Abstract
Background
In patients with advanced clear cell renal cell carcinoma, despite the undoubted benefits from immune checkpoint inhibitor (ICI)-based therapies over monotherapies of angiogenic/mTOR inhibitors in the intention-to-treat population, approximately a quarter of the patients can scarcely gain advantage from ICIs, prompting the search for predictive biomarkers for patient selection.
Methods
Clinical and multi-omic data of 2428 ccRCC patients were obtained from The Cancer Genome Atlas (TCGA, n = 537), JAVELIN Renal 101 (avelumab plus axitinib vs. sunitinib, n = 885), and CheckMate-009/010/025 (nivolumab vs. everolimus, n = 1006).
Results
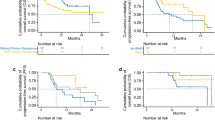
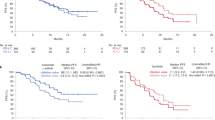
BAP1 mutations were associated with large progression-free survival (PFS) benefits from ICI-based immunotherapies over sunitinib/everolimus (pooled estimate of interaction HR = 0.71, 95% CI 0.51–0.99, P = 0.045). Using the top 20 BAP1 mutation-associated differentially expressed genes (DEGs) generated from the TCGA cohort, we developed the BAP1-score, negatively correlated with angiogenesis and positively correlated with multiple immune-related signatures concerning immune cell infiltration, antigen presentation, B/T cell receptor, interleukin, programmed death-1, and interferon. A high BAP1-score indicated remarkable PFS benefits from ICI-based immunotherapies over angiogenic/mTOR inhibitors (avelumab plus axitinib vs. sunitinib: HR = 0.55, 95% CI 0.43–0.70, P < 0.001; nivolumab vs. everolimus: HR = 0.72, 95% CI 0.52–1.00, P = 0.045), while these benefits were negligible in the low BAP1-score subgroup (HR = 1.16 and 1.02, respectively).
Conclusion
In advanced ccRCCs, the BAP1-score is a biologically and clinically significant predictor of immune microenvironment and the clinical benefits from ICI-based immunotherapies over angiogenic/mTOR inhibitors, demonstrating its potential utility in optimizing the personalized therapeutic strategies in patients with advanced ccRCC.






Similar content being viewed by others
Data availability
The authors declare that relevant data supporting the findings of this study are available within the paper and its Supplementary files. The references of all the included datasets are shown in Supplementary Table 1. Due to ethical and privacy concerns, we are unable to publish their full data in our study. Readers could contact the corresponding authors for the access of individual patient-level data for non-commercial purposes.
Abbreviations
- ccRCC:
-
Clear cell renal cell carcinoma
- CI:
-
Confidence interval
- CM-009/010/025:
-
Checkmate-009/010/025
- CTLA-4:
-
Cytotoxic T-cell lymphocyte-4
- DDR:
-
DNA damage repair
- DEG:
-
Differentially expressed gene
- GES:
-
Gene expression score
- HR:
-
Hazard ratio
- ICI:
-
Immune checkpoint inhibitor
- IHC:
-
Immunohistochemical
- PD-1:
-
Programmed cell death-1
- PD-L1:
-
Programmed death-ligand 1
- TCGA-KIRC:
-
The cancer genome atlas-kidney renal clear cell carcinoma
- TKI:
-
Tyrosine kinase inhibitor
- TMB:
-
Tumor mutational burden
- TPM:
-
Transcripts per million,
- RRR:
-
Ratio of relative risk
- ssGSEA:
-
Single sample gene set enrichment analysis
- STROBE:
-
Strengthening the reporting of observational studies in epidemiology
- VEGFR:
-
Vascular endothelial growth factor receptor
- WES:
-
Whole-exome sequencing
References
Choueiri TK, Powles T, Burotto M et al (2021) Nivolumab plus cabozantinib versus sunitinib for advanced renal-cell carcinoma. New Engl J Med 384:829–841. https://doi.org/10.1056/NEJMoa2026982
