Abstract
Purpose
Chronic infection (CO) and infected non-union of the long bones are relatively rare conditions in paediatric patients. Large bone defects secondary to these conditions can be managed with the induced membrane technique. The technique requires grafting of the bone void, although it is not yet established what bone substitute is the best option. The aim of this work was to evaluate the outcome and efficacy of treatment in children with CO and infected non-union of the long bones using the induced membrane technique and bone (BG) versus beta-tricalcium phosphate (BTP) grafting.
Methods
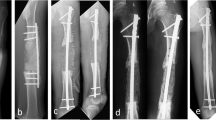
Eight skeletally immature patients with CO and infected non-union of the long bones were treated surgically between 2010 and 2017 by a combination of resection of necrotic infected bone, debridement of surrounding soft tissue, osteosynthesis using a stable internal fixation when needed, and application of antibiotic-laden cement (ALC) spacer inducing new membrane before final bone reconstruction with bone substitutes: BTP in five cases, BG (allograft and/or autologous graft) in three cases. A second surgical step, once inflammatory markers had normalized, consisted of ALC spacer removal, application of BG or BTP graft and concomitant stable osteosynthesis, if needed, if this had not been done during the first surgical stage. All the patients underwent clinical, laboratory and imaging evaluation before and after surgery. Antibiotics were adjusted according to culture and sensitivity.
Results
Mean patient age at time of diagnosis was 13 ± four years (range, 4–16) and all had at least a 12-month follow-up (range 12–60). Estimated time for induced membrane formation was significantly shorter in patients treated with BTP compared with BG: 3±1 vs. 10±2 (p = 0.02). This result was confirmed by multivariate analysis (p = 0.044) taking into account adjustment for age of patients and time after initial surgery. Time of final union was about 5.5 ± 4.1 months (range 2–66). At the last follow-up visit, bone had healed and all the patients had resumed daily living and sports activities.
Conclusion
The induced membrane technique with BG or BTP graft can achieve bone healing in large bone defects secondary to CO and infected non-union in children and adolescents. The choice of bone substitute is important. Our preliminary results show graft integration and bone healing can be expected sooner if BTP is used as bone void filler.

Similar content being viewed by others
References
Fitoussi F, Ilharreborde B (2015) Is the induced-membrane technique successful for limb reconstruction after resecting large bone tumors in children? Clin Orthop Rel Res 473:2067–2075. https://doi.org/10.1007/s11999-015-4164-6
Pannier S, Pejin Z, Dana C, Masquelet AC, Glorion C (2013) Induced membrane technique for the treatment of congenital pseudarthrosis of the tibia: preliminary results of five cases. J Child Orthop 7:477–485. https://doi.org/10.1007/s11832-013-0535-2
Harik NS, Smeltzer MS (2010) Management of acute hematogenous osteomyelitis in children. Expert Rev Anti-Infect Ther 8:175–181. https://doi.org/10.1586/eri.09.130
Gouron R, Petit L, Boudot C, Six I, Brazier M, Kamel S, Mentaverri R (2017) Osteoclasts and their precursors are present in the induced-membrane during bone reconstruction using the Masquelet technique. J Tissue Eng Regen Med 11:382–389. https://doi.org/10.1002/term.1921
Nicholas RW Jr (2015) CORR insights: is the induced-membrane technique successful for limb reconstruction after resecting large bone tumors in children? Clin Orthop Rel Res 473:2076–2078. https://doi.org/10.1007/s11999-015-4206-0
Morelli I, Drago L, George DA, Romano D, Romano CL (2017) Managing large bone defects in children: a systematic review of the ‘induced membrane technique’. J Pediatr Orthop B. https://doi.org/10.1097/BPB.0000000000000456
Gouron R, Deroussen F, Plancq MC, Collet LM (2013) Bone defect reconstruction in children using the induced membrane technique: a series of 14 cases. Orthop Traumatol Surg Res 99:837–843. https://doi.org/10.1016/j.otsr.2013.05.005
Gouron R (2016) Surgical technique and indications of the induced membrane procedure in children. Orthop Traumatol Surg Res 102:S133–S139. https://doi.org/10.1016/j.otsr.2015.06.027
Auregan JC, Begue T, Rigoulot G, Glorion C, Pannier S (2016) Success rate and risk factors of failure of the induced membrane technique in children: a systematic review. Injury 47(Suppl 6):S62–SS7. https://doi.org/10.1016/S0020-1383(16)30841-5
Wang X, Luo F, Huang K, Xie Z (2016) Induced membrane technique for the treatment of bone defects due to post-traumatic osteomyelitis. Bone Joint Res 5:101–105. https://doi.org/10.1302/2046–3758.53.2000487
Karger C, Kishi T, Schneider L, Fitoussi F, Masquelet AC, SOFCOT (2012) Treatment of posttraumatic bone defects by the induced membrane technique. Orthop Traumatol Surg Res 98:97–102. https://doi.org/10.1016/j.otsr.2011.11.001
Villemagne T, Bonnard C, Accadbled F, L'Kaissi M, de Billy B, Sales de Gauzy J (2011) Intercalary segmental reconstruction of long bones after malignant bone tumor resection using primary methyl methacrylate cement spacer interposition and secondary bone grafting: the induced membrane technique. J Pediatr Orthop 31:570–576. https://doi.org/10.1097/BPO.0b013e31821ffa82
