Abstract
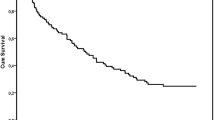
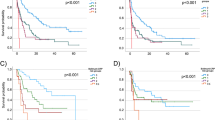
Despite recent advancements in immunotherapy, urothelial carcinoma patients with liver metastasis have a poor response to immune checkpoint inhibitors (ICIs) and short survival durations. Here, we investigated the clinical activity and molecular correlates of resistance to ICI in patients with metastatic urothelial carcinoma (mUC), focusing on liver metastasis. In this study, 755 patients with mUC who received pembrolizumab (JUOG cohort), 144 mUC patients who were treated with atezolizumab (IMvigor210 cohort), and 59 mUC patients who had metastatic samples available were enrolled. The presence of liver metastasis was associated with increased peripheral monocytes and a reduction in lymphocytes when compared with other metastatic sites, and a poor prognosis for ICI therapy. The peripheral monocyte-to-lymphocyte ratio was significantly correlated with the CD163+M2-like tumor-associated macrophage (TAM)/CD8+ tumor-infiltrative lymphocyte (TIL) ratio in the primary and metastatic UC lesions. Exploratory molecular analyses indicated that ICI-resistant status, such as decreased tumor mutation burden, low CD8+ TILs and immune checkpoint signatures, and increased M2-like TAM markers, in primary tumors was correlated with the presence of liver metastasis. In metastatic lesions, the CD163+M2-like TAM/CD8+TIL ratio and expression of cancer-associated fibroblasts induced by the TGFβ signaling pathway were higher in the liver versus the lung metastatic tumors. This study indicated that tumor-infiltrating lymphocyte and macrophage status in primary and metastatic lesions, which correlate with peripheral monocyte and lymphocyte status, may predict immunotherapy outcomes in UC patients with liver metastasis.





Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. Data of IMvigor210 can be found at http://research-pub.gene.com/IMvigor210CoreBiologies/.
Abbreviations
- CAF:
-
Cancer associated fibroblast
- c-index:
-
Concordance index
- CI:
-
Confidence interval
- CR:
-
Complete response
- ECOG-PS:
-
Eastern cooperative oncology group performance status
- FFPE:
-
Formalin-fixed, paraffin-embedded
- F-TBRS:
-
A pan-fibroblast TGFβ response signature
- HR:
-
Hazard ratio
- IC:
-
Tumor-infiltrating immune cell
- ICI:
-
Immune checkpoint inhibitor
- IHC:
-
Immunohistochemistry
- IRB:
-
Institutional review board
- JUOG:
-
The Japan urological oncology group
- LN:
-
Lymphonode
- MLR:
-
Monocyte-to-lymphocyte ratio
- Mo:
-
Months
- myCAF:
-
Myofibroblastic CAF
- NLR:
-
Neutrophil-to-lymphocyte ratio
- OR:
-
Odds ratio
- ORR:
-
Objective response rate
- OS:
-
Overall survival
- PD:
-
Progression disease
- PD-1:
-
Programmed cell death-1
- PD-L1:
-
Programmed cell death-ligand 1
- PR:
-
Partial response
- RECIST:
-
Response evaluation criteria in solid tumors
- SD:
-
Stable disease
- TAM:
-
Tumor associated macrophage
- TCGA:
-
The cancer genome atlas
- T eff :
-
T-effector
- TIL:
-
Tumor-infiltrating lymphocyte
- TMB:
-
Tumor mutation burden
- TME:
-
Tumor microenviroment
- TNB:
-
Tumor neoantigen burden
- UC:
-
Urothelial carcinoma
References
Balar AV, Galsky MD, Rosenberg JE, Powles T, Petrylak DP, Bellmunt J et al (2017) Atezolizumab as first-line treatment in cisplatin-ineligible patients with locally advanced and metastatic urothelial carcinoma: a single-arm, multicentre, phase 2 trial. Lancet 389:67–76
Witjes JA, Bruins HM, Cathomas R, Compérat EM, Cowan NC, Gakis G et al (2021) European association of urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2020 guidelines. Eur Urol 79:82–104
Clinton TN (2021) Defining resistance to immune checkpoint inhibitors in urothelial carcinoma: insights from PURE-01. Eur Urol 80:323–324
Khaki AR, Li A, Diamantopoulos LN, Miller NJ, Carril-Ajuria L, Castellano D et al (2021) A new prognostic model in patients with advanced urothelial carcinoma treated with first-line immune checkpoint inhibitors. Eur Urol Oncol 4:464–472