Motzer RJ, Rini BI, McDermott DF et al (2019) Nivolumab plus ipilimumab versus sunitinib in first-line treatment for advanced renal cell carcinoma: extended follow-up of efficacy and safety results from a randomised, controlled, phase 3 trial. Lancet Oncol 20:1370–1385. https://doi.org/10.1016/s1470-2045(19)30413-9
Motzer RJ, Tannir NM, McDermott DF et al (2018) Nivolumab plus Ipilimumab versus sunitinib in advanced renal-cell carcinoma. New Engl J Med 378:1277–1290. https://doi.org/10.1056/NEJMoa1712126
Powles T, Plimack ER, Soulières D et al (2020) Pembrolizumab plus axitinib versus sunitinib monotherapy as first-line treatment of advanced renal cell carcinoma (KEYNOTE-426): extended follow-up from a randomised, open-label, phase 3 trial. Lancet Oncol 21:1563–1573. https://doi.org/10.1016/s1470-2045(20)30436-8
Motzer R, Alekseev B, Rha SY et al (2021) Lenvatinib plus pembrolizumab or everolimus for advanced renal cell carcinoma. New Engl J Med 384:1289–1300. https://doi.org/10.1056/NEJMoa2035716
Rini BI, Plimack ER, Stus V et al (2019) Pembrolizumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. New Engl J Med. https://doi.org/10.1056/NEJMoa1816714
Rini BI, Powles T, Atkins MB et al (2019) Atezolizumab plus bevacizumab versus sunitinib in patients with previously untreated metastatic renal cell carcinoma (IMmotion151): a multicentre, open-label, phase 3, randomised controlled trial. Lancet 393:2404–2415. https://doi.org/10.1016/S0140-6736(19)30723-8
Motzer RJ, Penkov K, Haanen J et al (2019) Avelumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. New Engl J Med. https://doi.org/10.1056/NEJMoa1816047
Rini BI, Huseni M, Atkins MB et al (2018) Molecular correlates differentiate response to atezolizumab (atezo) + bevacizumab (bev) vs sunitinib (sun): Results from a phase III study (IMmotion151) in untreated metastatic renal cell carcinoma (mRCC). Ann Oncol 29:viii724–viii725. https://doi.org/10.1093/annonc/mdy424.037
Braun DA, Hou Y, Bakouny Z et al (2020) Interplay of somatic alterations and immune infiltration modulates response to PD-1 blockade in advanced clear cell renal cell carcinoma. Nat Med 26:909–918. https://doi.org/10.1038/s41591-020-0839-y
Ged Y, Chaim JL, DiNatale RG et al (2020) DNA damage repair pathway alterations in metastatic clear cell renal cell carcinoma and implications on systemic therapy. J Immunother Cancer. https://doi.org/10.1136/jitc-2019-000230
Labriola MK, Zhu J, Gupta RT et al (2020) Characterization of tumor mutation burden, PD-L1 and DNA repair genes to assess relationship to immune checkpoint inhibitors response in metastatic renal cell carcinoma. J Immunother Cancer. https://doi.org/10.1136/jitc-2019-000319
Motzer RJ, Choueiri TK, McDermott DF et al (2020) Biomarker analyses from the phase III CheckMate 214 trial of nivolumab plus ipilimumab (N+I) or sunitinib (S) in advanced renal cell carcinoma (aRCC). J Clin Oncol 38:5009. https://doi.org/10.1200/JCO.2020.38.15_suppl.5009
Motzer RJ, Robbins PB, Powles T et al (2020) Avelumab plus axitinib versus sunitinib in advanced renal cell carcinoma: biomarker analysis of the phase 3 JAVELIN Renal 101 trial. Nat Med 26:1733–1741. https://doi.org/10.1038/s41591-020-1044-8
Ross-Macdonald P, Walsh AM, Chasalow SD, Ammar R, Papillon-Cavanagh S, Szabo PM, Choueiri TK, Sznol M, Wind-Rotolo M (2021) Molecular correlates of response to nivolumab at baseline and on treatment in patients with RCC. J Immunother Cancer. https://doi.org/10.1136/jitc-2020-001506
Miao D, Margolis CA, Gao W et al (2018) Genomic correlates of response to immune checkpoint therapies in clear cell renal cell carcinoma. Science 359:801–806. https://doi.org/10.1126/science.aan5951
