Abstract
Background
Latency-associated peptide (LAP) was identified as crucial immune regulator in tumor microenvironment (TME) in recent researches. In this study, we aimed to estimate the predictive value of LAP expression for clinical survival and therapeutic response in muscle-invasive bladder cancer (MIBC).
Methods
Our study encompassed 140 MIBC patients from Zhongshan Hospital (ZSHS cohort), 401 patients from The Cancer Genome Atlas (TCGA cohort) and 195 patients received PDL1 blockade from IMvigor210 trial. Survival analyses were conducted through Kaplan–Meier curve and Cox regression model. LAP expression and its association with immune contexture were evaluated in ZSHS and TCGA cohort.
Results
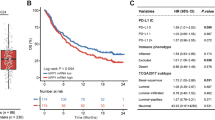
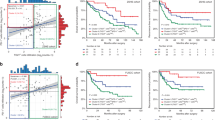
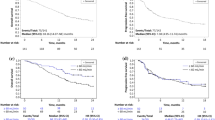
We found that high intratumoral LAP+ cells infiltration anticipated inferior survival and adjuvant chemotherapy (ACT) response, and was closely related to an immunoevasive contexture with increased M2 macrophages, neutrophils and conspicuously a cluster of highly exhausted CD8+ T cells. The combinational analysis of LAP+ cells and CD8+ T cells infiltration stratified patients into distinct risk groups with implications for therapeutic sensitivity to PDL1 blockade and refinement of molecular classification in MIBC.
Conclusions
LAP expression was correlated with patients’ inferior prognosis, ACT-tolerance and an immunoevasive TME with exhausted CD8+ T cell infiltration, suggesting that LAP could serve as a promising therapeutic target in MIBC. Simultaneously, our novel TME classification based on LAP+ cells and CD8+ T cells infiltration and its potential in appraising PDL1 blockade application for MIBC patients deserved further validation.




Similar content being viewed by others
Data availability
All data generated that are relevant to the results presented in this article are included in this article. Other data that were not relevant for the results presented here are available from the corresponding author Dr. Xu upon reasonable request.
Abbreviations
- ACT :
-
Adjuvant chemotherapy
- AJCC :
-
American Joint Committee on Cancer
- CI :
-
Confidence interval
- FPKM :
-
Fragments per kilobase of exon model per million mapped fragments
- GSEA :
-
Gene sets enrichment analysis
- HR :
-
Hazard ratios
- ICIs :
-
Immune checkpoint inhibitors
- IHC :
-
Immunohistochemistry
- LAP :
-
Latency-associated peptide
- LVI :
-
Lymphatic vessel invasion
- MIBC :
-
Muscle-invasive bladder cancer
- NMIBC :
-
Non-muscle-invasive bladder cancer
- OS :
-
Overall survival
- RFS :
-
Recurrence-free survival
- TCGA :
-
The Cancer Genome Atlas
- TGF-β :
-
Transforming growth factor-β
- TMA :
-
Tissue microarray
- TME :
-
Tumor microenvironment
- TNM :
-
Tumor–node–metastasis
- ZSHS :
-
Zhongshan Hospital
References
Hurst C, Rosenberg J, Knowles M (2018) SnapShot: bladder cancer. Cancer Cell 34(2):350-350.e1. https://doi.org/10.1016/j.ccell.2018.07.013
Robertson AG, Kim J, Al-Ahmadie H et al (2017) Comprehensive molecular characterization of muscle-invasive bladder cancer. Cell 171(3):540–56.e25. https://doi.org/10.1016/j.cell.2017.09.007
Knowles MA, Hurst CD (2015) Molecular biology of bladder cancer: new insights into pathogenesis and clinical diversity. Nat Rev Cancer 15(1):25–41. https://doi.org/10.1038/nrc3817
