Abstract
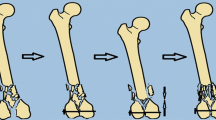
Despite recent developments in fracture treatment, cases of non-union after long bone fractures are still encountered. This work aims at evaluating the active management of delayed union after the bridge-plate fixation of multifragmentary diaphyseal fractures by a limited surgical interference. Nineteen patients were included. All had revision surgery for delayed union of multifragmentary diaphyseal fractures after bridge-plate fixation. The period between primary and revision surgery was 12–20 weeks. Increasing stability was performed by adding more screws in all cases. Interfragmentary compression was performed in 16 patients. Axial compression of the fracture was applied in two patients, while one patient had the plate exchanged for a longer one. Bone grafting was added in nine patients. Union was achieved in all patients 8–16 weeks after re-operation. This work is a message for timely surgical interference in delayed union after bridge-plate fixation by a limited surgical procedure, before complete failure of the fracture stabilisation or non-union.
Résumé
Malgré le développement des différents traitements, un certain nombre de pseudarthroses sont encore rencontré dans les fractures des os longs des membres. Le but de ce travail est d’évaluer la prise en charge de ces retards de consolidation après fixation par plaque de fractures diaphysaires multi fragmentaires. 19 patients ont été inclus pour ce travail. Ils ont bénéficié d’une reprise chirurgicale pour retard de consolidation après fixation par plaque. Le temps moyen entre l’intervention primaire et la révision a été de 12 à 20 semaines. Dans tous les cas il a été nécessaire d’augmenter la stabilité par l’addition de vis complémentaires. La compression inter fragmentaire a été réalisée chez 16 patients, une compression axiale chez 2 patients et un changement de plaque chez un patient. Une greffe a été nécessaire chez 9 patients. La consolidation a été totale chez tous les patients à 16 semaines après la réintervention. Ce travail a pour but de donner une information concernant l’algorithme chirurgical lorsqu’il existe un défaut de consolidation après ostéosynthèse par plaque.


Similar content being viewed by others
References
Babhulkar S, Pande K, Babhulkar S (2005) Nonunion of the diaphysis of long bones. Clin Orthop Relat Res 431:50–56
Baumgaertel F, Gotzen L (1994) The “biological” plate osteosynthesis in multi-fragment fractures of the para-articular femur. A prospective study. Unfallchirurg 97(2):78–84
Blatter G, Gasser B, Weber BG (1986) Die Wellenplatte. AO Bull 1:3–5
Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H (1999) Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma 13(6):401–406
Farouk O, Krettek C, Schandelmaier P, Said GZ, Tscherne H (1999) Anatomic basis of minimally invasive plate osteosynthesis in the femur. Tech Orthop 14(3):158–169
Gautier E, Ganz R (1994) The biological plate osteosynthesis. Zentralbl Chir 119(8):564–572
Müller ME, Allgöwer M, Schneider R, Willenegger H (1991) Manual of internal fixation: techniques recommended by the AO-ASIF group, 3rd edn. Springer, Berlin Heidelberg New York
Pai V, Coulter C, Pai V (2007) Minimally invasive plate fixation of the tibia. Int Orthop 31(4):491–496
Richter J, Schulze W, Muhr G (2000) Diaphyseal femur pseudarthroses—only a technical problem? Chirurg 71:1098–1106
Riemer B (2004) Plating diaphyseal fractures. Tech Orthop 18(4):360–367
Ring D, Barrick WT, Jupiter JB (1997) Recalcitrant nonunion. Clin Orthop Relat Res 340:181–189
Ring D, Kloen P, Kadzielski J, Helfet D, Jupiter JB (2004) Locking compression plates for osteoporotic nonunions of the diaphyseal humerus. Clin Orthop Relat Res 425:50–54
Smith WR, Morgan SJ (2002) Failure of internal fixation of the femoral shaft. Tech Orthop 17(4):448–457
Wenda K, Runkel M, Rudig L (1995) The “inserted” condylar plate. Unfallchirurgie 21(2):77–82
Wenda K, Runkel M, Degreif J, Rudig L (1997) Minimally invasive plate fixation in femoral shaft fractures. Injury 28(Suppl 1):A13–A19
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Said, G.Z., Farouk, O. & Said, H.G.Z. Delayed union of multifragmentary diaphyseal fractures after bridge-plate fixation. International Orthopaedics (SICOT) 33, 549–553 (2009). https://doi.org/10.1007/s00264-008-0528-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-008-0528-9