Abstract
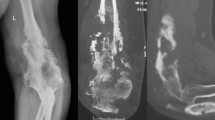
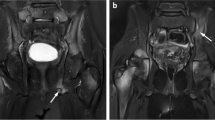
In the evidence-based medicine era, objective treatment guidelines have been laid down for pulmonary tuberculosis, but the same is not true for osteoarticular tuberculosis. This has led to demands for standardising the treatment protocol and to a lack of consensus between doctors regarding the composition and duration of treatment. Twenty-five patients with extraspinal osteoarticular tuberculosis were evaluated prospectively. Following the diagnosis, patients were given standard directly observed treatment short course (DOTS) regimen and were monitored for disease activity at zero, three and six months with the help of technetium-99m-labelled ciprofloxacin (99m Tc) scan. Tracer activity at the site was recorded and compared on sequential scans. Clinical and radiological profile of all the patients were also recorded at regular intervals and compared. All 25 cases had a positive 99mTc bone scan initially. Four patients (16%) converted to negative scans at three months, whereas the remaining 21 patients (84%) showed negative scans at six months. The end of six months therapy also coincided with resolution of clinical and radiological parameters in all cases. In conclusion, 99mTc scan is a promising tool for monitoring drug response in osteoarticular tuberculosis; however, due to the small sample size, studies with a large number of patients might be of help.

Similar content being viewed by others
References
Dye C, Garnett GP, Sleeman K, Williams BG (1998) Prospects for worldwide tuberculosis control under the WHO DOTS strategy. Lancet 352:1886–1891
Nakajima H (1993) Tuberculosis a global emergency. World Health 46(4):3
Tuli SM (2004) Tuberculosis of the Skeletal System, (third ed); 3-4
Masood S (1992) Diagnosis of tuberculosis of the bone and soft tissue by fine-needle aspiration biopsy. Diagn Cytopathol 8:451–455
World Health Organization: treatment of tuberculosis. Guidelines for national programs Ed 2, Geneva, World Health Organization 1997
Glassroth J (2000) Clinical considerations in designing trials of vaccines for tuberculosis. Clin Infect Dis 30(Suppl 3):S229–S232
Mitchison DA, Ellard GA, Fox W (1999) Studies on the treatment of tuberculosis undertaken by the British Medical Research Council Tuberculosis Unit between 1946-86. Int J Tuberc Lung Dis 10:231–279
Balasubramanian R (1991) Fully intermittent six-month treatment regimen for pulmonary tuberculosis in south India. Ind J Tuberc 38:51–53
MRC Working Party on Tuberculosis of the Spine (1993) Controlled trial of short-course regimens of chemotherapy in the ambulatory treatment of spinal tuberculosis results at three years of a study in Korea twelfth report of the medical research council working party on tuberculosis of the spine. J Bone Joint Surg Br 75:240–248
MRC Working Party on Tuberculosis of the Spine (1999) Five-year assessment of controlled trials of short-course chemotherapy regimens of 6, 9 or 18 months’ duration for spinal tuberculosis in patients ambulatory from the start or undergoing radical surgery Fourteenth report of the Medical Research Council Working Party on Tuberculosis of the Spin. Int Orthop 23(2):73–81
Ramachandran S, Clifton IJ, Collyns TA, Watson JP SB (2006) 6-month treatment for bone tuberculosis. Int J Tuberc Lung Dis 10(9):1063–1065
Yoon HJ, Song YG, Park WI, Choi JP, Chang KH, Kim JM (2004) Clinical manifestations and diagnosis of extrapulmonary tuberculosis. Yonsei Med J 45(3):453–461
Martini M, Cuahes M (1988) Bone and joint tuberculosis: a review of 652 cases. Orthopedics 11:861–866
Maekura R, Nakagawa M, Nakamura Y, Hiraga T, Yamamura Y, Ito M, Ueda E, Yano S, He H, Oka S et al (1993) Clinical evaluation of rapid serodiagnosis of pulmonary tuberculosis by ELISA with cord factor (trehalose-6,6'-dimycolate) as antigen purified from Mycobacterium tuberculosis. Am Rev Respir Dis 148:997–1001
Chiac P, Yen TSB, You JB, Maa JS, Fiss EH, Chang CH (1990) Detection and identification of Mycobacterium tuberculosis by DNA amplification. J Clin Microb 28:1877–1880
Noel AB, Lecossier D, Nassif X, Birgite G, Frebault VL, Hance AJ (1989) Rapid diagnosis of tuberculosis by amplification of mycobacterial DNA in clinical samples. Lancet 2(8671):1069–1071
Pandey V, Chawla K, Acharya K, Rao S, Rao S (2009) The role of polymerase chain reaction in the management of osteoarticular tuberculosis. Int Orthop 33(3):801–805
Soler R, Rodriguez E, Remuinan C, Santos M (2001) MRI of musculoskeletal extraspinal tuberculosis. J Computer Assisted Tomography 25(2):177–183
Vuyst D, Vanhoenacker F, Gielen J, Bernaerts A, De Schepper AM (2003) Imaging features of musculoskeletal tuberculosis. European Radiology.; 13:1809-1819
Britton KE, Vinjamuri S, Hall AV et al (1997) Clinical evaluation of technetium-99 m Infecton for the localization of bacterial infection. Eur J Nucl Med 24:553–556
Hall AV, Solanki KK, Vinjamuri S, Britton KE, Das SS (1998) Evaluation of the efficacy of 99mTc-Infecton, a novel agent for detecting sites of infection. J Clin Pathol 51:215–219
Britton KE, Wareham DW, Das SS, Solanki KK, Amaral H, Bhatnagar A, Katamihardja AHS, Malamitsi J, Moustafa HM, Soroa VE, Sundram FX, Padhy AK (2002) Imaging bacterial infection with 99mTc-ciprofloxacin (Infecton). J Clin Path 55:817–823
Vinjamuri S, Hall AV, Solanki KK et al (1996) Comparison of 99mTc Infecton imaging with radiolabeled white-cell imaging in the evaluation of bacterial infection. Lancet 347:233–235
Easmon CSF, Crane JP, Browers A (1986) Effect of ciprofloxacin on intracellular organism in-vitro and in-vivo studies. J of Antimicrob Chemotherapy 18(suppl):46–48
Sharma R, Tewari KN, Bhatnagar A, Mondal A, Mishra AK, Singh AK, Chopra MK, Rawat H, Kashyap R, Tripathi RP (2007) Tc-99 m ciprofloxacin scans for detection of tubercular bone infection. Clin Nucl Med 32(5):367–370
Conflict of Interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bhardwaj, V., Agrawal, M., Suri, T. et al. Evaluation of adequacy of short-course chemotherapy for extraspinal osteoarticular tuberculosis using 99mTc ciprofloxacin scan. International Orthopaedics (SICOT) 35, 1869–1874 (2011). https://doi.org/10.1007/s00264-010-1162-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-1162-x