Dizman N, Lyou Y, Salgia N et al (2020) Correlates of clinical benefit from immunotherapy and targeted therapy in metastatic renal cell carcinoma: comprehensive genomic and transcriptomic analysis. J Immunother Cancer. https://doi.org/10.1136/jitc-2020-000953
Motzer RJ, Escudier B, McDermott DF et al (2015) Nivolumab versus everolimus in advanced renal-cell carcinoma. New Engl J Med 373:1803–1813. https://doi.org/10.1056/NEJMoa1510665
Tucker MD, Rini BI (2020) Predicting response to immunotherapy in metastatic renal cell carcinoma. Cancers (Basel). https://doi.org/10.3390/cancers12092662
Guida A, Sabbatini R, Gibellini L, De Biasi S, Cossarizza A, Porta C (2021) Finding predictive factors for immunotherapy in metastatic renal-cell carcinoma: what are we looking for? Cancer Treat Rev 94:102157. https://doi.org/10.1016/j.ctrv.2021.102157
Motzer RJ, Choueiri TK, McDermott DF et al (2022) Biomarker analysis from CheckMate 214: nivolumab plus ipilimumab versus sunitinib in renal cell carcinoma. J Immunother Cancer. https://doi.org/10.1136/jitc-2021-004316
Liu XD, Kong W, Peterson CB et al (2020) PBRM1 loss defines a nonimmunogenic tumor phenotype associated with checkpoint inhibitor resistance in renal carcinoma. Nat Commun 11:2135. https://doi.org/10.1038/s41467-020-15959-6
Motzer RJ, Banchereau R, Hamidi H et al (2020) Molecular subsets in renal cancer determine outcome to checkpoint and angiogenesis blockade. Cancer Cell 38:803–817. https://doi.org/10.1016/j.ccell.2020.10.011
McDermott DF, Huseni MA, Atkins MB et al (2018) Clinical activity and molecular correlates of response to atezolizumab alone or in combination with bevacizumab versus sunitinib in renal cell carcinoma. Nat Med 24:749–757. https://doi.org/10.1038/s41591-018-0053-3
Wang Z, Zhao J, Wang G et al (2018) Comutations in DNA damage response pathways serve as potential biomarkers for immune checkpoint blockade. Cancer Res 78:6486–6496. https://doi.org/10.1158/0008-5472.CAN-18-1814
Altman DG, Bland JM (2003) Interaction revisited: the difference between two estimates. BMJ 326:219
Ballman KV (2015) Biomarker: predictive or prognostic? J Clin Oncol 33:3968–3971. https://doi.org/10.1200/JCO.2015.63.3651
Newman AM, Liu CL, Green MR, Gentles AJ, Feng W, Xu Y, Hoang CD, Diehn M, Alizadeh AA (2015) Robust enumeration of cell subsets from tissue expression profiles. Nat Methods 12:453–457. https://doi.org/10.1038/nmeth.3337
Barbie DA, Tamayo P, Boehm JS et al (2009) Systematic RNA interference reveals that oncogenic KRAS-driven cancers require TBK1. Nature 462:108–112. https://doi.org/10.1038/nature08460
Subramanian A, Tamayo P, Mootha VK et al (2005) Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci USA 102:15545–15550. https://doi.org/10.1073/pnas.0506580102
Charoentong P, Finotello F, Angelova M, Mayer C, Efremova M, Rieder D, Hackl H, Trajanoski Z (2017) Pan-cancer immunogenomic analyses reveal genotype-immunophenotype relationships and predictors of response to checkpoint blockade. Cell Rep 18:248–262. https://doi.org/10.1016/j.celrep.2016.12.019
Cancer Genome Atlas Research N (2013) Comprehensive molecular characterization of clear cell renal cell carcinoma. Nature 499:43–49. https://doi.org/10.1038/nature12222
Thorsson V, Gibbs DL, Brown SD et al (2018) The immune landscape of cancer. Immunity 48:812–830. https://doi.org/10.1016/j.immuni.2018.03.023
Pena-Llopis S, Vega-Rubin-de-Celis S, Liao A et al (2012) BAP1 loss defines a new class of renal cell carcinoma. Nat Genet 44:751–759. https://doi.org/10.1038/ng.2323
