstract
Background
We evaluated the pre-operative factors affecting anatomical and reverse total shoulder arthroplasty (TSA and RTSA) indications in primary osteoarthritis and compared outcomes in patients aged 70 years and older.
Methods
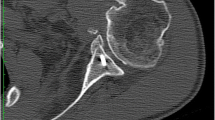
Fifty-eight patients received a TSA with an all-polyethylene glenoid component (APGC) or an RTSA with/without glenoid lateralization and the same curved short-stem humeral component. Active anterior and lateral elevation (AAE, ALE), internal and external rotation (IR, ER), pain, and the Constant–Murley score (CS) were recorded pre and post-operatively. Pre-operative rotator cuff (RC) fatty infiltration (FI) and modified Walch glenoid morphology were assessed. Humeral and glenoid component radiological outcomes were recorded.
Results
RTSA were older than TSA patients (p = 0.006), had lower pre-operative AAE (p < 0.001), ALE (p < 0.001), IR (p = 0.002), pain (p = 0.008) and CS (p < 0.001), and greater supraspinatus FI (p < 0.001). At a mean of 28.8 months, both implants yielded significantly different post-operative scores and similar complication rates. Both groups achieved similar post-operative AAE, ER, and IR; ALE was higher in TSA (p = 0.006); and AAE and ALE delta scores were higher in RTSA (p = 0.045 and p = 0.033, respectively). Radiolucent line rates were higher around the TSA APGC than the RTSA baseplate (p = 0.001). High-grade RC FI adversely affected mobility improvement. Humeral cortical thinning was significantly higher in TSA (p = 0.001).
Conclusion
RTSA patients were older, had poorer pre-operative active mobility, and had greater RC FI than TSA. Both devices provided good mid-term clinical and ROM improvement.




Similar content being viewed by others
References
Steinhaus ME, Gowd AK, Hurwit DJ, Lieber AC, Liu JN (2019) Return to work after shoulder arthroplasty: a systematic review and meta-analysis. J Shoulder Elb Surg. https://doi.org/10.1016/j.jse.2018.12.011
Roberson TA, Bentley JC, Griscom JT, Kissenberth MJ, Tolan SJ, Hawkins RJ, Tokish JM (2017) Outcomes of total shoulder arthroplasty in patients younger than 65 years: a systematic review. J Shoulder Elb Surg 26:1298–1306. https://doi.org/10.1016/j.jse.2016.12.069
Patel RB, Muh S, Okoroha KR, Wright TW, Flurin PH, Roche C, Zuckerman JD (2018) Results of total shoulder arthroplasty in patients aged 55 years or younger versus those older than 55 years: an analysis of 1135 patients with over 2 years of follow-up. J Shoulder Elb Surg. https://doi.org/10.1016/j.jse.2018.09.029
Liu JN, Steinhaus ME, Garcia GH, Chang B, Fields K, Dines DM, Warren RF, Gulotta LV (2018) Return to sport after shoulder arthroplasty: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 26:100–112. https://doi.org/10.1007/s00167-017-4547-1
Bryant D, Litchfield R, Sandow M, Gartsman GM, Guyatt G, Kirkley A (2005) A comparison of pain, strength, range of motion, and functional outcomes after hemiarthroplasty and total shoulder arthroplasty in patients with osteoarthritis of the shoulder. A systematic review and meta-analysis. J Bone Joint Surg Am 87:1947–1956. https://doi.org/10.2106/JBJS.D.02854
Young AA, Walch G, Pape G, Gohlke F, Favard L (2012) Secondary rotator cuff dysfunction following total shoulder arthroplasty for primary glenohumeral osteoarthritis: results of a multicenter study with more than five years of follow-up. J Bone Joint Surg Am 94:685–693. https://doi.org/10.2106/JBJS.J.00727
Grammont PM, Baulot E (1993) Delta shoulder prosthesis for rotator cuff rupture. Orthopedics 16:65–68