Sonpavde G, Manitz J, Gao C, Tayama D, Kaiser C, Hennessy D et al (2020) Five-factor prognostic model for survival of post-platinum patients with metastatic urothelial carcinoma receiving PD-L1 inhibitors. J Urol 204:1173–1179
Kobayashi T, Ito K, Kojima T, Kato M, Kanda S, Hatakeyama S et al (2021) Risk stratification for the prognosis of patients with chemoresistant urothelial cancer treated with pembrolizumab. Cancer Sci 112:760–773
Milette S, Sicklick JK, Lowy AM, Brodt P (2017) Molecular pathways: targeting the microenvironment of liver metastases. Clin Cancer Res 23:6390–6399
Curtis LT, Sebens S, Frieboes HB (2021) Modeling of tumor response to macrophage and T lymphocyte interactions in the liver metastatic microenvironment. Cancer Immunol Immunother 70:1475–1488
Lee JC, Mehdizadeh S, Smith J, Young A, Mufazalov IA, Mowery CT et al (2020) Regulatory T cell control of systemic immunity and immunotherapy response in liver metastasis. Sci Immunol 5:eaba0759
Doherty DG (2016) Immunity, tolerance and autoimmunity in the liver: a comprehensive review. J Autoimmun 66:60–75
Li F, Tian Z (2013) The liver works as a school to educate regulatory immune cells. Cell Mol Immunol 10:292–302
Loo K, Tsai KK, Mahuron K, Liu J, Pauli ML, Sandoval PM, et al. (2017) Partially exhausted tumor-infiltrating lymphocytes predict response to combination immunotherapy. JCI Insight 2
Yu J, Green MD, Li S, Sun Y, Journey SN, Choi JE et al (2021) Liver metastasis restrains immunotherapy efficacy via macrophage-mediated T cell elimination. Nat Med 27:152–164
Mariathasan S, Turley SJ, Nickles D, Castiglioni A, Yuen K, Wang Y et al (2018) TGFβ attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature 554:544–548
Choi YH, Lee JW, Lee SH, Choi JH, Kang J, Lee BS et al (2019) A high monocyte-to-lymphocyte ratio predicts poor prognosis in patients with advanced gallbladder cancer receiving chemotherapy. Cancer Epidemiol Biomark Prev 28:1045–1051
Bolen CR, McCord R, Huet S, Frampton GM, Bourgon R, Jardin F et al (2017) Mutation load and an effector T-cell gene signature may distinguish immunologically distinct and clinically relevant lymphoma subsets. Blood Adv 1:1884–1890
Subramanian A, Tamayo P, Mootha VK, Mukherjee S, Ebert BL, Gillette MA et al (2005) Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci USA 102:15545–15550
Tremble LF, McCabe M, Walker SP, McCarthy S, Tynan RF, Beecher S et al (2020) Differential association of CD68. Br J Cancer 123:1553–1561
Chen J, Yang P, Xiao Y, Zhang Y, Liu J, Xie D et al (2017) Overexpression of α-sma-positive fibroblasts (CAFs) in nasopharyngeal carcinoma predicts poor prognosis. J Cancer 8:3897–3902
Bangalore S, Guo Y, Samadashvili Z, Blecker S, Xu J, Hannan EL (2015) Everolimus-eluting stents or bypass surgery for multivessel coronary disease. N Engl J Med 372:1213–1222
Bellmunt J, Choueiri TK, Fougeray R, Schutz FA, Salhi Y, Winquist E et al (2010) Prognostic factors in patients with advanced transitional cell carcinoma of the urothelial tract experiencing treatment failure with platinum-containing regimens. J Clin Oncol 28:1850–1855
Bajorin DF, Dodd PM, Mazumdar M, Fazzari M, McCaffrey JA, Scher HI et al (1999) Long-term survival in metastatic transitional-cell carcinoma and prognostic factors predicting outcome of therapy. J Clin Oncol 17:3173–3181
Batlle E, Massagué J (2019) Transforming growth factor-β signaling in immunity and cancer. Immunity 50:924–940
Ganesh K, Massagué J (2018) TGF-β inhibition and immunotherapy: checkmate. Immunity 48:626–628
Sahai E, Astsaturov I, Cukierman E, DeNardo DG, Egeblad M, Evans RM et al (2020) A framework for advancing our understanding of cancer-associated fibroblasts. Nat Rev Cancer 20:174–186
