Abstract
Purpose
This study investigated the efficacy of platelet-rich plasma (PRP) on articular surfaces on which the mosaicplasty technique was performed. Our hypothesis was that PRP can accelerate the osseointegration process and enhance the quality of articular integrity after the mosaicplasty procedure.
Methods
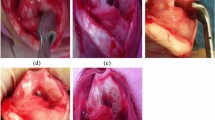
Standard defects were created in the femoral groove of both patellofemoral joints of 12 New Zealand rabbits. PRP solution was placed inside the defect before fixation of the osteochondral autografts and injected inside the involved joint after capsular closure of the tested knees. The contralateral knees served as the control sides. The animals were euthanized three or six weeks after mosaicplasty, and both limbs were assessed according to Pineda’s histological grading scale. Significance level was set at p ≤ 0.05 a priori, and the Mann–Whitney U test was used for statistical analysis.
Results
Histologic findings at the interface between the transferred autograft and the original cartilage revealed better integration of the adjacent surfaces in the mosaicplasty with PRP group three weeks after the procedure; the difference was significant (p < 0.05). However, no significant difference in the transition zone was observed between the groups six weeks after the experiment (p = 0.59).
Conclusions
Our animal model showed that adjunctive use of PRP produced a better healing response and resulted in superior histological scores after three weeks compared with the mosaicplasty-only procedure. Interpretation of our results is important in terms of rapid return to previous activity levels. Thus, application of PRP can represent a valid therapeutic option for improving the efficacy of mosaicplasty by stimulating the local healing response.








Similar content being viewed by others
References
Heir S, Nerhus TK, Rotterud JH, Loken S, Ekeland A, Engebretsen L, Aroen A (2010) Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med 38(2):231–237
Buckwalter JA, Mankin HA (1998) Articular cartilage repair and transplantation. Arthritis Rheum 41:1331–1342
Bartlett W, Skinner JA, Gooding CR, Carrington RW, Flanagan AM, Briggs TW, Bentley G (2005) Autologous chondrocyte implantation versus matrix-induced autologous chondrocyte implantation for osteochondral defects of the knee: a prospective, randomised study. J Bone Joint Surg Br 87(5):640–645
Bentley G, Biant LC, Carrington RW, Akmal M, Goldberg A, Williams AM, Skinner JA, Pringle J (2003) A prospective, randomised comparison of autologous chondrocyte implantation versus mosaicplasty for osteochondral defects in the knee. J Bone Joint Surg Br 85(2):223–230
Steadman JR, Rodkey WG, Briggs KK, Rodrigo JJ (1999) The microfracture technic in the management of complete cartilage defects in the knee joint. Orthopade 28:26e32
Peterson L, Brittberg M, Kiviranta I, Akerlund EL, Lindahl A (2002) Autologous chondrocyte transplantation. Biomechanics and long-term durability. Am J Sports Med 30:2e12
Altan E, Senaran H, Acar MA, Aydın K, Ozbaydar MU (2013) Mozaicplasty technique for treatment of reverse Hill-Sachs lesion. Tech Should Elbow Surg 14:1–4. doi:10.1097/BTE.0b013e318274962c
Marcacci M, Kon E, Zaffagnini S, Iacono F, Neri MP, Vascellari A et al (2005) Multiple osteochondral arthroscopic grafting (mosaicplasty) for cartilage defects of the knee: prospective study results at 2-year follow-up. Arthroscopy 21(4):462–470
Borzini P, Mazzucco L (2005) Tissue regeneration and in loco administration of platelet derivatives: clinical outcome, heterogeneous products, and heterogeneity of the effector mechanisms. Transfusion 45:1759e67
