Abstract
Background
Stage IV melanoma has high mortality, largely unaffected by traditional therapies. Immunotherapy including cytokine therapies and checkpoint inhibitors improves outcomes, but has significant toxicities. In this phase I/IIa trial, we investigated safety and efficacy of a dendritoma vaccine, an active, specific immunotherapy, in stage IV melanoma patients.
Methods
Autologous tumor lysate and dendritic cells were fused creating dendritoma vaccines for each patient. Phase I patients were vaccinated every 3 months with IL-2 given for 5 days after initial inoculation. Phase IIa patients were vaccinated every 6 weeks with IL-2 given on days 1, 3 and 5 after initial inoculation. Toxicity and clinical outcomes were assessed.
Results
Twenty-five patients were enrolled and inoculated. All dendritoma and IL-2 toxicities were <grade 3. Median overall survival (OS) was 16.1 months with projected 5-year survival = 29 %. Significant OS improvement for patients receiving ≥3 versus <3 inoculations (43.1 vs. 16.7 %, p = 0.02) was observed. Patients with no evidence of disease (NED) showed improved OS (80 vs. 14 %, p = 0.005). No clinicopathologic differences were present between phase I (n = 10) and IIa (n = 15) patients; phase IIa patients received more frequent dosing and higher mean number of inoculations. Phase IIa median OS was significantly higher (23.8 vs. 8.7 months, p = 0.004).
Conclusions
The dendritoma vaccine has minimal toxicity profile with potential clinical benefit. There was OS advantage for NED stage IV patients, those receiving higher number of doses and increased frequency. Based on these results, we initiated a phase IIb trial utilizing improved dendritoma technology in the adjuvant setting for NED stage III/IV melanoma patients.
Similar content being viewed by others
Introduction
Over the past 30 years, the increasing incidence of melanoma has elevated it to the fifth and sixth most common cancer in men and women, respectively [1]. While melanoma accounts for only 4 % of dermatologic cancers, it is responsible for 80 % of skin cancer-related deaths, indicative of the high mortality rate associated with advanced melanoma [2]. Historically, standard of care therapies including surgery, radiation and non-specific chemotherapy (i.e. dacarbazine) resulted in largely disappointing and non-durable clinical outcomes [3]. As our understanding of melanoma has evolved, immunotherapy has become an increasingly important part of treatment regimens, starting with the introduction of the cytokine therapies, interleukin-2 (IL-2) and interferon-α, in the 1990s [4, 5].Though cytokine therapy has achieved a slightly more durable response than chemotherapy, overall response rates remain low at 15–20 % [4, 6]. These disappointing results, coupled with the high mortality rate of advanced melanoma, have left investigators searching for a more effective option.
Given the improvement with cytokine therapy, the logical place to search for a cure for advanced melanoma was in the field of immunotherapy. Checkpoint inhibitors (CPI), which aim to unleash the immune system by limiting auto-regulation, were investigated and found to provide durable clinical response in several disease models, most notably in melanoma and renal cell carcinoma, where immunotherapy had already shown benefit [7–9]. Ipilimumab (Yervoy), a monoclonal antibody against the cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) receptor, became the first CPI approved by the Food and Drug Administration (FDA) in 2011 and has been shown to increase the median overall survival (OS) in patients with metastatic melanoma [7, 8]. In late 2014, pembrolizumab (Keytruda) and nivolumab (Opdivo), PD-1 blocking CPI, were approved by the FDA in patients with unresectable or metastatic melanoma with progression on ipilimumab and a BRAF inhibitor if BRAF V600 mutation is positive [10, 11]. Although survival data have been encouraging with 15–20 % complete clinical responses and reports of long-term survival in some patients, the non-specific nature of CPI has led to high grade adverse events (≥grade 3 in >10–50 %), most often autoimmune or inflammatory in nature [7, 9–16]. Predictably, as combinations of these CPI have been investigated, even more toxicity has been demonstrated [13, 14]. Though their widespread application is limited by toxicity, the CPI class, which activates T cells against tumor cells as opposed to directly attacking them, has demonstrated the power of the immune system to recognize and destroy established cancers.
