Abstract
Introduction
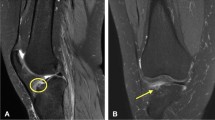
Osgood-Schlatter disease (OSD) is a traction apophysitis of the tibial tubercle and a common cause of anterior knee pain in growing adolescents. A variety of benign neoplasms can also cause bony prominence over the tibial tubercle in adolescents that might clinically imitate OSD. Therefore, the differential diagnosis of tumours mimicking OSD is critical and considered the primary goal of this study.
Methods
Eleven patients who were referred to our orthopaedic oncology department with clinical suspicions of OSD and obscure radiographic presentation were identified. The final diagnosis was OSD in three cases. The demographic, clinical, and radiologic characteristics of the remaining eight patients in whom a tumour mimicked OSD were evaluated. The diagnosis was confirmed by pathologic examination.
Results
The final diagnosis was periosteal chondroma in four cases, osteochondroma in three cases, and dysplasia epiphysealis hemimelica (DEH) in one case. The average age of the patients was 10.5 ± 3.1 years. In the majority of patients (62.5%), the lesion was painless. The mean size of the bump was 6.5 ± 1.2 cm2. In patients with a painful knee, the pain was constant and activity-independent. At history taking, the pain and bump size were progressive.
Conclusion
Lack of pain, progressive pain and bump, activity-independent pain, a bump size larger than 5 cm2 at presentation, and age fewer than ten years could be considered in favour of tumours and against OSD.




Similar content being viewed by others
References
Gholve PA, Scher DM, Khakharia S, Widmann RF, Green DW (2007) Osgood schlatter syndrome. Curr Opin Pediatr 19(1):44–50
Nkaoui M, El Alouani EM (2017) Osgood-schlatter disease: risk of a disease deemed banal. Pan Afr Med J 28:56. https://doi.org/10.11604/pamj.2017.28.56.13185
Patel DR, Villalobos A (2017) Evaluation and management of knee pain in young athletes: overuse injuries of the knee. Translat Pediatr 6(3):190
Siddiq MAB (2018) Osgood-Schlatter disease unveiled under high-frequency ultrasonogram. Cureus 10(10)
Indiran V, Jagannathan D (2018) Osgood-Schlatter disease. N Engl J Med 378(11):e15. https://doi.org/10.1056/NEJMicm1711831
Vancauwenberghe T, Vanhoenacker F, Van Doninck J, Declercq H (2013) Periosteal chondroma of the proximaltibia mimicking Osgood-Schlatter’s disease. JBR-BTR 96(1):30–33
G B, P P, S N, J M (2016) Solitary Osteochondroma of the tibial tuberosity mimicking Osgood-Schlatter lesion: a rare cause of anterior knee pain in adolescents: a case report. Malays Orthop J 10(2):47
Jamshidi K, Bagherifard A, Mirzaei A (2017) Desmoplastic fibroma versus soft-tissue desmoid tumour of forearm: a case series of diagnosis, surgical approach, and outcome. J Hand Surg Eur Vol 42(9):952–958
Jamshidi K, Givehchian B, Mirzaei A (2017) Florid reactive periostitis of the long bone: a case series of seven patients. J Orthop Sci 22(3):560–565
Jamshidi K, Mirzaei A (2017) Long bone enchondroma vs. low-grade chondrosarcoma: current concepts review. Shafa Orthop J 4(1):e9155
Baumfeld D, Pires R, Macedo B, Abreu-e-Silva G, Alves T, Raduan P, Nery C (2014) Trevor disease (memimelic epiphyseal displasia): 12-year follow-up case report and literature review. Ann Med Health Sci Res 4(1):9–13
Araujo CR Jr, Montandon S, Montandon C, Teixeira K-I-SS, Moraes FB, Moreira MA (2006) Dysplasia epiphysealis hemimelica of the patella. Radiographics 26(2):581–586
Smith JM, Varacallo M (2019) Osgood Schlatter’s disease (tibial tubercle apophysitis). StatPearls Publishing, Treasure island
Murphy CE, Kenny CM (2019) Not just for boys: a rare case of symptomatic Osgood-Schlatter disease in a skeletally mature woman. BMJ Case Rep 12(3):e228963
Circi E, Beyzadeoglu T (2017) Results of arthroscopic treatment in unresolved Osgood-Schlatter disease in athletes. Int Orthop 41(2):351–356
Vaishya R, Azizi AT, Agarwal AK, Vijay V (2016) Apophysitis of the tibial tuberosity (Osgood-Schlatter disease): a review. Cureus 8(9)
Lee DW, Kim MJ, Kim WJ, Ha JK, Kim JG (2016) Correlation between magnetic resonance imaging characteristics of the patellar tendon and clinical scores in Osgood-Schlatter disease. Knee Surg Relat Res 28(1):62
Aparicio G, Abril J, Calvo E, Alvarez L (1997) Radiologic study of patellar height in Osgood-Schlatter disease. J Pediatr Orthop 17(1):63–66
Seyfettinoğlu F, Köse Ö, Oğur HU, Tuhanioğlu Ü, Çiçek H, Acar B (2018) Is there a relationship between patellofemoral alignment and Osgood–Schlatter disease? A case-control study. J Knee Surg. https://doi.org/10.1055/s-0038-1676523
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the review board of our institute, and informed consent was obtained from the patients’ parents to use their medical data for publication.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jamshidi, K., Mirkazemi, M., Izanloo, A. et al. Benign bone tumours of tibial tuberosity clinically mimicking Osgood-Schlatter disease: a case series. International Orthopaedics (SICOT) 43, 2563–2568 (2019). https://doi.org/10.1007/s00264-019-04397-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04397-9