Shukla DR, McAnany S, Kim J, Overley S, Parsons BO (2016) Hemiarthroplasty versus reverse shoulder arthroplasty for treatment of proximal humeral fractures: a meta-analysis. J Shoulder Elb Surg 25:330–340. https://doi.org/10.1016/j.jse.2015.08.030
Erickson BJ, Bohl DD, Cole BJ, Verma NN, Nicholson G, Romeo AA, Harris JD (2018) Reverse total shoulder arthroplasty: indications and techniques across the world. Am J Orthop (Belle Mead NJ) 47. DOI https://doi.org/10.12788/ajo.2018.0079
Walch G, Moraga C, Young A, Castellanos-Rosas J (2012) Results of anatomic nonconstrained prosthesis in primary osteoarthritis with biconcave glenoid. J Shoulder Elb Surg 21:1526–1533. https://doi.org/10.1016/j.jse.2011.11.030
Moineau G, Levigne C, Boileau P, Young A, Walch G, French Society for S, Elbow (2012) Three-dimensional measurement method of arthritic glenoid cavity morphology: feasibility and reproducibility. Orthop Traumatol Surg Res 98:S139–S145. https://doi.org/10.1016/j.otsr.2012.06.007
Walch G, Vezeridis PS, Boileau P, Deransart P, Chaoui J (2015) Three-dimensional planning and use of patient-specific guides improve glenoid component position: an in vitro study. J Shoulder Elb Surg 24:302–309. https://doi.org/10.1016/j.jse.2014.05.029
Gauci MO, Boileau P, Baba M, Chaoui J, Walch G (2016) Patient-specific glenoid guides provide accuracy and reproducibility in total shoulder arthroplasty. Bone Joint J 98-B:1080–1085. https://doi.org/10.1302/0301-620X.98B8.37257
Luedke C, Kissenberth MJ, Tolan SJ, Hawkins RJ, Tokish JM (2018) Outcomes of anatomic total shoulder arthroplasty with B2 glenoids: a systematic review. JBJS Rev 6:e7. https://doi.org/10.2106/JBJS.RVW.17.00112
Bercik MJ, Kruse K 2nd, Yalizis M, Gauci MO, Chaoui J, Walch G (2016) A modification to the Walch classification of the glenoid in primary glenohumeral osteoarthritis using three-dimensional imaging. J Shoulder Elb Surg 25:1601–1606. https://doi.org/10.1016/j.jse.2016.03.010
Chan K, Knowles NK, Chaoui J, Ferreira LM, Walch G, Athwal GS (2018) Is the Walch B3 glenoid significantly worse than the B2? Should Elb 10:256–261. https://doi.org/10.1177/1758573217724111
Chan K, Knowles NK, Chaoui J, Gauci MO, Ferreira LM, Walch G, Athwal GS (2017) Characterization of the Walch B3 glenoid in primary osteoarthritis. J Shoulder Elb Surg 26:909–914. https://doi.org/10.1016/j.jse.2016.10.003
Chin PC, Hachadorian ME, Pulido PA, Munro ML, Meric G, Hoenecke HR Jr (2015) Outcomes of anatomic shoulder arthroplasty in primary osteoarthritis in type B glenoids. J Shoulder Elb Surg 24:1888–1893. https://doi.org/10.1016/j.jse.2015.05.052
Boileau P, Morin-Salvo N, Gauci MO, Seeto BL, Chalmers PN, Holzer N, Walch G (2017) Angled BIO-RSA (bony-increased offset-reverse shoulder arthroplasty): a solution for the management of glenoid bone loss and erosion. J Shoulder Elb Surg 26:2133–2142. https://doi.org/10.1016/j.jse.2017.05.024
Point GM (2013) Total shoulder replacement—EU analysis and market forecasts. In. GlobalData
Porcellini G, Combi A, Merolla G, Bordini B, Stea S, Zanoli G, Paladini P (2018) The experience of the RIPO, a shoulder prosthesis registry with 6-year follow-up. Musculoskelet Surg 102:273–282. https://doi.org/10.1007/s12306-017-0529-1
Implants RotOP (2014) Annual report 2016 Regione Emilia Romagna. In. RIPO
Chalmers PN, Salazar DH, Romeo AA, Keener JD, Yamaguchi K, Chamberlain AM (2018) Comparative utilization of reverse and anatomic total shoulder arthroplasty: a comprehensive analysis of a high-volume center. J Am Acad Orthop Surg 26:e504–e510. https://doi.org/10.5435/JAAOS-D-17-00075