The success of CPI in treating melanoma has led to increased interest in melanoma vaccines, which theoretically offer similar anti-tumor mechanisms without the toxicities of CPI. Provenge (Sipuleucel-T), a dendritic cell (DC) vaccine for prostate cancer, gained FDA approval in 2010 and remains the only approved cancer vaccine [17, 18]. Provenge has demonstrated an improvement in OS for late-stage prostate cancer patients without significant toxicity, demonstrating the promise of cancer vaccines. Similar to the majority of melanoma vaccines tested to date, however, Provenge is antigen-specific and targets only the subset of patients whose tumors express this one antigen. Our approach uses autologous DCs, similar to Provenge, but exposes them to the full repertoire of tumor antigens from an individual’s cancer, making it applicable to anyone, yet specific to their tumor.
We have isolated highly purified hybrid cells from fusion of autologous DCs and tumor cells instantly and without culture, and named these cells dendritomas [19, 20]. Prior to initiation of our phase I and IIa trials, both animal models and in vitro human testing showed dendritomas made from subjects’ peripheral blood DCs and autologous primary tumor cells effectively produced tumor-specific anti-tumor immunity [20–26]. The aim of this trial was to establish a safe, optimized dosing schedule with secondary goals of evaluating OS. Here, we present the clinical results of our phase I/IIa trial in late-stage melanoma patients.
Methods
Patient characteristics
The study was a prospective, single institution trial in the Greenville Hospital System approved by the institutional review board and monitored by the FDA under investigational new drug #8851. Enrollment criteria included histologically confirmed metastatic melanoma, with an expected survival of 3–6 months and Eastern Cooperative Oncology Group performance status of ≤3. Inclusion criteria also required adequate pulmonary function (forced expiratory volume in 1 s > 25 % of predicted or diffusion capacity of the lungs for carbon monoxide >25 % of predicted), adequate cardiac function, serum creatinine <1.6, hemoglobin >9.0, white blood cell count >3000, platelet count >100,000 and no history of a seizure disorder. The previous treatment with chemotherapy or immunosuppressive agents must have been discontinued at least 30 days prior to vaccination and previous treatment with other forms of immunotherapy discontinued 6 months prior to vaccination unless progression of disease was documented. Central nervous system metastases were allowed, and there were no limitations on tumor location or volume.
Vaccine preparation
Tumor preparation, DC preparation and dendritoma creation were performed as described by Holmes et al. [20]. Briefly, autologous DCs were isolated from a peripheral blood draw, matured and stained fluorescent green. A tumor volume of >1 cm3 was necessary for vaccine preparation for each patient; collected via oncologic surgical resection or biopsy. Twenty patients had an oncologic surgical resection, while the other five had a surgical biopsy to collect needed tumor volume. The tumor tissue was reduced to single cell suspension and stained red fluorescent. The tumor suspension was then fused with the DC; successful creation of the dendritoma was confirmed by the dual fluorescent staining of red and green [20]. Vaccines consisted of 100,000–1,000,000 (mean 504,024 ± 52,802) dendritomas. The number of dendritomas in each patient’s vaccine varied depending on the yield from the culture and fusion process. After irradiation, dendritomas were then re-suspended in 2–3 ml of normal saline, and within 24 h of re-suspension injected into the patient immediately adjacent to a lymph node basin.
