Abstract
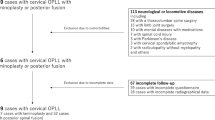
Between May 2002 and October 2006, 19 patients (17 men and 2 women; average age 57.2; range 47–71 years) received anterior corpectomy and fusion for severe ossification of the posterior longitudinal ligament (OPLL) in our department. Preoperative radiological evaluation showed the narrowing by the OPLL exceeded 50% in all cases, and OPLL extended from one to three vertebrae. We followed-up all patients for 12–36 months (mean 18 months). The Japanese Orthopaedic Association (JOA) score before surgery was 9.3 ± 1.8 (range 5–12) which significantly increased to 14.2 ± 1.3 (range 11–16) points at the last follow-up (P < 0.01). The improvement rate (IR) of neurological function ranged from 22.2–87.5%, with a mean of 63.2% ± 15.2%. The operation also provided a significant increase in the cervical lordosis and the cord flatting rate (P < 0.01). No severe neurological complication developed. We therefore concluded that anterior decompression and fusion was effective and safe in the treatment of the selected patients, although OPLL exceeded 50% diameter of the spinal canal.
Résumé
Entre mai 2002 et octobre 2006, 19 patients (17 hommes et 2 femmes) âgés en moyenne de 57,2 ans (47 à 71 ans) ont bénéficié d’une corporectomie antérieure avec arthrodèse pour une ossification sévère postérieure du ligament (OPLL). L’évaluation radiologique préopératoire a montré que l’importance de l’ossification était supérieure à 50% dans tous les cas et cette ossification (OPLL) s’étendait sur 1 à 3 niveaux vertébraux. Tous les patients ont été suivis en moyenne de 12 à 36 mois (18 mois en moyenne). Le score de la JOA a été de 1,8 en préopératoire (5 à 12) et a progressé jusqu’à 9,3 à 14,2 (11 à 16) au dernier suivi (P < 0,01). Le pourcentage d’amélioration neurologique a été de 22,2% à 87,5% avec une moyenne de 63,2%. L’intervention entraîne également une amélioration significative de la lordose cervicale et du taux d’applatissement de la moelle (P < 0,01). Aucune complication neurologique sévère n’a été observée. Nous pouvons conclure que la décompression antérieure associée à une greffe est une technique efficace et sûre du traitement des OPLL chez les patients sélectionnés dont le diamètre du canal rachidien doit être supérieur à 50%.


Similar content being viewed by others
References
Choi S, Lee SH, Lee JY et al (2005) Factors affecting prognosis of patients who underwent corpectomy and fusion for treatment of cervical ossification of the posterior longitudinal ligament: analysis of 47 patients. J Spinal Disord Tech 18:309–314
Chiang HS, Kondo S, Mizuno J et al (2004) Airway obstruction caused by cerebrospinal fluid leakage after anterior cervical spine surgery. A report of two cases. J Bone Joint Surg (Am) 86:370–372
Dorai Z, Morgan H, Coimbra C (2003) Titanium cage reconstruction after cervical corpectomy. J Neurosurg 24:3–7
Epstein N (2001) Anterior approaches to cervical spondylosis and ossification of the posterior longitudinal ligament: review of operative technique and assessment of 65 multilevel circumferential procedures. Surg Neurol 55:313–324
Epstein N (1993) The surgical management of ossification of the posterior longitudinal ligament in 51 patients. J Spinal Disord 6:432–454
Epstein N (2001) Identification of ossification of the posterior longitudinal ligament extending through the dura on preoperative computed tomographic examinations of the cervical spine. Spine 26:182–186
Hee HT, Majd ME, Holt RT et al (2003) Complications of multilevel cervical corpectomies and reconstruction with titanium cages and anterior plating. J Spinal Disord Tech 16:1–9
Hida K, Iwasaki Y, Koyanagi I et al (1997) Bone window computed tomography for detection of dural defect associated with cervical ossification posterior longitudinal ligament. Neurol Med Chir (Tokyo) 37:173–175
Iwasaki M, Okuda S, Miyauchi A et al (2007) Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: clinical results and limitations of laminoplasty. Spine 32:647–653
Iwasaki M, Okuda S, Miyauchi A et al (2007) Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: advantages of anterior decompression and fusion over laminoplasty. Spine 32:654–660
Kojima T, Waga S, Kudo Y et al (1989) Anterior cervical vertebrectomy and interbody fusion for multilevel spondylosis and ossification of the posterior longitudinal ligament. Neurosurgery 24:864–871
Kanayama M, Hashimoto T, Shigenobu K et al (2003) Pitfalls of anterior cervical fusion using titanium mesh and local autograft. J Spinal Disord Tech 16:513–518
Mizuno J, Nakagawa H (2006) Ossified posterior longitudinal ligament: management strategies and outcomes. Spine J 6:282–288
Masaki Y, Yamazaki M, Okawa A et al (2007) An analysis of factors causing poor surgical outcome in patients with cervical myelopathy due to ossification of the posterior longitudinal ligament: anterior decompression with spinal fusion versus laminoplasty. J Spinal Disord Tech 20:7–13
Matsuoka T, Yamaura I, Kurosa Y et al (2001) Long-term results of the anterior floating method for cervical myelopathy caused by ossification of the posterior longitudinal ligament. Spine 26:241–248
Narotam PK, Pauley SM, McGinn GJ (2003) Titanium mesh cages for cervical spine stabilization after corpectomy: a clinical and radiological study. J Neurosurg 24:172–180
Onari K, Akiyama N, Kondo S et al (2001) Long-term follow-up results of anterior interbody fusion applied for cervical myelopathy due to ossification of the posterior longitudinal ligament. Spine 26:488–493
Smith MD, Bolesta MJ, Leventhal M et al (1992) Postoperative cerebrospinal fluid fistula associated with erosion of the dura. Findings after anterior resection of ossification of the posterior longitudinal ligament in the cervical spine. J Bone Joint Surg 74:270–277
Tani T, Ushida T, Ishida K et al (2002) Relative safety of anterior microsurgical decompression versus laminoplasty for cervical myelopathy with a massive ossified posterior longitudinal ligament. Spine 27:2491–2498
Yamaura I, Kurosa Y, Matuoka T et al (1999) Anterior floating method for cervical myelopathy caused by ossification of the posterior longitudinal ligament. Clin Orthop Relat Res 359:27–34
Yonenobu K, Hosono N, Iwasaki M et al (1991) Neurologic complications of surgery for cervical compression myelopathy. Spine 16:1277–1282
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, Y., Chen, D., Wang, X. et al. Anterior corpectomy and fusion for severe ossification of posterior longitudinal ligament in the cervical spine. International Orthopaedics (SICOT) 33, 477–482 (2009). https://doi.org/10.1007/s00264-008-0542-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-008-0542-y