Taylor BC, French BG, Fowler TT, Russell J, Poka A (2012) Induced membrane technique for reconstruction to manage bone loss. J Am Acad Orthop Surg 20:142–150. https://doi.org/10.5435/JAAOS-20-03-142
Masquelet AC, Fitoussi F, Begue T, Muller GP (2000) [Reconstruction of the long bones by the induced membrane and spongy autograft]. [Article in French] Ann Chir Plast Esthet 45:346–53
Kumar CY, Nalini KB, Menon J, Patro DK, Benerji BH (2013) Calcium sulfate as bone graft substitute in the treatment of osseous bone defects: a prospective study. J Clin Diagn Res 7(12):2926–2928. https://doi.org/10.7860/JCDR/2013/6404.3791
Andreacchio A, Alberghina F, Testa G, Canavese F (2017) Surgical treatment for symptomatic non-ossifying fibromas of the lower extremity with calcium sulphate grafts in skeletally immature patients. Eur J Orthop Surg Traumatol. https://doi.org/10.1007/s00590-017-2028-3
Helbig L, Simank HG, Lorenz H, Putz C, Wolfl C, Suda AJ et al (2014) Establishment of a new meticillin resistant staphylococcus aureus animal model of osteomyelitis. Int Orthop 38:891–897. https://doi.org/10.1007/s00264-013-2149-1
Christou C, Oliver RA, Yu Y, Walsh WR (2014) The Masquelet technique for membrane induction and the healing of ovine critical sized segmental defects. PLoS One 9(12):e114122. https://doi.org/10.1371/journal.pone.0114122
Winkler H (2017) Treatment of chronic orthopedic infection. EFORT Open Rev 2:110–116. https://doi.org/10.1302/2058–5241.2.160063
Mansour TM, Ghanem IB (2017) Preliminary results of the induced membrane technique for the reconstruction of large bone defects. J Pediatr Orthop 37:e67–e74. https://doi.org/10.1097/BPO.0000000000000663
Sasaki G, Watanabe Y, Miyamoto W, Yasui Y, Morimoto S, Kawano H (2017) Induced membrane technique using beta-tricalcium phosphate for reconstruction of femoral and tibial segmental bone loss due to infection: technical tips and preliminary clinical results. Int Orthop. https://doi.org/10.1007/s00264-017-3503-5
Buchholz HW, Gartmann HD (1972) [Infection prevention and surgical management of deep insidious infection in total endoprosthesis]. Chirurg 43:446–53
Buchholz HW, Engelbrecht H (1970) [Depot effects of various antibiotics mixed with Palacos resins]. [Article in German] Chirurg 41:511–5
Ogose A, Hotta T, Kawashima H, Kondo N, Ku W, Kamura T, Endo N (2005) Comparison of hydroxyapatite and beta tricalcium phosphate as bone substitutes after excision of bone tumors. J Biomed Mater Res B Appl Biomater 72:94–101. https://doi.org/10.1002/jbm.b.30136
Bassey LO, Antia-Obong OE, Antia UE (1995) Sequestrectomy and local muscle flap implantation for chronic osteomyelitis in children and adolescents. East Afr Med J 72:787–790
Kucukkaya M, Kabukcuoglu Y, Tezer M, Kuzgun U (2002) Management of childhood chronic tibial osteomyelitis with the Ilizarov method. J Pediatr Orthop 22:632–637
Paley D, Herzenberg JE (2002) Intramedullary infections treated with antibiotic cement rods: preliminary results in nine cases. J Orthop Trauma 16:723–729
Shrestha P, Mohan S, Roy S (2015) Bug on the back: vertebral osteomyelitis secondary to fluoroquinolone resistant salmonella typhi in an immunocompetent patient. BMJ Case Rep 27:2015. https://doi.org/10.1136/bcr-2015-212503
Unal VS, Dayican A, Demirel M, Portakal S, Ozkan G, Ucaner A (2006) [Selection of treatment modalities in children with chronic osteomyelitis]. [Article in Turkish] Acta Orthop Traumatol Turc 40:56–61
Hoang NT, Staudenmaier R, Feucht A, Hoehnke C (2009) Effectiveness of free gracilis muscle flaps in the treatment of chronic osteomyelitis with purulent fistulas at the distal third of the tibia in children. J Pediatr Orthop 29:305–311. https://doi.org/10.1097/BPO.0b013e31819903e1
Bar-On E, Weigl DM, Bor N, Becker T, Katz K, Mercado E, Livni G (2010) Chronic osteomyelitis in children: treatment by intramedullary reaming and antibiotic-impregnated cement rods. J Pediatr Orthop 30:508–513. https://doi.org/10.1097/BPO.0b013e3181e00e34
Mora Rios FG, Isunza Ramirez A, Lopez Marmolejo A, Palma Rosillo RM, Guízar Cuevas S, Mora Magaña I, Velásquez Pedroza VH (2010) [Sensitivity and specificity of the Tc-99m ciprofloxacin scan in pediatric osteomyelitis]. [Article in Spanish] Acta Orthop Mex 24:248–51
Feise RJ (2002) Do multiple outcome measures require p-value adjustment? BMC Med Res Methodol 2:8. https://doi.org/10.1186/1471-2288-2-8
Cohen J (1988) Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associate Publishers, Mahwah
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
No patients were involved. This is a retrospective study of patient’s data, and an IRB approval was obtained.
Additional information
Level of evidence: III
Rights and permissions
About this article
Cite this article
Rousset, M., Walle, M., Cambou, L. et al. Chronic infection and infected non-union of the long bones in paediatric patients: preliminary results of bone versus beta-tricalcium phosphate grafting after induced membrane formation. International Orthopaedics (SICOT) 42, 385–393 (2018). https://doi.org/10.1007/s00264-017-3693-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3693-x