Treatment protocols
Phase I was completed as shown in Fig. 1a. Patients were inoculated with doses of 0.25−1.0 × 106 dendritomas every 3 months, up to a maximum of five vaccinations, depending on the availability of dendritomas and/or disease progression. Starting day one after the first inoculation of dendritoma, IL-2 was administered daily by subcutaneous injection for a total of 5 days. IL-2 doses started at 3mIU/m2/day and increased by 3mIU/m2/day to a maximum dose of 9mIU/m2/day. Each patient was pre-medicated 1 h prior to IL-2 injection with Claritin (10 mg) and Celebrex (100 mg) or Relafen (1000 mg). Inoculations two through five were administered in similar fashion to the initial, but without IL-2.
Trial schemas for phase I (a) and IIa (b). a Phase 1: 10 days prior to first inoculation blood samples were taken for autologous serum and dendritic cells. One day prior to inoculation surgical excision was performed. The dendritoma was created and then sorted on day of first inoculation. The first inoculation was followed with IL-2 therapy for 5 days. Re-inoculation occurred every 3 months after evaluation at 90 days. b Phase IIa: the initial preparation was similar to Phase I. The differences occurred with the first inoculation was followed with IL-2 therapy on days one, three and five and re-inoculation occurred every 6 weeks after evaluation at 45 days
Phase IIa was completed as shown in Fig. 1b. Patients were vaccinated with doses from 0.1−1.0 × 106 dendritomas every 6 weeks up to six vaccinations, depending on dendritoma availability. This was not designed as a dose-escalation trial, but rather after the phase I, it was identified that shorter intervals were needed between inoculations to maintain immunity. Thus, the dosing schedule was modified in the phase IIa trial by increasing the frequency of inoculations. With the increased overall doses created, the overall dendritoma dose per inoculation was lower in the phase IIa patients. IL-2 at a dose of 3mIU/m2/day was given on post-vaccination days one, three and five after the first inoculation. Again, re-vaccination was similar to the first, but without IL-2. The IL-2 dosing was modified between the phase I and IIa in an effort to improve the toxicity profile while maintaining similar immune stimulation.
Clinical toxicity and recurrence of disease
Following administration of the vaccine, patients in both phases were assessed for toxicity effects and clinical outcome. Evaluation of disease progression and vital status occurred as dictated by standard of care screening and conducted by the patient’s oncologist. Patients were followed at prescribed intervals throughout progression, if present, and until death when applicable. Patients were monitored for toxicities, which were graded by the National Cancer Institute Common Terminology Criteria for Adverse Events (version 4.0). Immediately post-vaccination, patients were evaluated on days one and three with a complete blood count, creatinine level, liver function tests and clinical examination. Clinical examination, complete blood count, electrolytes, blood urea nitrogen level and creatinine were then completed at 2-week and 1-month follow-up. Computerized tomography scans of the head, chest, abdomen and pelvis were obtained at 3-month intervals and prior to re-vaccination when the two coincided. The measurable residual disease was used for evaluation of response.
Statistical analysis
Median and interquartile range (IQR provided as the first and third quartiles) were used to summarize continuous data with Wilcoxon rank-sum test used to compare groups. Chi-square or Fisher’s exact test was utilized to compare groups proportionally. Kaplan–Meier curves were used to quantify OS, and a simple log-rank test was used to compare between groups. A p value < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 22 (Armonk, NY: IBM Corp.).
Results
Demographics
A total of 25 stage IV melanoma patients were enrolled in the phase I/IIa study. The overall demographics data are given in Table 1. The median age was 62 years old (IQR 52–68), and 44 % were male (n = 11). Prior to inoculation, 80 % underwent at least one oncologic surgical resection and 60 % of patients underwent multi-modality treatments. All patients had progressed to stage IV disease before enrollment, but six had no evidence of disease (NED) prior to inoculation. Five of the NED patients underwent oncologic surgical resection, while one patient underwent radiation and chemotherapy and was deemed NED prior to initiation of the dendritoma vaccinations.
