Abstract
Operative treatment of prepatellar bursitis is indicated in intractable bursitis. The most common complication of surgical treatment for prepatellar bursitis is skin problems. For traumatic prepatellar bursitis, we propose a protocol of outpatient endoscopic surgery under local anaesthesia. From September 1996 to February 2001, 60 cases of failed nonoperative treatment for prepatellar bursitis were included. The average age was 33.5 ± 11.1 years (range 21–55). The average operation duration was 18 minutes. Two to three mini-arthroscopic portals were used in our series. No sutures or a simple suture was needed for the portals after operation. After follow-up for an average of 36.3 months, all patients are were symptom-free and had regained knee function. None of the population had local tenderness or hypo-aesthesia around their wound. Their radiographic and sonographic examinations showed no recurrence of bursitis. Outpatient arthroscopic bursectomy under local anaesthesia is an effective procedure for the treatment of post-traumatic prepatellar bursitis after failed conservative treatments. Both the cosmetic results and functional results were satisfactory.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prepatellar bursa is located subcutaneously and is present in most people. Various aetiologies have been proposed as the cause of prepatellar bursitis [1–9]. Chronic inflammation of prepatellar bursa after repetitive minor trauma, so called “housemaid’s knee”, can be seen in those whose occupations require a kneeling posture, such as carpet layers and housemaids. Acute trauma, such as a fall directly onto the patella, may cause patellar bursitis [6]. The other causes of prepatellar bursitis include infection or low-grade inflammatory conditions, such as gout, syphilis, tuberculosis, or rheumatoid arthritis. Treatment for prepatellar bursitis is determined primarily by the cause of bursitis and secondarily by the pathological change in the bursa [3]. Surgery is not required in most instances; but, if needed, the surgical procedures involved are (1) aspiration and irrigation with an appropriate drug [10], (2) incision and drainage in cases of acute suppurative bursitis [11, 12], and (3) excision of chronically infected and thickened bursa [3, 7–9, 11–16]. For the last category of patients, we usually make a transverse incision at the anterior knee region under regional or general anaesthesia, which entails admission to hospital and leaves poor cosmetic results. The resultant skin problems cause suffering in some cases. In this study, we propose an out-patient arthroscopic method under local anaesthesia aiming at a better cosmetic appearance and cost savings for the treatment of chronic prepatellar bursitis. We presume that the results of the endoscopic approach would be better than those obtained with the conventional technique.
Materials and methods
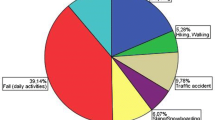
From September 1996 to February 2001, 60 patients (31 male and 29 female) with prepatellar bursitis who had failed to respond to non-operative treatments were included in this prospective study. Patients who presented with acute suppurative infection, systemic diseases (such as rheumatoid arthritis, gout, tuberculosis, diabetic mellitus, bleeding tendencies, etc.), alcoholism, or steroid therapy were excluded from our series. Only those who had repeated minor injuries or an apparent trauma of the ipsilateral knee were included. The average age was 33.5 ± 11.1 years (range 21–55). Twenty-seven patients (45%) had a history of repeated minor knee injuries without apparent underlying cause. There were housewives, farmers, construction workers, fishermen, electronic technicians, athletes, engineers, and teachers. The repeated minor injuries were due to occupations or lifestyles in which they were frequently required to kneel. The other cases had a clear history of trauma. The mechanisms were motorcycle accidents and histories of falling down while running in the office, during matches, or while jogging, and after a contusion caused by contact with a hard object. All these patients had histories of undergoing aspiration of fluid or injection of steroid into prepatellar bursa cavities at our hospital or the other clinics. The diagnosis was based mainly on clinical examination, history, and sonographic examination. Radiographic examination included plain films of an anteroposterior and a lateral view of the knee. MRI (magnetic resonance image) or CT (computerised tomography) was not used routinely. Aspiration was performed to rule out active infection and all samples were cultured. If the culture was positive for bacterial growth, the patients were excluded from the study. Once the patients proved unresponsive to aspiration, endoscopy was immediately arranged.
Operative technique
Patients were placed in a supine position. The tourniquet was routinely applied on the thigh and was not inflated until necessary. The skin was prepared in an aseptic manner over the whole lower extremity. A 1% xylocaine with a 1:100,000 epinephrine solution was infiltrated at the portal site and then into the cavity. A 2.7-mm diameter, 30-degree endoscope was used for monitoring. A 2.7-mm motorised shaver was used to remove thickened synovium. Two or three 2 mm portals were made (Fig. 1). An anterior medial portal and an anterior lateral portal were routinely used; and, if necessary, a superior lateral portal was also made. A no. 11 scalpel was used to create a 2-mm incision for each portal. Then the trochar was inserted into the cavity and the instruments followed. The bursa cavity and synovial thickening were directly visualised by endoscopy. The motorised shaver was inserted through the other portal, and total synovectomy (including the bursa) was performed until all the pathological lesions were removed (Fig. 2). After all the procedures were completed, the portals were closed with adhesive tape without any suture. The anterior knee area was dressed with loosely unfolded gauze and padding and bandage applied.