Borazjani BH, Chen AC, Bae WC et al (2006) Effect of impact on chondrocyte viability during insertion of human osteochondral grafts. J Bone Joint Surg Am 88(9):1934–1943
Gulotta LV, Rudzki JR, Kovacevic D, Chen CC, Milentijevic D, Williams RJ 3rd (2009) Chondrocyte death and cartilage degradation after autologous osteochondral transplantation surgery in a rabbit model. Am J Sports Med 37(7):1324–1333
Hangody L, Kish G, Karapati Z, Eberhart R (1997) Osteochondral plugs: Autogenous osteochondral mosaicplasty for the treatment of focal chondral and osteochondral articular defects. Oper Tech Orthop 7:312–322
Pecina M, Jelic M, Martinovic S, Haspl M, Vukicevic S (2002) Articular cartilage repair: the role of bone morphogenetic proteins. Int Orthop 26:131–136
Borovecki F, Pecina Slaus N, Vukicevic S (2007) Biological mechanisms of bone and cartilage remodelling-genomic perspective. Int Orthop 31:799–805
Griffin XL, Smith CM, Costa ML (2009) The clinical use of platelet rich plasma in the promotion of bone healing: A systematic review. Injury 40:158–162
Akeda K, An HS, Okuma M, Attawia M, Miyamoto K, Thonar EJ et al (2006) Platelet-rich plasma stimulates porcine articular chondrocyte proliferation and matrix biosynthesis. Osteoarthr Cartil 14:1272–1280
Wu W, Chen F, Liu Y, Ma Q, Mao T (2007) Autologous injectable tissue-engineered cartilage by using platelet-rich plasma: Experimental study in a rabbit model. J Oral Maxillofac Surg 65:1951–1957
Dold A, Zywiel M, Taylor DW, Dwyer T, Theodoropoulos J (2014) Platelet-rich plasma in the management of articular cartilage pathology: a systematic review. Clin J Sport Med 24(1):31–43. doi:10.1097/01.jsm.0000432855.85143.e5
Sun Y, Feng Y, Zhang CQ, Chen SB, Cheng XG (2010) The regenerative effect of platelet-rich plasma on healing in large osteochondral defects. Int Orthop 34(4):589–597
Nam EK, Makhsous M, Koh J, Bowen M, Nuber G, Zhang LQ (2004) Biomechanical and histological evaluation of osteochondral transplantation in a rabbit model. Am J Sports Med 32(2):308–316
Wakitani S, Goto T, Pineda SJ, Young RG, Mansour JM, Caplan AI et al (1994) Mesenchymal cell-based repair of large, full-thickness defects of articular cartilage. J Bone Joint Surg Am 76:579–592
DeLong JM, Russell RP, Mazzocca AD (2012) Platelet-rich plasma: the PAW classification system. Arthroscopy 28(7):998–1009
Saito M, Takahashi KA, Arai Y, Inoue A, Sakao K, Tonomura H et al (2009) Intraarticular administration of platelet-rich plasma with biodegradable gelatin hydrogel microspheres prevents osteoarthritis progression in the rabbit knee. Clin Exp Rheumatol 27:201–207
Milano G, Deriu L, Passino ES, Masala G, Manunta A, Postacchini R et al (2012) Repeated platelet concentrate injections enhance reparative response of microfractures in the treatment of chondral defects of the knee: an experimental study in an animal model. Arthroscopy 28(5):688–701
O’Driscoll SW, Keeley FW, Salter RB (1986) The chondrogenic potential of free autogenous periosteal grafts for biological resurfacing of major full-thickness defects in joint surfaces under the influence of continuous passive motion. J Bone Joint Surg Am 68(7):1017–1035
Drengk A, Zapf A, Sturmer EK, Sturmer KM, Frosch KH (2009) Influence of platelet-rich plasma on chondrogenic differentiation and proliferation of chondrocytes and mesenchymal stem cells. Cells Tissues Organs 189(5):317–326
Whiteside RA, Jakob RP, Wyss UP, Mainil-Varlet P (2005) Impact loading of articular cartilage during transplantation of osteochondral autograft. J Bone Joint Surg Br 87(9):1285–1291
Baumbach K, Petersen JP, Ueblacker P et al (2008) The fate of osteochondral grafts after autologous osteochondral transplantation: a one-year follow-up study in a minipig model. Arch Orthop Trauma Surg 128:1255–1263