Witjes JA, Bruins HM, Cathomas R et al (2021) European association of urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2020 guidelines. Eur Urol 79(1):82–104. https://doi.org/10.1016/j.eururo.2020.03.055
von der Maase H, Hansen SW, Roberts JT et al (2000) Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicenter, phase III study. J Clin Oncol 18(17):3068–3077. https://doi.org/10.1200/jco.2000.18.17.3068
Vasekar M, Degraff D, Joshi M (2016) Immunotherapy in bladder cancer. Curr Mol Pharmacol 9(3):242–251. https://doi.org/10.2174/1874467208666150716120945
Patel VG, Oh WK, Galsky MD (2020) Treatment of muscle-invasive and advanced bladder cancer in 2020. CA Cancer J Clin 70(5):404–423. https://doi.org/10.3322/caac.21631
Crispen PL, Kusmartsev S (2020) Mechanisms of immune evasion in bladder cancer. Cancer Immunol Immunother 69(1):3–14. https://doi.org/10.1007/s00262-019-02443-4
Flavell RA, Sanjabi S, Wrzesinski SH, Licona-Limón P (2010) The polarization of immune cells in the tumour environment by TGFbeta. Nat Rev Immunol 10(8):554–567. https://doi.org/10.1038/nri2808
Liu H, Zhu Y, Zhu H et al (2019) Role of transforming growth factor β1 in the inhibition of gastric cancer cell proliferation by melatonin in vitro and in vivo. Oncol Rep 42(2):753–762. https://doi.org/10.3892/or.2019.7190
Khalil N (1999) TGF-beta: from latent to active. Microbes Infect 1(15):1255–1263. https://doi.org/10.1016/s1286-4579(99)00259-2
Batlle E, Massague J (2019) Transforming growth factor-beta signaling in immunity and cancer. Immunity 50(4):924–940. https://doi.org/10.1016/j.immuni.2019.03.024
Shi M, Zhu J, Wang R et al (2011) Latent TGF-β structure and activation. Nature 474(7351):343–349. https://doi.org/10.1038/nature10152
Gabriely G, da Cunha AP, Rezende RM et al (2017) Targeting latency-associated peptide promotes antitumor immunity. Sci Immunol. https://doi.org/10.1126/sciimmunol.aaj1738
Flemming A (2017) Tumour Immunology: LAP targeting reduces tolerogenic cells in cancer. Nat Rev Immunol 17(7):402–403. https://doi.org/10.1038/nri.2017.65
Mariathasan S, Turley SJ, Nickles D et al (2018) TGFβ attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature 554(7693):544–548. https://doi.org/10.1038/nature25501
Chen B, Khodadoust MS, Liu CL, Newman AM, Alizadeh AA (2018) Profiling tumor infiltrating immune cells with CIBERSORT. Methods Mol Biol 1711:243–259. https://doi.org/10.1007/978-1-4939-7493-1_12
Fridman WH, Zitvogel L, Sautès-Fridman C, Kroemer G (2017) The immune contexture in cancer prognosis and treatment. Nat Rev Clin Oncol 14(12):717–734. https://doi.org/10.1038/nrclinonc.2017.101
Schneider AK, Chevalier MF, Derré L (2019) The multifaceted immune regulation of bladder cancer. Nat Rev Urol 16(10):613–630. https://doi.org/10.1038/s41585-019-0226-y
Baitsch L, Baumgaertner P, Devêvre E et al (2011) Exhaustion of tumor-specific CD8+ T cells in metastases from melanoma patients. J Clin Invest 121(6):2350–2360. https://doi.org/10.1172/jci46102
Liu Z, Zhou Q, Wang Z et al (2020) Intratumoral TIGIT(+) CD8(+) T-cell infiltration determines poor prognosis and immune evasion in patients with muscle-invasive bladder cancer. J Immunother Cancer. https://doi.org/10.1136/jitc-2020-000978
Angell H, Galon J (2013) From the immune contexture to the Immunoscore: the role of prognostic and predictive immune markers in cancer. Curr Opin Immunol 25(2):261–267. https://doi.org/10.1016/j.coi.2013.03.004