Postoperative care
No hospitalisation was needed. Patients went home immediately after surgery. No antibiotic was needed either before or after operation. Nonsteroidal anti-inflammatory drugs (NSAID) were given and ice packing was applied for the first 48 hours. No vigorous activity was allowed in the first two weeks. The wounds were not inspected until 48 hours later. An elastic compression bandage was applied to the knee in the first week. Patients returned to normal activities from the third postoperative week.
Follow-up
We evaluated the patients by recording swelling, pain, activities, and range of motion of their knee every month. Radiographic and sonographic examinations were made at the first and third months and every three months after operation.
Results
The average time for follow-up was 45.3 ± 14.9 months (range 29–87). Preoperatively, our patients received a local steroid injection an average of 3.2 ± 2.3 times (range 1–8) and underwent aspiration an average of 4.1 ± 2.9 times (range 1–12). The radiographical examination was normal in all cases. In the endoscopic operations, two portals were made for only 24 (40%) patients and three portals for the other 36 (60%). All cases had endoscopic findings of synovial thickening and local inflammatory vascular patches throughout the cavity (both anterior and posterior wall) (Fig. 3). No loose bodies or bony fragments were found. None of the surgical cultures produced growth in either aerobic or anaerobic groups. Average operation time was 18 ± 5.6 minutes (range 10–25). After arthroscopic surgery, mild pain was present in 12 (20%), cases but could be controlled easily with oral analgesics. In our follow-up, 80% of the patients were completely pain-free. All patients returned to their pre-injury work and activities. There was no infection nor dehiscence of the surgical wound. No limitation of their activities was noted. No tenderness or hypoethesia of the surgical scar was noted. Knee range of motion (ROM) was full in every case. Only three patients needed repeated aspiration on the fifth to tenth days after operation due to vigorous ambulation and activities against our advice. No more recurrent swelling was found. In the final radiographic examination, no heterotopic bone formation or patella infera could be perceived. The sonographic examination showed no recurrence of accumulated fluid in any of the 60 cases. No infection, wound disruption, or any other iatrogenic problems developed. No compartment syndrome occurred.
Discussion
Prepatellar bursitis may be induced by many things, e.g. infections, tophi, rheumatoid arthritis, tuberculosis, trauma, minor injuries, or even in polio cases [1–9, 17]. Non-operative treatment is the mainstay for prepatellar bursitis [3]. This includes initial aspiration, applying compressive dressings, such as an Ace bandage, and administering nonsteroidal anti-inflammatory agents for ten to 14 days [18]. Due to the fact that repeated bursal aspiration is generally of little value [18], surgical excision is indicated for stubborn cases. The literature reveals that the most common complication of surgical treatment is wound problems [3, 11–15, 19, 20]. Poor healing of the incision, local tenderness, or decreased sensation of scar are not rare [2, 17]. Quayle and Robinson [11] described excision of only the posterior half of the prepatellar bursa, which is supposed to help in preventing damage to the overlying skin. Endoscopic examination of extra-articular cavities, clefts, and recesses is routinely performed today [3, 11–16, 19–23]. Witonski [16] suggested an arthroscopic resection of prepatellar bursitis of traumatic origin with good cosmetic results and economic advantages (reduced costs, time-saving and shortened hospital stays). Kerr et al. [22] reported that arthroscopic bursectomy could prevent wound problems [11–16]; however, their patients needed hospitalisation and general anaesthesia.
In our series, we treated patients on an outpatient basis. Only local anaesthesia was infiltrated into the bursal cavity and incision sites. Since endoscopic portals were very small, no suture was needed. If tension is present after operation, a simple suture can be applied without difficulty. The operation time is short (average time 18 minutes). In terms of reducing medical costs, the economic advantages are remarkable. Our results showed these endoscopic procedures caused no infection, no limitation of range of motion, no need for lifestyle change and no skin problems. The sonographic and radiographic examinations showed no recurrence of fluid accumulation. However, we did not include infectious bursitis and systemic diseases accompanied by bursitis in our series. Gomez-Rodriguez et al. [8] stated that 95% of septic bursitis could be treated well without open surgical drainage. Pien et al. [17] described 47 episodes of septic bursitis in a private community medical practice, and the majority of patients were able to be treated as outpatients with oral antibiotics. Both authors considered surgical procedures were unnecessary in septic bursitis. On the contrary, Knight et al. [10] suggested treatment of septic olecranon and prepatellar bursitis with percutaneous placement of a suction-irrigation system with subsequent antibiotic treatment for 19 days. The role of endoscopic surgery in treatment for septic prepatellar bursitis is still unclear, and further investigation is required.
