Abstract
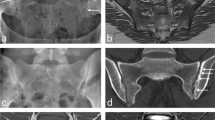
Infections of the sacroiliac joint are uncommon and the diagnosis is usually delayed. In a retrospective study, 17 patients who had been treated for tuberculosis sacroiliitis between 1994 and 2004 were reviewed. Two patients were excluded due to a short follow-up (less than 2 years). Low back pain and difficulty in walking were the most common presenting features. Two patients presented with a buttock abscess and spondylitis of the lumbar spine was noted in two patients. The Gaenslen’s and FABER (flexion, abduction and external rotation) tests were positive in all patients. Radiological changes included loss of cortical margins with erosion of the joints. An open biopsy and curettage was performed in all patients; histology revealed chronic infection and acid-fast bacilli were isolated in nine patients. Antituberculous (TB) medication was administered for 18 months and the follow-up ranged from 3 to 10 years (mean: 5 years). The sacroiliac joint fused spontaneously within 2 years. Although all patients had mild discomfort in the lower back following treatment they had no difficulty in walking. Sacroiliac joint infection must be included in the differential diagnosis of lower back pain and meticulous history and clinical evaluation of the joint are essential.
Résumé
L’infection des sacro-iliaques est rare et le diagnostic est souvent retardé. Dans une revue rétrospective 17 patients étaient traités pour une tuberculose sacro-iliaque entre 1994 et 2004. Deux patients étaient exclus à cause d’un suivi de moins de 2 ans. Des lombalgies et des difficultés de marche étaient les signes les plus fréquents. Deux patients présentaient un abcés de la fesse et deux autres une spondylite lombaire. Les test de Faber et de Gaenslen étaient positif chez tous les patients. Les signes radiologiques comportaient des érosions articulaires et des lyses corticales. Un curetage- biopsie était fait chez tous les patients et un bacille acido-résistant était isolé chez 9 patients. Un traitement anti-tuberculeux était administré pour 18 mois et le suivi était de 3 à 10 ans (en moyenne 5 ans). L’articulation sacro-iliaque se fusionnait dans les 2 ans. Bien que tous les patients gardaient un certain disconfort lombaire, ils n’avaient pas de difficulté de marche. L’infection sacro-iliaque doit faire partie des diagnostics différentiels des lombalgies et une évaluation méticuleuse de l’histoire et de la clinique est essentielle.



Similar content being viewed by others
References
Attarian DE (2001) Septic sacroiliitis: the overlooked diagnosis. J South Orthop Assoc 10(1):57–60
Babhulkar SS (2002) Clinical comment. Clin Orthop 398:2–3
Chen WS (1995) Chronic sciatica caused by tuberculous sacroiliitis-a case report. Spine 20(10):1194–1196
Coy JT, Wolf CR, Brower TD, Winter WG (1976) Pyogenic arthritis of the sacro-iliac joint. Long-term follow-up.J Bone Joint Surg Am 58(6):845–849
Davies PD, Humphries MJ, Byfield SP, Nunn AJ, Darbyshire JH, Citron KM, Fox W (1984) Bone and joint tuberculosis. A survey of notifications in England and Wales. J Bone Joint Surg Br 66(3):326–330
Dunn EJ, Bryan DM, Nugent JT, Robinson RA (1976) Pyogenic infections of the sacroiliac joint. Clin Orthop 118:113–118
Goldberg J, Kovarsky J (1983) Tuberculous sacroiliitis. South Med J 76(9):1175–1176
Gordan G, Kabins SA (1980) Pyogenic sacroiliitis. Am J Med 69:50–56
Hendrix RW, Lin PJ, Kane WJ (1982) Simplified aspiration or injection technique for the sacroiliac joint. J Bone Joint Surg Am 64(8):1249–1252
Isaacson AS, Whitehouse WM (1949) Spontaneous sacroiliac obliteration in patients with tuberculosis. J Bone Joint Surg Am 31(2):306–311
Kim NH, Lee HM, Suh JS (1994) Magnetic resonance imaging for the diagnosis of tuberculous spondylitis. Spine 19(21):2451–2455
Kim NH, Lee HM, Yoo JD, Suh JS (1999) Sacroiliac joint tuberculosis—classification and treatment. Clin Orthop 358:215–222
Laeslett M, Williams M (1994) The reliability of selected pain provocation tests for sacroiliac joint pathology. Spine 19(11):1243–1248
Martini M, Ouahes M (1988) Bone and joint tuberculosis: a review of 652 cases. Orthopedics 6:861–866
Miskew DB, Block RA, Witt PF (1979) Aspiration of infected sacroiliac joints. J Bone Joint Surg Am 61(7):1071–1072
Nicholson RA (1974) Twenty years of bone and joint tuberculosis in Bradford. A comparison of the disease in the indigenous and Asian populations. J Bone Joint Surg Br 56(4):760–765
Osman AA, Govender S (1995) Septic sacroiliitis. Clin Orthop 313:214–219
Pouchot J, Vinceneux P, Barge J, Boussougant Y, Grossin M, Pierre J, Carbon C, Kahn MF, Esdaile JM (1988) Tuberculosis of the sacroiliac joint: clinical features, outcome and evaluation of closed needle biopsy in 11 consecutive cases. Am J Med 84:622–628
Seddon HJ, Strange FG (1940) Sacroiliac tuberculosis. Br J Surg 28:193–221
Soholt ST (1951) Tuberculosis of the sacroiliac joint. J Bone Joint Surg Am 33(1):119–129
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ramlakan, R.J.S., Govender, S. Sacroiliac joint tuberculosis. International Orthopaedics (SICO 31, 121–124 (2007). https://doi.org/10.1007/s00264-006-0132-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-006-0132-9