Nenclares P, Gunn L, Soliman H, Bover M, Trinh A, Leslie I, et al. (2021) On-treatment immune prognostic score for patients with relapsed and/or metastatic head and neck squamous cell carcinoma treated with immunotherapy. J Immunother Cancer 9
Sanford DE, Belt BA, Panni RZ, Mayer A, Deshpande AD, Carpenter D et al (2013) Inflammatory monocyte mobilization decreases patient survival in pancreatic cancer: a role for targeting the CCL2/CCR2 axis. Clin Cancer Res 19:3404–3415
Grossman JG, Nywening TM, Belt BA, Panni RZ, Krasnick BA, DeNardo DG et al (2018) Recruitment of CCR2. Oncoimmunology 7:e1470729
Bhattacharjee S, Hamberger F, Ravichandra A, Miller M, Nair A, Affo S, et al. (2021) Tumor restriction by type I collagen opposes tumor-promoting effects of cancer-associated fibroblasts. J Clin Invest 131
Li S, Sun S, Xiang H, Yang J, Peng M, Gao Q (2020) Liver metastases and the efficacy of the PD-1 or PD-L1 inhibitors in cancer: a meta-analysis of randomized controlled trials. Oncoimmunology 9:1746113
Acknowledgements
We greatly thank Mr. Ryousuke Yamaka for his technical assistance in tissue sampling.
Funding
This study has been supported by the Japan Society for the Promotion of Science KAKENHI fund (# 20K07601 to TY, # 25713055, and # 19H03790 to TK).
Author information
Authors and Affiliations
Consortia
Contributions
TY and TK contributed to study concept and design. TY, TK, and CO contributed to acquisition, analysis, or interpretation of data. TY drafied the manuscript. All authors critically revised the manuscript for important intellectual content. TY contributed to statistical analysis. TY, TK, HK, and HN supervised the study.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for publication
Not required.
Ethical approval
Institutional review boards of the Kansai Medical University, Kyoto University Graduate School of Medicine and local each participating institution as the Japan Urological Oncology Group framework approved this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
Study institutes: Osaka City University, Akita University, Hirosaki University, National Cancer Center Hospital, Hamamatsu University School of Medicine, Yamagata University Faculty of Medicine, Kyoto University, University of Tsukuba, Nara Medical University, Shizuoka General Hospital, University of the Ryukyus, Iwate Medical University, Oita University, Hiroshima University, Shimane University, Kansai Medical University, Osaka University, Kagawa University, University of Yamanashi, Japanese Red Cross Wakayama Medical Center, Kyoto Prefectural University of Medicine, Kobe City Nishi-Kobe Medical Center, Japanese Red Cross Osaka Hospital, Nagoya University, Harasanshin Hospital, Hokkaido University, Japanese Red Cross Otsu Hospital, Kagoshima University, Kyushu University, Shikoku Cancer Center, Tenri Hospital, Hakodate Goryoukaku Hospital, Kitasato University, Kyoto Katsura Hospital, National Hospital Organization Kyoto Medical Center, Kumamoto University, National Hospital Organization Himeji Medical Center, Tazuke Kofukai Medical Research Institute, Kitano Hospital, Toyooka Hospital, Hokkaido Cancer Center, University of Miyazaki, Hitachi General Hospital, The Jikei University Kashiwa Hospital, Shimada Municipal Hospital, Mie University, Yamaguchi University, Ibaraki Prefectural Central Hospital, Kyoto City Hospital, Kochi School of Medicine, Ijinkai Takeda General Hospital, University of Toyama, Otsu City Hospital, Sapporo Medical University, Kansai Electric Power Hospital, Kurume University, Hyogo College of Medicine, Hirakata Kohsai Hospital, Rakuwakai Otowa Memorial Hospital, Jikei University.
Rights and permissions
About this article
Cite this article
Yoshida, T., Ohe, C., Ito, K. et al. Clinical and molecular correlates of response to immune checkpoint blockade in urothelial carcinoma with liver metastasis. Cancer Immunol Immunother 71, 2815–2828 (2022). https://doi.org/10.1007/s00262-022-03204-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-022-03204-6