Conclusion
For the treatment of stubborn post-traumatic prepatellar bursitis, outpatient endoscopic bursectomy under local anaesthesia is a time-saving and cost-effective procedure. Both cosmetic and functional results are satisfactory.
References
Bhat AK, Bhaskaranand K (2001) Massive prepatellar bursitis in post-polio residual paralysis: a case report. J Orthop Surg (Hong Kong) 9(1):71–73
Butcher JD, Salzman KL, Lillegard WA (1996) Lower extremity bursitis. Am Fam Physician 53(7):2317–2324
Crenshaw AH (1992) Campbells’s operative orthopaedics. Mosby, St Louis
Davis JM, Broughton SJ (1996) Prepatellar bursitis caused by Brucella abortus. Med J Aust 165(8):460
Dawn B, Williams JK, Walker SE (1997) Prepatellar bursitis: a unique presentation of tophaceous gout in an normouricemic patient. J Rheumatol 24(5):976–978
Donahue F, Turkel D, Mnaymneh W, Ghandur-Mnaymneh L (1996) Hemorragic prepatellar bursitis. Skeletal Radiol 25(3):298–301
Garcia-Porrua C, Gonzalez-Gay MA, Ibanez D, Garcia-Pais MJ (1999) The clinical spectrum of severe septic bursitis in northwestern Spain: a 10 year study. J Rheumatol 26(3):663–667
Gomez-Rodriguez N, Mendez-Garcia MJ, Ferreiro-Seoane JL, Ibanez-Ruan J, Penelas-Cortes Bellas Y (1997) Infectious bursitis: study of 40 cases in the prepatellar and olecranon regions. Enferm Infecc Microbiol Clín 15(5):237–242
Papadakis KA, Vartivarian SE, Vassilaki ME, Anaissie EJ (1996) Septic prepatellar bursitis caused by Stenotrophomonas (Xanthomonas) maltophilia. Clin Infect Dis 22(2):388–389
Knight JM, Thomas JC, Maurer RC (1986) Treatment of septic olecranon and prepatellar bursitis with percutaneous placement of a suction-irrigation system. A report of 12 cases. Clin Orthop 206:90–93
Quayle JB, Robinson MP (1978) A useful procedures in the treatment of chronic olecranon bursitis. Injury 9:249
Quayle JB, Robinson MP (1976) An operation for chronic prepatellar bursitis. J Bone Joint Surg (Br) 58:504
Nussbaumer P, Candrian C, Hollinger A (2001) Endoscopic bursa shaving in acute bursitis. Swiss Surg 7(3):121–125
Steinacker T, Verdonck A (1998) Endoscopic therapy of pre-patellar bursitis. Sportverletz Sportschaden 12(4):162–164
Stell IM (2000) Management of acute bursitis outcome study of a structured approach. J R Soc Med 92(10):516–521
Witonski D (1997) Arthroscopic resection of bursitis changes in the prepatellar bursae—preliminary report. Ortopedia Polska 62(1):63–65
Pien FD, Ching D, Kim E (1991) Septic bursitis: experience in a community practice. Orthopaedics 14(9):981–984
McAfee JH, Smith DL (1988) Olecranon and prepatellar bursitis—diagnosis and treatment. West J Med 149:607–610
Freys SM (1997) Olecranon and pre-patellar bursitis. Langenbecks Arch Chir Suppl Kongressbd 114:493–496
Ogilvie-Harris DJ, Gilbart M (2000) Endoscopic bursal resection: the olecranon bursa and prepatellar bursa. Arthroscopy 16(3):249–253
Kaalund S, Breddam M, Kristensen G (1998) Endoscopic resection of the septic prepatellar bursa. Arthroscopy 14(7):757–758
Kerr DR (1993) Prepatellar and olecranon arthroscopic bursectomy. Clin Sports Med 12(1):137–142
Klein W (1996) Endoscopy of the deep infrapatellar bursae. Arthroscopy 12(1):127–131
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Huang, YC., Yeh, WL. Endoscopic treatment of prepatellar bursitis. International Orthopaedics (SICOT) 35, 355–358 (2011). https://doi.org/10.1007/s00264-010-1033-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-1033-5