Bruni D, Angell HK, Galon J (2020) The immune contexture and Immunoscore in cancer prognosis and therapeutic efficacy. Nat Rev Cancer 20(11):662–680. https://doi.org/10.1038/s41568-020-0285-7
Fakih M, Ouyang C, Wang C et al (2019) Immune overdrive signature in colorectal tumor subset predicts poor clinical outcome. J Clin Invest 129(10):4464–4476. https://doi.org/10.1172/jci127046
Huntsman DG, Ladanyi M (2018) The molecular pathology of cancer: from pan-genomics to post-genomics. J Pathol 244(5):509–511. https://doi.org/10.1002/path.5057
Kamoun A, de Reyniès A, Allory Y et al (2020) A consensus molecular classification of muscle-invasive bladder cancer. Eur Urol 77(4):420–433. https://doi.org/10.1016/j.eururo.2019.09.006
Tang H, Qiao J, Fu YX (2016) Immunotherapy and tumor microenvironment. Cancer Lett 370(1):85–90. https://doi.org/10.1016/j.canlet.2015.10.009
Necchi A, Pond GR, Moschini M et al (2019) Development of a prediction tool for exclusive locoregional recurrence after radical cystectomy in patients with muscle-invasive bladder cancer. Clin Genitourin Cancer 17(1):7-14.e3. https://doi.org/10.1016/j.clgc.2018.09.008
Seiler R, Ashab HAD, Erho N et al (2017) Impact of molecular subtypes in muscle-invasive bladder cancer on predicting response and survival after neoadjuvant chemotherapy. Eur Urol 72(4):544–554. https://doi.org/10.1016/j.eururo.2017.03.030
Tan TZ, Rouanne M, Tan KT, Huang RY, Thiery JP (2019) Molecular subtypes of urothelial bladder cancer: results from a meta-cohort analysis of 2411 tumors. Eur Urol 75(3):423–432. https://doi.org/10.1016/j.eururo.2018.08.027
Xie F, Ling L, van Dam H, Zhou F, Zhang L (2018) TGF-β signaling in cancer metastasis. Acta Biochim Biophys Sin (Shanghai) 50(1):121–132. https://doi.org/10.1093/abbs/gmx123
Batlle E, Massagué J (2019) Transforming growth factor-β signaling in immunity and cancer. Immunity 50(4):924–940. https://doi.org/10.1016/j.immuni.2019.03.024
Ruffell B, Chang-Strachan D, Chan V et al (2014) Macrophage IL-10 blocks CD8+ T cell-dependent responses to chemotherapy by suppressing IL-12 expression in intratumoral dendritic cells. Cancer Cell 26(5):623–637. https://doi.org/10.1016/j.ccell.2014.09.006
Tumeh PC, Harview CL, Yearley JH et al (2014) PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature 515(7528):568–571. https://doi.org/10.1038/nature13954
Wherry EJ, Kurachi M (2015) Molecular and cellular insights into T cell exhaustion. Nat Rev Immunol 15(8):486–499. https://doi.org/10.1038/nri3862
Dimeloe S, Gubser P, Loeliger J et al (2019) Tumor-derived TGF-β inhibits mitochondrial respiration to suppress IFN-γ production by human CD4(+) T cells. Sci Signal. https://doi.org/10.1126/scisignal.aav3334
Li S, Liu M, Do MH et al (2020) Cancer immunotherapy via targeted TGF-β signalling blockade in T(H) cells. Nature 587(7832):121–125. https://doi.org/10.1038/s41586-020-2850-3
Liu M, Kuo F, Capistrano KJ et al (2020) TGF-β suppresses type 2 immunity to cancer. Nature 587(7832):115–120. https://doi.org/10.1038/s41586-020-2836-1
Acknowledgements
We thank Dr. Lingli Chen (Department of Pathology, Zhongshan Hospital, Fudan University, Shanghai, China) and Dr. Yunyi Kong (Department of Pathology, Fudan University Shanghai Cancer Center, Shanghai, China) for their excellent pathological technology help.
