Abstract
Purpose
The purpose of the study was to evaluate the influence of β-tricalcium phosphate (β-TCP) content on absorption rate and osteoconductive behavior of β-TCP/poly-L-lactic acid (PLLA) interference screws for anterior cruciate ligament (ACL) reconstruction. The authors compared two biocomposite β-TCP/PLLA screws containing 30 % (30TCP) and 60 % (60TCP) β-TCP (Ligafix®, SBM), respectively, used in ACL reconstruction with patellar tendon (BPTB) and hamstrings (HS) autografts.
Methods
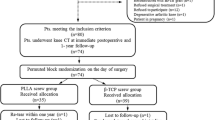
Twenty-eight knees with a 30TCP screw and 25 knees with a 60TCP screw were retrospectively included. Mean follow-up period was 37.5 months (range, 29–45 months). Post-operatively, all patients were examined clinically, had stress X-rays to measure anterior tibial translation and computed tomography (CT) to determine screw tract density, osteoconductivity and completed functional scores.
Results
Clinical evaluation and functional scores were similar for both groups. There was no case of tunnel widening, cyst formation, increased inflammatory process or osteolysis. Both types of screws evidenced a decrease of Hounsfield units (HU) density over time (p < 0.001). The 60TCP screw resorbed more rapidly than the 30TCP (−62 vs –52 % of initial HU density respectively, p < 0.01) at latest follow-up. At three years, 97 % of the 30TCP and 96 % of the 60TCP screws showed osteoconductivity according to the Barber-Dockery’s architectural score.
Conclusions
Both types of screws showed considerable osteoconductivity at the site of the screw tract. The majority of the 30 % β-TCP screws were fully resorbed and osteointegrated during the fourth postoperative year. The clinical results are good-to-excellent for both groups. The addition of 30 % or 60 % β-TCP in the biocomposite screw did not adversely affect clinical outcome and it minimized the inflammatory process. The material with the highest β-TCP content was absorbed more rapidly, supporting the hypothesis that increased β-TCP content in β-TCP/PLLA biocomposite material resulted in enhanced absorption rate of interference screws used in ACL reconstruction without affecting fixation strength.
Level of Evidence
Level IV, Therapeutic case series





Similar content being viewed by others
References
Luhmann SJ, Schoenecker PL, Dobbs MB, Gordon JE (2007) Arthroscopic findings at the time of patellar realignment surgery in adolescents. J Pediatr Orthop 27(5):493–498
Spindler KP, Wright RW (2008) Clinical practice. Anterior cruciate ligament tear. N Engl J Med 359(20):2135–2142
Kartus J, Magnusson L, Stener S, Brandsson S, Eriksson BI, Karlsson J (1999) Complications following arthroscopic anterior cruciate ligament reconstruction. A 2-5-year follow-up of 604 patients with special emphasis on anterior knee pain. Knee Surg Sports Traumatol Arthrosc 7(1):2–8
Li S, Chen Y, Lin Z, Cui W, Zhao J, Su W (2012) A systematic review of randomized controlled clinical trials comparing hamstring autografts versus bone-patellar tendon-bone autografts for the reconstruction of the anterior cruciate ligament. Arch Orthop Trauma Surg 132(9):1287–1297
Safran MR, Greene HS (2006) Avoidance and management of intra-articular complications of anterior cruciate ligament reconstruction. Instr Course Lect 55:475–488
Tjoumakaris FP, Herz-Brown AL, Bowers AL, Sennett BJ, Bernstein J (2012) Complications in brief: Anterior cruciate ligament reconstruction. Clin Orthop Relat Res 470(2):630–636
Hoxie SC, Dobbs RE, Dahm DL, Trousdale RT (2008) Total knee arthroplasty after anterior cruciate ligament reconstruction. J Arthroplasty 23(7):1005–1008
Magnussen RA, Demey G, Lustig S, Servien E, Neyret P (2012) Total knee arthroplasty for secondary osteoarthritis following ACL reconstruction: a matched-pair comparative study of intra-operative and early post-operative complications. Knee 19(4):275–278