Hakimi AA, Ostrovnaya I, Reva B et al (2013) Adverse outcomes in clear cell renal cell carcinoma with mutations of 3p21 epigenetic regulators BAP1 and SETD2: a report by MSKCC and the KIRC TCGA research network. Clin Cancer Res 19:3259–3267. https://doi.org/10.1158/1078-0432.CCR-12-3886
Wang Z, Wang X, Xu Y et al (2022) Mutations of PI3K-AKT-mTOR pathway as predictors for immune cell infiltration and immunotherapy efficacy in dMMR/MSI-H gastric adenocarcinoma. BMC Med. https://doi.org/10.1186/s12916-022-02327-y
Loi S, Michiels S, Baselga J et al (2013) PIK3CA genotype and a PIK3CA mutation-related gene signature and response to everolimus and letrozole in estrogen receptor positive breast cancer. PLoS ONE 8:e53292. https://doi.org/10.1371/journal.pone.0053292
Zhang K, Hong X, Song Z et al (2020) Identification of deleterious NOTCH mutation as novel predictor to efficacious immunotherapy in NSCLC. Clin Cancer Res. https://doi.org/10.1158/1078-0432.CCR-19-3976
Zhang F, Wang J, Xu Y, Cai S, Li T, Wang G, Li C, Zhao L, Hu Y (2022) Co-occurring genomic alterations and immunotherapy efficacy in NSCLC. NPJ Precis Oncol 6:4. https://doi.org/10.1038/s41698-021-00243-7
Bai H, Duan J, Li C et al (2020) EPHA mutation as a predictor of immunotherapeutic efficacy in lung adenocarcinoma. J Immunother Cancer. https://doi.org/10.1136/jitc-2020-001315
Wang T, Lu R, Kapur P et al (2018) An empirical approach leveraging tumorgrafts to dissect the tumor microenvironment in renal cell carcinoma identifies missing link to prognostic inflammatory factors. Cancer Discov 8:1142–1155. https://doi.org/10.1158/2159-8290.CD-17-1246
Bononi A, Giorgi C, Patergnani S et al (2017) BAP1 regulates IP3R3-mediated Ca(2+) flux to mitochondria suppressing cell transformation. Nature 546:549–553. https://doi.org/10.1038/nature22798
Lee HS, Seo HR, Lee SA, Choi S, Kang D, Kwon J (2019) BAP1 promotes stalled fork restart and cell survival via INO80 in response to replication stress. Biochem J 476:3053–3066. https://doi.org/10.1042/BCJ20190622
Lee HS, Lee SA, Hur SK, Seo JW, Kwon J (2014) Stabilization and targeting of INO80 to replication forks by BAP1 during normal DNA synthesis. Nat Commun 5:5128. https://doi.org/10.1038/ncomms6128
Nishikawa H, Wu W, Koike A, Kojima R, Gomi H, Fukuda M, Ohta T (2009) BRCA1-associated protein 1 interferes with BRCA1/BARD1 RING heterodimer activity. Cancer Res 69:111–119. https://doi.org/10.1158/0008-5472.CAN-08-3355
Daou S, Barbour H, Ahmed O et al (2018) Monoubiquitination of ASXLs controls the deubiquitinase activity of the tumor suppressor BAP1. Nat Commun 9:4385. https://doi.org/10.1038/s41467-018-06854-2
Daou S, Hammond-Martel I, Mashtalir N et al (2015) The BAP1/ASXL2 histone H2A deubiquitinase complex regulates cell proliferation and is disrupted in cancer. J Biol Chem 290:28643–28663. https://doi.org/10.1074/jbc.M115.661553
Ji Z, Mohammed H, Webber A, Ridsdale J, Han N, Carroll JS, Sharrocks AD (2014) The forkhead transcription factor FOXK2 acts as a chromatin targeting factor for the BAP1-containing histone deubiquitinase complex. Nucleic Acids Res 42:6232–6242. https://doi.org/10.1093/nar/gku274
Ruan HB, Han X, Li MD et al (2012) O-GlcNAc transferase/host cell factor C1 complex regulates gluconeogenesis by modulating PGC-1alpha stability. Cell Metab 16:226–237. https://doi.org/10.1016/j.cmet.2012.07.006
Baughman JM, Rose CM, Kolumam G et al (2016) NeuCode proteomics reveals bap1 regulation of metabolism. Cell Rep 16:583–595. https://doi.org/10.1016/j.celrep.2016.05.096
Bononi A, Yang H, Giorgi C et al (2017) Germline BAP1 mutations induce a Warburg effect. Cell Death Differ 24:1694–1704. https://doi.org/10.1038/cdd.2017.95