Funding
This study was funded by grants from National Natural Science Foundation of China (31770851, 81872082, 81902556, 82002670), Shanghai Municipal Natural Science Foundation (19ZR1431800), Shanghai Sailing Program (18YF1404500, 19YF1427200, 21YF1407000), Shanghai Municipal Commission of Health and Family Planning Program (20174Y0042, 201840168, 20184Y0151) and Fudan University Shanghai Cancer Center for Outstanding Youth Scholars Foundation (YJYQ201802). All these study sponsors have no roles in the study design, in the collection, analysis and interpretation of data.
Author information
Authors and Affiliations
Contributions
R. Y, H. Z, Z. L and K. J were involved in acquisition of data, analysis and interpretation of data, statistical analysis and drafting of the manuscript; C. L, S. Y, Y. Y, R. Y, H. Z, Y. W, L. L and Y. Z helped in technical and material support; Y. C, J. X, L. X and Z. W contributed to study concept and design, analysis and interpretation of data, drafting of the manuscript, obtained funding and study supervision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest.
Consent for publication
All authors provide their consent for publication.
Ethics approval and consent to participate
The study followed the Declaration of Helsinki and was approved by the Clinical Research Ethics Committee of Zhongshan Hospital. Signed informed consent was obtained from each patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
262_2021_2987_MOESM1_ESM.tif
Supplementary Figure 1. Patient cohort and IHC staining of LAP expression in MIBC. (A) Enrollment process of patients in ZSHS cohort and TCGA cohort. (B) Representative immunohistochemistry images of LAP+ cells. FFPE, Formalin-Fixed and Paraffin-Embedded (TIF 1220 kb)
262_2021_2987_MOESM2_ESM.tif
Supplementary Figure 2. Association of tumor immune microenvironment with LAP expression. (A) IHC evaluation of various immune cells between LAP+ cells low/high subgroups in ZSHS cohort. Mann–Whitney test was adopted (TIF 457 kb)
262_2021_2987_MOESM3_ESM.tif
Supplementary Figure 3. The survival benefit of CD8+ T cells infiltration is impaired by LAP expression. (A-B) Kaplan–Meier curve of OS according to LAP/TGFB1 expression and CD8+ T cells infiltration in TCGA cohort (A) and ZSHS cohort (B) (TIF 390 kb)
262_2021_2987_MOESM4_ESM.tif
Supplementary Figure 4. CD8+ T cells infiltration fails to predict prognosis in patients with high LAP/TGFB1 subgroup. (A-D) Kaplan–Meier curve of OS (A, C) and RFS (B, D) according to CD8+ cells infiltration in all patients (left), patients with low LAP/TGFB1 expression (middle) and patients with high LAP/TGFB1 expression (right) in ZSHS cohort (A, B) and TCGA cohort (C, D) (TIF 1642 kb)
262_2021_2987_MOESM5_ESM.tif
Supplementary Figure 5. Association of TME classification based on LAP expression and CD8+ T cells infiltration with clinical outcomes and molecular features in MIBC. (A-B) Kaplan-Meier curves of RFS between three clusters in ZSHS cohort (A) and TCGA cohort (B) by log-rank test. (C) Comparison of consensus molecular systems with three clusters in TCGA cohort by Chi-square test. (D) Kaplan–Meier curve of RFS by log-rank test in basal/squamous subtype between cluster II and cluster III patients in TCGA cohort (TIF 524 kb)
Rights and permissions
About this article
Cite this article
Ye, R., Zeng, H., Liu, Z. et al. Latency-associated peptide identifies therapeutically resistant muscle-invasive bladder cancer with poor prognosis. Cancer Immunol Immunother 71, 301–310 (2022). https://doi.org/10.1007/s00262-021-02987-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-021-02987-4