Kamath GV, Redfern JC, Greis PE, Burks RT (2011) Revision anterior cruciate ligament reconstruction. Am J Sports Med 39(1):199–217
Cheatham SA, Johnson DL (2013) Anticipating problems unique to revision ACL surgery. Sports Med Arthrosc 21(2):129–134
Thomas NP, Kankate R, Wandless F, Pandit H (2005) Revision anterior cruciate ligament reconstruction using a 2-stage technique with bone grafting of the tibial tunnel. Am J Sports Med 33(11):1701–1709
Coats AC, Johnson DL (2012) Two-stage revision anterior cruciate ligament reconstruction: indications, review, and technique demonstration. Orthopedics 35(11):958–960
Barber FA, Dockery WD (2008) Long-term absorption of beta-tricalcium phosphate poly-L-lactic acid interference screws. Arthroscopy 24(4):441–447
Drogset JO, Grontvedt T, Myhr G (2006) Magnetic resonance imaging analysis of bioabsorbable interference screws used for fixation of bone-patellar tendon-bone autografts in endoscopic reconstruction of the anterior cruciate ligament. Am J Sports Med 34(7):1164–1169
Emond CE, Woelber EB, Kurd SK, Ciccotti MG, Cohen SB (2011) A comparison of the results of anterior cruciate ligament reconstruction using bioabsorbable versus metal interference screws: a meta-analysis. J Bone Joint Surg Am 93(6):572–580
Johnston M, Morse A, Arrington J, Pliner M, Gasser S (2011) Resorption and remodeling of hydroxyapatite-poly-L-lactic acid composite anterior cruciate ligament interference screws. Arthroscopy 27(12):1671–1678
Lind M, Feller J, Webster KE (2009) Tibial bone tunnel widening is reduced by polylactate/hydroxyapatite interference screws compared to metal screws after ACL reconstruction with hamstring grafts. Knee 16(6):447–451
Konan S, Haddad FS (2009) A clinical review of bioabsorbable interference screws and their adverse effects in anterior cruciate ligament reconstruction surgery. Knee 16(1):6–13
Barber FA, Dockery WD (2006) Long-term absorption of poly-L-lactic Acid interference screws. Arthroscopy 22(8):820–826
Warden WH, Chooljian D, Jackson DW (2008) Ten-year magnetic resonance imaging follow-up of bioabsorbable poly-L-lactic acid interference screws after anterior cruciate ligament reconstruction. Arthroscopy 24(3):370–e371-373
Mastrokalos DS, Paessler HH (2008) Allergic reaction to biodegradable interference poly-L-lactic acid screws after anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft. Arthroscopy 24(6):732–733
Agrawal CM, Athanasiou KA (1997) Technique to control pH in vicinity of biodegrading PLA-PGA implants. J Biomed Mater Res 38(2):105–114
Aunoble S, Clement D, Frayssinet P, Harmand MF, Le Huec JC (2006) Biological performance of a new beta-TCP/PLLA composite material for applications in spine surgery: in vitro and in vivo studies. J Biomedical Mater Res Part A 78(2):416–422
Weimann A, Rodieck M, Zantop T, Hassenpflug J, Petersen W (2005) Primary stability of hamstring graft fixation with biodegradable suspension versus interference screws. Arthroscopy 21(3):266–274
Macarini L, Milillo P, Mocci A, Vinci R, Ettorre GC (2008) Poly-L-lactic acid–hydroxyapatite (PLLA-HA) bioabsorbable interference screws for tibial graft fixation in anterior cruciate ligament (ACL) reconstruction surgery: MR evaluation of osteointegration and degradation features. Radiol Med 113(8):1185–1197
Hunt JA, Callaghan JT (2008) Polymer-hydroxyapatite composite versus polymer interference screws in anterior cruciate ligament reconstruction in a large animal model. Knee Surg Sports Traumatol Arthrosc 16(7):655–660