Zhang Y, Shi J, Liu X et al (2018) BAP1 links metabolic regulation of ferroptosis to tumour suppression. Nat Cell Biol 20:1181–1192. https://doi.org/10.1038/s41556-018-0178-0
Peng H, Yang F, Hu Q, Sun J, Peng C, Zhao Y, Huang C (2020) The ubiquitin-specific protease USP8 directly deubiquitinates SQSTM1/p62 to suppress its autophagic activity. Autophagy 16:698–708. https://doi.org/10.1080/15548627.2019.1635381
He M, Chaurushiya MS, Webster JD et al (2019) Intrinsic apoptosis shapes the tumor spectrum linked to inactivation of the deubiquitinase BAP1. Science 364:283–285. https://doi.org/10.1126/science.aav4902
Luo Z, Mu L, Zheng Y, Shen W, Li J, Xu L, Zhong B, Liu Y, Zhou Y (2020) NUMB enhances Notch signaling by repressing ubiquitination of NOTCH1 intracellular domain. J Mol Cell Biol 12:345–358. https://doi.org/10.1093/jmcb/mjz088
Misaghi S, Ottosen S, Izrael-Tomasevic A et al (2009) Association of C-terminal ubiquitin hydrolase BRCA1-associated protein 1 with cell cycle regulator host cell factor 1. Mol Cell Biol 29:2181–2192. https://doi.org/10.1128/MCB.01517-08
Kapur P, Peña-Llopis S, Christie A, Zhrebker L, Pavía-Jiménez A, Rathmell WK, Xie X-J, Brugarolas J (2013) Effects on survival of BAP1 and PBRM1 mutations in sporadic clear-cell renal-cell carcinoma: a retrospective analysis with independent validation. Lancet Oncol 14:159–167. https://doi.org/10.1016/s1470-2045(12)70584-3
Kapur P, Christie A, Raman JD et al (2014) BAP1 immunohistochemistry predicts outcomes in a multi-institutional cohort with clear cell renal cell carcinoma. J Urol 191:603–610. https://doi.org/10.1016/j.juro.2013.09.041
Miura Y, Inoshita N, Ikeda M et al (2017) Loss of BAP1 protein expression in the first metastatic site predicts prognosis in patients with clear cell renal cell carcinoma. Urol Oncol 35:386–391. https://doi.org/10.1016/j.urolonc.2017.02.003
Tennenbaum DM, Manley BJ, Zabor E et al (2017) Genomic alterations as predictors of survival among patients within a combined cohort with clear cell renal cell carcinoma undergoing cytoreductive nephrectomy. Urol Oncol 35(532):e7–e13. https://doi.org/10.1016/j.urolonc.2017.03.015
Oka S, Inoshita N, Miura Y et al (2018) The loss of BAP1 protein expression predicts poor prognosis in patients with nonmetastatic clear cell renal cell carcinoma with inferior vena cava tumor thrombosis. Urol Oncol 36(365):e9–e14. https://doi.org/10.1016/j.urolonc.2018.04.015
Ge YZ, Xu LW, Zhou CC et al (2017) A BAP1 mutation-specific MicroRNA signature predicts clinical outcomes in clear cell renal cell carcinoma patients with wild-type BAP1. J Cancer 8:2643–2652. https://doi.org/10.7150/jca.20234
Minardi D, Lucarini G, Milanese G, Di Primio R, Montironi R, Muzzonigro G (2016) Loss of nuclear BAP1 protein expression is a marker of poor prognosis in patients with clear cell renal cell carcinoma. Urol Oncol 34(338):e11–e18. https://doi.org/10.1016/j.urolonc.2016.03.006
da Costa WH, da Cunha IW, Fares AF et al (2018) Prognostic impact of concomitant loss of PBRM1 and BAP1 protein expression in early stages of clear cell renal cell carcinoma. Urol Oncol 36(243):e1–e8. https://doi.org/10.1016/j.urolonc.2018.01.002
Hsieh JJ, Chen D, Wang PI et al (2017) Genomic biomarkers of a randomized trial comparing first-line everolimus and sunitinib in patients with metastatic renal cell carcinoma. Eur Urol 71:405–414. https://doi.org/10.1016/j.eururo.2016.10.007
Voss MH, Reising A, Cheng Y et al (2018) Genomically annotated risk model for advanced renal-cell carcinoma: a retrospective cohort study. Lancet Oncol 19:1688–1698. https://doi.org/10.1016/s1470-2045(18)30648-x