Toxicity
All study drug-related toxicity was less than grade 3 with flu-like symptoms being the most common. The most common adverse events include systemic fever (60 %), chills (32 %), nausea (28 %), arthralgias/myalgias (28 %) and erythema (20 %). Phase I had greater toxicity overall (p = 0.004), although phase IIa patients had a non-significant increase in neurologic and skin manifestation (p = 0.61 and p = 0.79, respectively; Fig. 2). The skin-specific toxicities from both trials appeared after the IL-2 administration and included bruising, erythema, facial flushing and swelling, pruritus, rash and local swelling; there were no skin-specific toxicities following the dendritoma administration.
Toxicity by system for phase I and phase IIa patients. The phase I patients experienced more overall toxicities, in all areas except neurologic and skin compared to the phase IIa patients. The most common adverse events experienced by patients in phase I included fever (100 %), chills (50 %), hypotension (40 %), nausea (40 %), anemia (40 %), arthralgia/myalgia (30 %), weight gain (30 %), stomatitis (30 %) and edema (30 %). The most common adverse events in the phase IIa were headache (27 %), dizziness (13 %), erythema (33 %) and rash (20 %)
There were four serious adverse events, which were investigated and deemed unrelated to the dendritoma vaccine. One patient died 19 days after the first vaccination, but the cause of death was determined to be progressive disease. Another patient experienced thrombocytopenia that required splenectomy 73 days after the last vaccination. A third patient experienced grade 3 chest pain on the first day of treatment administration. The pain subsequently resolved, and all cardiac tests were normal with no repeat episodes experienced after subsequent vaccination. Another patient experienced gastric bleeding that was most likely caused by warfarin therapy. The same patient also experienced hypoxia after IL-2 administration and blood transfusions for treatment of anemia; this patient had a significant past medical history of congestive heart failure and hypoxia requiring hospitalization.
Clinical outcomes
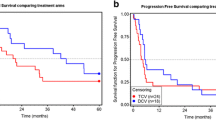
Median OS was 16.1 months (IRQ 8.7–23.8 months), compared to 8–10 months expected OS using stage-matched historical controls [3]. The Kaplan–Meier 5-year estimated survival rate was 29.2 % compared to 10–12 % for historical controls (Fig. 3a) [3]. On subset analysis, there were no differences in OS based on age (p = 0.42), gender (p = 0.96), time to treatment (p = 0.67), initial presenting stage (p = 0.59) or dendritoma dosage (p = 0.15). A significant improvement in estimated OS was observed in patients receiving ≥3 versus those receiving <3 inoculations (43.1 vs. 16.7 %, p = 0.02; Fig. 3b). To avoid survival bias, an additional evaluation excluding patients that did not survive >6 months (n = 4) and, therefore, were unable to complete the inoculations was performed. After this exclusion, patients receiving ≥3 doses (n = 13) continued to show the potential clinical benefit of more doses with improved median OS compared to those receiving <3 doses (n = 8; median OS 21.5, IQR 14.2–30.9 vs. 13.4, IQR 8.5–23.6 months; p = 0.18). Furthermore, the estimated 5-year DFS in this population still trended toward favoring ≥3 inoculations (43.1 vs. 25.0 %; p = 0.19). A statistically significant improvement in survival was noted in patients who were NED (n = 6) at the time of initial vaccination compared to those patients who had evidence of disease (80 vs. 14 %, p = 0.005; Fig. 3c). The final clinical outcomes of the patients who were NED prior to inoculation included continued NED in 50 % (n = 3), alive with disease in 33 % (n = 2) and expired in 17 % (n = 1). At final analysis of the trial, eight patients (32 %) were alive with a median follow-up of 31.9 months (IQR 23.2–36.5 months). Four of these patients (50 %) had stable disease, one (12.5 %) had progressive disease, and three (37.5 %) remained disease-free.