Tibesku CO, Szuwart T, Kleffner TO et al (2004) Hyaline cartilage degenerates after autologous osteochondral transplantation. J Orthop Res 22(6):1210–1214
Hurtig M, Pearce S, Warren S, Kalra M, Miniaci A (2001) Arthroscopic mosaic arthroplasty in the equine third carpal bone. Vet Surg 30:228–239
Chen L, Yang X, Huang G et al (2013) Platelet-rich plasma promotes healing of osteoporotic fractures. Orthopedics 36(6):e687–e694
Arpornmaeklong P, Kochel M, Depprich R, Kübler NR, Würzler KK (2004) Influence of platelet-rich plasma (PRP) on osteogenic differentiation of rat bone marrow stromal cells. An in vitro study. Int J Oral Maxillofac Surg 33(1):60–70
Dallari D, Savarino L, Stagni C et al (2007) Enhanced tibial osteotomy healing with use of bone grafts supplemented with platelet gel or platelet gel and bone marrow stromal cells. J Bone Joint Surg Am 89:2413–2420
Castricini R, Longo U, de Benedetto M et al (2011) Platelet-rich plasma augmentation for arthroscopic rotator cuff repair: A randomized controlled trial. Am J Sports Med 39:258–265
Mishra A, Tummala P, King A, Lee B, Kraus M, Tse V et al (2009) Buffered platelet-rich plasma enhances mesenchymal stem cell proliferation and chondrogenic differentiation. Tissue Eng Part C Methods 15:431–435
Milano G, Passino ES, Deriu L et al (2010) The effect of platelet rich plasma combined with microfractures on the treatment of chondral defects: An experimental study in a sheep model. Osteoarthritis Cartilage 18:971–980
Qi YY, Chen X, Jiang YZ et al (2009) Local delivery of autologous platelet in collagen matrix simulated in situ articular cartilage repair. Cell Transplant 18:1161–1169
Kon E, Filardo G, Delcogliano M et al (2010) Platelet autologous growth factors decrease the osteochondral regeneration capability of a collagen-hydroxyapatite scaffold in a sheep model. BMC Musculoskelet Disord 11:220
Brehm W, Aklin B, Yamashita T et al (2006) Repair of superficial osteochondral defects with an autologous scaffold-free cartilage construct in a caprine model: implantation method and short-term results. Osteoarthritis Cartilage 14:1214–1226
Weibrich G, Kleis WK, Hitzler WE, Hafner G (2005) Comparison of the platelet concentrate collection system with the plasma-rich-in-growth-factors kit to produce platelet-rich plasma: a technical report. Int J Oral Maxillofac Implants 20:118e23
Leitner GC, Gruber R, Neumüller J, Wagner A, Kloimstein P, Höcker P et al (2006) Platelet content and growth factor release in platelet-rich plasma: a comparison of four different systems. Vox Sang 91:135–139
Pettersson S, Wetterö J, Tengvall P, Kratz GJ (2009) Human articular chondrocytes on macroporous gelatin microcarriers form structurally stable constructs with blood-derived biological glues in vitro. Tissue Eng Regen Med 3(6):450–460
Sheth U, Simunovic N, Klein G et al (2012) Efficacy of autologous platelet-rich plasma use for orthopaedic indications: A meta-analysis. J Bone Joint Surg Am 94:298–307
Marx RE (2004) Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg 62:489–496
Hui JH, Chen F, Thambyah A, Lee EH (2004) Treatment of chondral lesions in advanced osteochondritis dissecans: a comparative study of the efficacy of chondrocytes, mesenchymal stem cells, periosteal graft, and mosaicplasty (osteochondral autograft) in animal models. J Pediatr Orthop 24(4):427–433
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Altan, E., Aydin, K., Erkocak, O. et al. The effect of platelet-rich plasma on osteochondral defects treated with mosaicplasty. International Orthopaedics (SICOT) 38, 1321–1328 (2014). https://doi.org/10.1007/s00264-013-2275-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-2275-9