Panou V, Gadiraju M, Wolin A et al (2018) Frequency of germline mutations in cancer susceptibility genes in malignant mesothelioma. J Clin Oncol 36:2863–2871. https://doi.org/10.1200/JCO.2018.78.5204
Harbour JW, Onken MD, Roberson ED et al (2010) Frequent mutation of BAP1 in metastasizing uveal melanomas. Science 330:1410–1413. https://doi.org/10.1126/science.1194472
Njauw CN, Kim I, Piris A et al (2012) Germline BAP1 inactivation is preferentially associated with metastatic ocular melanoma and cutaneous-ocular melanoma families. PLoS ONE 7:e35295. https://doi.org/10.1371/journal.pone.0035295
Popova T, Hebert L, Jacquemin V et al (2013) Germline BAP1 mutations predispose to renal cell carcinomas. Am J Hum Genet 92:974–980. https://doi.org/10.1016/j.ajhg.2013.04.012
Farley MN, Schmidt LS, Mester JL et al (2013) A novel germline mutation in BAP1 predisposes to familial clear-cell renal cell carcinoma. Mol Cancer Res 11:1061–1071. https://doi.org/10.1158/1541-7786.MCR-13-0111
Shrestha R, Nabavi N, Lin YY et al (2019) BAP1 haploinsufficiency predicts a distinct immunogenic class of malignant peritoneal mesothelioma. Genome Med 11:8. https://doi.org/10.1186/s13073-019-0620-3
Figueiredo CR, Kalirai H, Sacco JJ, Azevedo RA, Duckworth A, Slupsky JR, Coulson JM, Coupland SE (2020) Loss of BAP1 expression is associated with an immunosuppressive microenvironment in uveal melanoma, with implications for immunotherapy development. J Pathol 250:420–439. https://doi.org/10.1002/path.5384
Zhou Q, Qi Y, Wang Z et al (2020) CCR5 blockade inflames antitumor immunity in BAP1-mutant clear cell renal cell carcinoma. J Immunother Cancer. https://doi.org/10.1136/jitc-2019-000228
Wang L, Birch NW, Zhao Z et al (2021) Epigenetic targeted therapy of stabilized BAP1 in ASXL1 gain-of-function mutated leukemia. Nat Cancer 2:515–526. https://doi.org/10.1038/s43018-021-00199-4
Acknowledgements
We thank Dizai Shi (Stitch) for his emotional support and the researchers involved in the TCGA-KIRC dataset and the clinical trials (JAVELIN and CM-009/010/025) who shared patient-level data for public use.
Funding
This work was supported by National Natural Science Foundation of China (81770790 and 81972389 to Xu Zhang) and Hainan Province Science and Technology Special Fund (ZDYF2021SHFZ056 to Taoping Shi).
Author information
Authors and Affiliations
Contributions
KL, YH, YX, and TS conceptualized and designed this study. KL and YX developed the methodology and acquired the data. KL, YH, YX, and TS analyzed and interpreted the data. All authors contributed to the writing, review, and/or revision of the manuscript. GW, SC, and XZ provided administrative, technical, and/or material support. XZ and TS supervised this study. All authors approved the submitted version of manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest, except the employment of Yu Xu, Guoqiang Wang, and Shangli Cai in Burning Rock Biotech.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Ethical approval
Our study is following the principles of the Declaration of Helsinki and was approved by the Institution Review Board of Chinese PLA General Hospital (ChiCTR2000030405).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, K., Huang, Y., Xu, Y. et al. BAP1-related signature predicts benefits from immunotherapy over VEGFR/mTOR inhibitors in ccRCC: a retrospective analysis of JAVELIN Renal 101 and checkmate-009/010/025 trials. Cancer Immunol Immunother 72, 2557–2572 (2023). https://doi.org/10.1007/s00262-023-03424-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-023-03424-4