Mizuno N, Denard PJ, Raiss P, Walch G (2013) Reverse total shoulder arthroplasty for primary glenohumeral osteoarthritis in patients with a biconcave glenoid. J Bone Joint Surg Am 95:1297–1304. https://doi.org/10.2106/JBJS.L.00820
Steen BM, Cabezas AF, Santoni BG, Hussey MM, Cusick MC, Kumar AG, Frankle MA (2015) Outcome and value of reverse shoulder arthroplasty for treatment of glenohumeral osteoarthritis: a matched cohort. J Shoulder Elb Surg 24:1433–1441. https://doi.org/10.1016/j.jse.2015.01.005
Wright MA, Keener JD, Chamberlain AM (2019) Comparison of clinical outcomes after anatomic total shoulder arthroplasty and reverse shoulder arthroplasty in patients 70 years and older with glenohumeral osteoarthritis and an intact rotator cuff. J Am Acad Orthop Surg. https://doi.org/10.5435/JAAOS-D-19-00166
Neer CS 2nd (1974) Replacement arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am 56:1–13
Friedman RJ, Hawthorne KB, Genez BM (1992) The use of computerized tomography in the measurement of glenoid version. J Bone Joint Surg Am 74:1032–1037
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC (1994) Fatty muscle degeneration in cuff ruptures. Pre- and post-operative evaluation by CT scan. Clin Orthop Relat Res:78–83
Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C (1999) Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elb Surg 8:599–605
Boutsiadis A, Lenoir H, Denard PJ, Panisset JC, Brossard P, Delsol P, Guichard F, Barth J (2018) The lateralization and distalization shoulder angles are important determinants of clinical outcomes in reverse shoulder arthroplasty. J Shoulder Elb Surg 27:1226–1234. https://doi.org/10.1016/j.jse.2018.02.036
Boileau P, Moineau G, Roussanne Y, O'Shea K (2011) Bony increased-offset reversed shoulder arthroplasty: minimizing scapular impingement while maximizing glenoid fixation. Clin Orthop Relat Res 469:2558–2567. https://doi.org/10.1007/s11999-011-1775-4
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res:160–164
Kibler WB, Sciascia A, Dome D (2006) Evaluation of apparent and absolute supraspinatus strength in patients with shoulder injury using the scapular retraction test. Am J Sports Med 34:1643–1647. https://doi.org/10.1177/0363546506288728
Merolla G, De Santis E, Sperling JW, Campi F, Paladini P, Porcellini G (2010) Infraspinatus strength assessment before and after scapular muscles rehabilitation in professional volleyball players with scapular dyskinesis. J Shoulder Elb Surg 19:1256–1264. https://doi.org/10.1016/j.jse.2010.01.022
Molè D RO, Riand N, Levigne C, Walch G. (1999) Cemented glenoid components: results in osteoarthritis and rheumatoid arthritis. In: Walch G BP, editors. (ed) Shoulder arthroplasty. Springer-Verlag, Berlin. pp. 163-171
Sperling JW, Cofield RH, O'Driscoll SW, Torchia ME, Rowland CM (2000) Radiographic assessment of ingrowth total shoulder arthroplasty. J Shoulder Elb Surg 9:507–513
Schnetzke M, Coda S, Raiss P, Walch G, Loew M (2016) Radiologic bone adaptations on a cementless short-stem shoulder prosthesis. J Shoulder Elb Surg 25:650–657. https://doi.org/10.1016/j.jse.2015.08.044
Sperling JW, Cofield RH, Rowland CM (2000) Heterotopic ossification after total shoulder arthroplasty. J Arthroplast 15:179–182
Melis B, DeFranco M, Ladermann A, Mole D, Favard L, Nerot C, Maynou C, Walch G (2011) An evaluation of the radiological changes around the Grammont reverse geometry shoulder arthroplasty after eight to 12 years. J Bone Joint Surg (Br) 93:1240–1246. https://doi.org/10.1302/0301-620X.93B9.25926
Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D (2004) Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg (Br) 86:388–395
Crosby LA, Hamilton A, Twiss T (2011) Scapula fractures after reverse total shoulder arthroplasty: classification and treatment. Clin Orthop Relat Res 469:2544–2549. https://doi.org/10.1007/s11999-011-1881-3
Chalmers PN, Keener JD (2016) Expanding roles for reverse shoulder arthroplasty. Curr Rev Musculoskelet Med 9:40–48. https://doi.org/10.1007/s12178-016-9316-0
Merolla G, Ciaramella G, Fabbri E, Walch G, Paladini P, Porcellini G (2016) Total shoulder replacement using a bone ingrowth central peg polyethylene glenoid component: a prospective clinical and computed tomography study with short- to mid-term follow-up. Int Orthop 40:2355–2363. https://doi.org/10.1007/s00264-016-3255-7
Griffin JW, Hadeed MM, Novicoff WM, Browne JA, Brockmeier SF (2014) Patient age is a factor in early outcomes after shoulder arthroplasty. J Shoulder Elb Surg 23:1867–1871. https://doi.org/10.1016/j.jse.2014.04.004
Bovonratwet P, Malpani R, Ondeck NT, Tyagi V, Grauer JN (2019) Elective total shoulder arthroplasty in octogenarians: a safe procedure. J Am Acad Orthop Surg 27:145–154. https://doi.org/10.5435/JAAOS-D-17-00364
Merolla G, Walch G, Ascione F, Paladini P, Fabbri E, Padolino A, Porcellini G (2018) Grammont humeral design versus onlay curved-stem reverse shoulder arthroplasty: comparison of clinical and radiographic outcomes with minimum 2-year follow-up. J Shoulder Elb Surg 27:701–710. https://doi.org/10.1016/j.jse.2017.10.016
Lopez CD, Maier SP, Bloom ZJ, Shiu BB, Petkovic D, Jobin CM (2018) Outcomes of lesser tuberosity osteotomy in revision anatomic shoulder arthroplasty. J Shoulder Elb Surg 27:e219–e224. https://doi.org/10.1016/j.jse.2017.12.006
Rauck RC, Swarup I, Chang B, Dines DM, Warren RF, Gulotta LV, Henn RF 3rd (2018) Effect of pre-operative patient expectations on outcomes after reverse total shoulder arthroplasty. J Shoulder Elb Surg 27:e323–e329. https://doi.org/10.1016/j.jse.2018.05.026
Choate WS, Shanley E, Washburn R, Tolan SJ, Salim TI, Tadlock J, Shealy EC, Long CD, Crawford AE, Kissenberth MJ, Lonergan KT, Hawkins RJ, Tokish JM (2017) The incidence and effect of fatty atrophy, positive tangent sign, and rotator cuff tears on outcomes after total shoulder arthroplasty. J Shoulder Elb Surg 26:2110–2116. https://doi.org/10.1016/j.jse.2017.05.022
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
IRB approval was obtained from the institutional review board of the Coordinator Center in Cattolica, Italy, as part of a large Shoulder Arthroplasty database (Prot. No. 6478/20191.5/117 CEROM, Italy).
Conflict of interest
Gilles Walch, Vincenzo De Cupis, Francesco Franceschi, Claudio Ascani, and Giuseppe Porcellini are paid consultants for the Wright Medical Group.
The other authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of Evidence: Level III, Retrospective cohort design, Treatment study
Rights and permissions
About this article
Cite this article
Merolla, G., De Cupis, M., Walch, G. et al. Pre-operative factors affecting the indications for anatomical and reverse total shoulder arthroplasty in primary osteoarthritis and outcome comparison in patients aged seventy years and older. International Orthopaedics (SICOT) 44, 1131–1141 (2020). https://doi.org/10.1007/s00264-020-04501-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04501-4