Laxdal G, Kartus J, Eriksson BI, Faxen E, Sernert N, Karlsson J (2006) Biodegradable and metallic interference screws in anterior cruciate ligament reconstruction surgery using hamstring tendon grafts: prospective randomized study of radiographic results and clinical outcome. Am J Sports Med 34(10):1574–1580
Stener S, Ejerhed L, Sernert N, Laxdal G, Rostgard-Christensen L, Kartus J (2010) A long-term, prospective, randomized study comparing biodegradable and metal interference screws in anterior cruciate ligament reconstruction surgery: radiographic results and clinical outcome. Am J Sports Med 38(8):1598–1605
Tecklenburg K, Burkart P, Hoser C, Rieger M, Fink C (2006) Prospective evaluation of patellar tendon graft fixation in anterior cruciate ligament reconstruction comparing composite bioabsorbable and allograft interference screws. Arthroscopy 22(9):993–999
Nyland J, Kocabey Y, Caborn DN (2004) Insertion torque pullout strength relationship of soft tissue tendon graft tibia tunnel fixation with a bioabsorbable interference screw. Arthroscopy 20(4):379–384
Shen C, Jiang SD, Jiang LS, Dai LY (2010) Bioabsorbable versus metallic interference screw fixation in anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials. Arthroscopy 26(5):705–713
Homaeigohar S, Shokrgozar MA, Khavandi A, Sadi AY (2008) In vitro biological evaluation of beta-TCP/HDPE–A novel orthopedic composite: a survey using human osteoblast and fibroblast bone cells. J Biomedical Mater Res Part A 84(2):491–499
Prado RK, Ntagiopoulos PG, Fucs PM, Severino NR, Dejour D (2012) A new technique in double-bundle anterior cruciate ligament reconstruction using implant-free femoral fixation. Int Orthop 36(7):1479–1485, discussion 1539–1441
Dejour D, Ferrua P, Bonin N, Saggin PR (2012) Double-bundle bone-patellar tendon-bone and gracilis in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 20(11):2239–2242
Hounsfield GN (1973) Computerized transverse axial scanning (tomography). 1. Description of system. Br J Radiol 46(552):1016–1022
Kobayashi M, Nakagawa Y, Suzuki T, Okudaira S, Nakamura T (2006) A retrospective review of bone tunnel enlargement after anterior cruciate ligament reconstruction with hamstring tendons fixed with a metal round cannulated interference screw in the femur. Arthroscopy 22(10):1093–1099
Fauno P, Kaalund S (2005) Tunnel widening after hamstring anterior cruciate ligament reconstruction is influenced by the type of graft fixation used: a prospective randomized study. Arthroscopy 21(11):1337–1341
Chhabra A, Kline AJ, Nilles KM, Harner CD (2006) Tunnel expansion after anterior cruciate ligament reconstruction with autogenous hamstrings: a comparison of the medial portal and transtibial techniques. Arthroscopy 22(10):1107–1112
Barrett GR, Brown TD (2007) Femoral tunnel defect filled with a synthetic dowel graft for a single-staged revision anterior cruciate ligament reconstruction. Arthroscopy 23(7):796–e791-794
Radford MJ, Noakes J, Read J, Wood DG (2005) The natural history of a bioabsorbable interference screw used for anterior cruciate ligament reconstruction with a 4-strand hamstring technique. Arthroscopy 21(6):707–710
Jarvela T, Moisala AS, Sihvonen R, Jarvela S, Kannus P, Jarvinen M (2008) Double-bundle anterior cruciate ligament reconstruction using hamstring autografts and bioabsorbable interference screw fixation: prospective, randomized, clinical study with 2-year results. Am J Sports Med 36(2):290–297
Conflict of interest
Dr. David Dejour receives royalty fees from SBM. The other authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ntagiopoulos, P.G., Demey, G., Tavernier, T. et al. Comparison of resorption and remodeling of bioabsorbable interference screws in anterior cruciate ligament reconstruction. International Orthopaedics (SICOT) 39, 697–706 (2015). https://doi.org/10.1007/s00264-014-2530-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2530-8