Abstract
Purpose
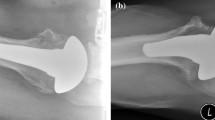
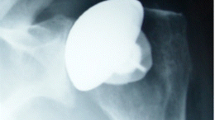
When the proximal humeral anatomy is altered because of malunion, shoulder arthroplasty is a challenge for the orthopaedic surgeon, and tuberosity osteotomy should be avoided whenever possible. The purpose of this study was to investigate the clinical and radiological outcomes of anatomic stemless shoulder arthroplasty in cases of malunion. We hypothesized that a stemless prosthesis can be implanted without performing tuberosity osteotomy.
Methods
We conducted a continuous, single surgeon, retrospective case series study with a minimum follow-up of two years (mean of 44 months, range 24–80). The Constant-Murley score, active range of motion and X-rays were evaluated in 27 patients (mean age of 60 years, range 37–83) with proximal humeral malunion who were treated with a stemless anatomic shoulder prosthesis.
Results
In all patients, the prosthesis was implanted without the need for tuberosity osteotomy. The Constant score improved from 27 to 62 (p ≤ 0.001), active anterior elevation from 81° to 129° (p ≤ 0.001), and external rotation from 5° to 40° (p ≤ 0.001). There was no evidence of radiological loosening.
Conclusions
Use of a stemless anatomic shoulder prosthesis avoids the need for tuberosity osteotomy and certain surgical difficulties, even in cases of severe tuberosity malunion, and leads to good functional outcomes in the short term.







Similar content being viewed by others
References
Boileau P, Trojani C, Walch G et al (2001) Shoulder arthroplasty for the treatment of the sequelae of fractures of the proximal humerus. J Shoulder Elbow Surg 10:299–308. doi:10.1067/mse.2001.115985
Mansat P, Guity MR, Bellumore Y, Mansat M (2004) Shoulder arthroplasty for late sequelae of proximal humeral fractures. J Shoulder Elbow Surg 13:305–312. doi:10.1016/S1058274604000370
Mansat P, Bonnevialle N (2015) Treatment of fracture sequelae of the proximal humerus: anatomical vs reverse shoulder prosthesis. Int Orthop 39:349–354. doi:10.1007/s00264-014-2651-0
Dines DM, Warren RF, Altchek DW, Moeckel B (1993) Posttraumatic changes of the proximal humerus: Malunion, nonunion, and osteonecrosis. Treatment with modular hemiarthroplasty or total shoulder arthroplasty. J Shoulder Elbow Surg 2:11–21. doi:10.1016/S1058-2746(09)80132-8
Willis M, Min W, Brooks JP et al (2012) Proximal humeral malunion treated with reverse shoulder arthroplasty. J Shoulder Elbow Surg 21:507–513. doi:10.1016/j.jse.2011.01.042
Neer CS 2nd (1970) Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 52:1077–1089
Antuña SA, Sperling JW, Sánchez-Sotelo J, Cofield RH (2002) Shoulder arthroplasty for proximal humeral malunions: long-term results. J Shoulder Elbow Surg 11:122–129
Beredjiklian PK, Iannotti JP (1998) Treatment of proximal humerus fracture malunion with prosthetic arthroplasty. Instr Course Lect 47:135–140
Boileau P, Chuinard C, Le Huec J-C et al (2006) Proximal humerus fracture sequelae: impact of a new radiographic classification on arthroplasty. Clin Orthop Relat Res 442:121–130
Brunner U, Köhler S (2007) Shoulder arthroplasty for treatment of the sequelae of proximal humerus fractures. Orthopade 36:1037–1049. doi:10.1007/s00132-007-1157-5
Ortmaier R, Resch H, Matis N et al (2013) Reverse shoulder arthroplasty in revision of failed shoulder arthroplasty-outcome and follow-up. Int Orthop 37:67–75. doi:10.1007/s00264-012-1742-z
Ballas R, Béguin L (2013) Results of a stemless reverse shoulder prosthesis at more than 58 months mean without loosening. J Shoulder Elbow Surg 22:e1–e6. doi:10.1016/j.jse.2012.12.005
Schnetzke M, Coda S, Walch G, Loew M (2015) Clinical and radiological results of a cementless short stem shoulder prosthesis at minimum follow-up of two years. Int Orthop 39:1351–1357. doi:10.1007/s00264-015-2770-2
Geurts GF, van Riet RP, Jansen N, Declercq G (2010) Placement of the stemless humeral component in the Total Evolutive Shoulder System (TESS). Tech Hand Up Extrem Surg 14:214–217. doi:10.1097/BTH.0b013e3181e397c5
Huguet D, DeClercq G, Rio B et al (2010) Results of a new stemless shoulder prosthesis: radiologic proof of maintained fixation and stability after a minimum of three years’ follow-up. J Shoulder Elbow Surg 19:847–852. doi:10.1016/j.jse.2009.12.009
Atoun E, Van Tongel A, Hous N et al (2014) Reverse shoulder arthroplasty with a short metaphyseal humeral stem. Int Orthop 38:1213–1218. doi:10.1007/s00264-014-2328-8
Teissier P, Teissier J, Kouyoumdjian P, Asencio G (2014) The TESS reverse shoulder arthroplasty without a stem in the treatment of cuff-deficient shoulder conditions: clinical and radiographic results. J Shoulder Elbow Surg 24(1):45–51. doi:10.1016/j.jse.2014.04.005
Kadum B, Hassany H, Wadsten M et al (2015) Geometrical analysis of stemless shoulder arthroplasty: a radiological study of seventy TESS total shoulder prostheses. Int Orthop. doi:10.1007/s00264-015-2935-z
Acknowledgments
Lucie Pautet, Ph.D., from The Comprehensive Nuclear-Test-Ban Treaty Organization (CTBTO), is acknowledged for technical help.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Not applicable. French law does not provide for consultation of an ethics committee for non-interventional biomedical research (Article L1121-1 of the Code of Public Health).
Conflict of interest
Richard Ballas and Philippe Teissier have no competing interests to declare. Dr Jacques Teissier received Royalties and Personal Fees from Biomet Compagny, Warsaw, Indiana, which is related to the subject of this work.
Rights and permissions
About this article
Cite this article
Ballas, R., Teissier, P. & Teissier, J. Stemless shoulder prosthesis for treatment of proximal humeral malunion does not require tuberosity osteotomy. International Orthopaedics (SICOT) 40, 1473–1479 (2016). https://doi.org/10.1007/s00264-016-3138-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3138-y