Abstract
Purpose
The purpose of this study was to compare and evaluate the safety and efficacy of percutaneous vertebroplasty at a hyperextension position (PVPHP) and percutaneous kyphoplasty at a hyperextension position (PKPHP) for the treatment of osteoporotic Kümmell’s disease.
Methods
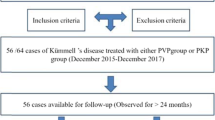
This study was a retrospective, single-centre study. There were 35 patients with osteoporotic Kümmell’s disease who were analyzed. Twenty-two of them underwent PVPHP and the other 13 patients underwent PKPHP from January 2013 to January 2015. The volume of bone cement injection and operation costs were compared. We compared the visual analogue score (VAS) and vertebral Cobb’s angle at pre-operation, the second day after operation, and the final follow-up. We compared the Oswestry disability index (ODI) score at the pre-operation and the final follow-up.
Results
There were no significant differences in gender, age, course of disease, bone mineral density (BMD), and mean follow-up time between the two groups (P > 0.05). Regarding the costs of the operation, the PKPHP group was significantly higher than the PVPHP group (P < 0.05). Compared with the pre-operation (P < 0.05), the post-operative ODI score, VAS, and Cobb’s angle of the two groups were improved significantly. Even though the correction of Cobb’s angle in the PKPHP group was slightly better than the PVPHP position group, there were no significant differences between two groups (P > 0.05). At the final follow-up, the Cobb’s angle was increased in both groups, but there was no significant difference (P > 0.05). There was no significant difference in the bone cement leakage rate between the two groups (P > 0.05).
Conclusion
For the treatment of Kümmell’s disease, PVPHP and PKPHP are both safe and effective, but PVPHP is more economical and can be considered a preferred method of treatment.



Similar content being viewed by others
References
Libicher M, Appelt A, Berger I, Baier M, Meeder PJ, Grafe I, Dafonseca K, Nöldge G, Kasperk C (2007) The intravertebral vacuum phenomen as specific sign of osteonecrosis in vertebral compression fractures: results from a radiological and histological study. Eur Radiol 17(9):2248–2252
Swartz K, Fee D (2008) Kummell’s disease: a case report and literature review. Spine (Phila Pa 1976) 33(5):E152–E155. https://doi.org/10.1097/BRS.0b013e3181657f31
Yang H, Pan J, Wang G (2014) A review of osteoporotic vertebral fracture nonunion management. Spine (Phila Pa 1976) 39(26 Spec No.):B4-6. https://doi.org/10.1097/brs.0000000000000538
Chen GD, Lu Q, Wang GL, Zou J, Yang HL, Yang Y, Luo ZP (2015) Percutaneous kyphoplasty for Kummell disease with severe spinal canal stenosis. Pain Physician 18(6):E1021–E1028
Jang JS, Kim DY, Lee SH (2003) Efficacy of percutaneous vertebroplasty in the treatment of intravertebral pseudarthrosis associated with noninfected avascular necrosis of the vertebral body. Spine (Phila Pa 1976) 28(14):1588–1592
Yang H, Gan M, Zou J, Mei X, Shen X, Wang G, Chen L (2010) Kyphoplasty for the treatment of Kummell’s disease. Orthopedics 33(7):479. https://doi.org/10.3928/01477447-20100526-07
Do HM, Jensen ME, Marx WF, Kallmes DF (1999) Percutaneous vertebroplasty in vertebral osteonecrosis (Kummell’s spondylitis). Neurosurg Focus 7(1):e2
Peh WC, Gelbart MS, Gilula LA, Peck DD (2003) Percutaneous vertebroplasty: treatment of painful vertebral compression fractures with intraosseous vacuum phenomena. AJR Am J Roentgenol 180(5):1411–1417. https://doi.org/10.2214/ajr.180.5.1801411
Han S, Wan S, Ning L, Tong Y, Zhang J, Fan S (2011) Percutaneous vertebroplasty versus balloon kyphoplasty for treatment of osteoporotic vertebral compression fracture: a meta-analysis of randomised and non-randomised controlled trials. Int Orthop 35(9):1349–1358. https://doi.org/10.1007/s00264-011-1283-x
Wu AM, Chi YL, Ni WF (2013) Vertebral compression fracture with intravertebral vacuum cleft sign: pathogenesis, image, and surgical intervention. Asian Spine J 7(2):148–155. https://doi.org/10.4184/asj.2013.7.2.148
Zhang GQ, Gao YZ, Chen SL, Ding S, Gao K, Wang HQ (2015) Comparison of percutaneous vertebroplasty and percutaneous kyphoplasty for the management of Kümmell’s disease: a retrospective study. Indian J Orthop 49(6):577–582. https://doi.org/10.4103/0019-5413.168752
van der Schaaf I, Fransen H (2009) Percutaneous vertebroplasty as treatment for Kummell’s disease. JBR-BTR : organe de la Societe royale belge de radiologie (SRBR) = orgaan van de Koninklijke Belgische Vereniging voor Radiologie (KBVR) 92(2):83–85
Huang Y, Peng M, He S, Tang X, Dai M, Tang C (2016) Clinical efficacy of percutaneous kyphoplasty at the hyperextension position for the treatment of osteoporotic Kummell disease. Clin Spine Surg 29(4):161–166. https://doi.org/10.1097/bsd.0000000000000259
Hur W, Lee JJ, Kim J, Kang SW, Lee IO, Lee MK, Choi SS (2014) Spontaneous air reduction of vertebra plana with Kummell’s disease during vertebroplasty: subsequent experience with an intentional trial. Pain medicine (Malden, Mass) 15(7):1240–1242. https://doi.org/10.1111/pme.12443
Eom KS, Kim TY (2012) Percutaneous vertebroplasty-induced adjacent vertebral compression fracture. Pain Physician 15(4):E527–E532
Lane JI, Maus TP, Wald JT, Thielen KR, Bobra S, Luetmer PH (2002) Intravertebral clefts opacified during vertebroplasty: pathogenesis, technical implications, and prognostic significance. AJNR Am J Neuroradiol 23(10):1642–1646
Krauss M, Hirschfelder H, Tomandl B, Lichti G, Bar I (2006) Kyphosis reduction and the rate of cement leaks after vertebroplasty of intravertebral clefts. Eur Radiol 16(5):1015–1021. https://doi.org/10.1007/s00330-005-0056-6
Tsai TT, Chen WJ, Lai PL, Chen LH, Niu CC, Fu TS, Wong CB (2003) Polymethylmethacrylate cement dislodgment following percutaneous vertebroplasty: a case report. Spine (Phila Pa 1976) 28(22):E457–E460. https://doi.org/10.1097/01.brs.0000096668.54378.25
Wang HS, Kim HS, Ju CI, Kim SW (2008) Delayed bone cement displacement following balloon kyphoplasty. J Korean Neurosurg Soc 43(4):212–214. https://doi.org/10.3340/jkns.2008.43.4.212
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent was not required.
Rights and permissions
About this article
Cite this article
Zhang, J., Fan, Y., He, X. et al. Is percutaneous kyphoplasty the better choice for minimally invasive treatment of neurologically intact osteoporotic Kümmell’s disease? A comparison of two minimally invasive procedures. International Orthopaedics (SICOT) 42, 1321–1326 (2018). https://doi.org/10.1007/s00264-018-3832-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3832-z