Phase I versus phase IIa
Comparison of the phase I with the IIa trial revealed no significant differences with respect to age, gender, initial stage, stage at inoculation, NED status prior to inoculation or prior treatments received (Table 2, all p > 0.1). Differences, however, were noted in the average dendritoma dose, as well as in the interval between doses, with phase I patients getting higher doses (757,130 ± 90,420 vs. 382,744 ± 35,750, p < 0.01), but at longer intervals (108.1 ± 14.8 vs. 44.3 ± 3.5 days, p < 0.01). Overall, as expected by the protocol differences, phase I patients received more doses of IL-2 (5 vs. 3 doses).
Phase IIa patients had a significantly increased median OS compared to phase I patients (28.7, IRQ 15.7–29.8 vs. 8.7, IRQ 2.9–11.7 months; p = 0.01). On 5-year projected survival analysis, phase IIa patients again had a significantly increased survival compared to phase I (41.1 vs. 10 %, p = 0.004, Fig. 3d). There were more NED patients in the Phase IIa trial, though the difference was not statistically significant (33 vs. 10 %, p = 0.12). If the NED prior to inoculation patients were excluded from both trials, the 5-year estimated survival was 26.7 vs. 0 % (IIa vs. I, respectively; p = 0.003).
Discussion
The results of our phase I/IIa trial of the dendritoma vaccine show another promising avenue for harnessing the power of the immune system to defeat melanoma. Although this initial trial was small, the dendritoma vaccine produced a median survival of 16.1 months and a projected 5-year survival of 29.2 %, a vast improvement over historical controls (median survival 8–10 months and 5-year survival 10–12 %) [3] and a clinical benefit that is similar in magnitude to CPI therapy [7, 13, 24, 27]. Additionally, the survival curve in our trial flattens after 30 months (Fig. 3a), much like the survival curve seen with ipilimumab therapy, suggesting the potential for similar long-term efficacy [12].
The real promise of the dendritoma vaccine is that it may produce clinical efficacy comparable to CPI, but without the significant toxicity. In the ipilimumab approval trial, drug-related adverse events were experienced in 80 % of patients receiving ipilimumab alone, with two-thirds of these being immune-related and 22 % of all toxicities ≥grade 3. There were even 14 deaths (2.2 %) related to the study drug, 50 % of which were related to immune-related adverse events [9]. Similarly, nivolumab and pembrolizumab treatment was associated with significant grade ≥3 toxicity (74.3 and 82 %, respectively), forcing some patients to discontinue therapy (6.8 and 9 % of patients, respectively) [10, 11]. Recent attempts to combine CPI to increase efficacy have led to even greater toxicity. Combination nivolumab and ipilimumab therapy caused treatment-related grade 3 or 4 adverse events in 54 % of patients [28]. Clearly, the toxicity profile remains the primary limitation to CPI therapy.
The dendritoma vaccine, on the other hand, does not have significant immune-associated toxicity. In fact, the minimal toxicity seen with vaccination was commonly seen after IL-2 injection. As patients in phase I received higher IL-2 doses than those in phase IIa, we predictably noted more adverse events in the phase I group. While the phase I patients also received a higher number of dendritomas per inoculation, the increased toxicity is not likely related to this because the reactions consistently occurred after the IL-2 injection. Even with this increased toxicity in phase I, no patients had grade 3 toxicities and no patients required discontinuation of therapy because of adverse reactions, which is a vast improvement compared to the CPI. Furthermore, in future trials, IL-2 will be eliminated as the immunoadjuvant; so we anticipate an even lower toxicity rate. We will continue to monitor the possible relationship between number of DC per inoculation and toxicity. Overall, this evidence of efficacy without significant toxicity opens the possibility for wide applicability of the dendritoma or similar vaccine.
In addition to the minimal toxicity profile and promising overall analysis of the dendritoma vaccine, further analyses revealed even better outcomes in certain subgroups. While the NED group was small, we saw a signal toward benefit in this subgroup with a statistically significant difference between patients who were NED prior to inoculation and those who had evidence of disease. The vaccine showed its highest efficacy in these stage IV NED patients, with an estimated 5-year survival of 80 %. While it is somewhat intuitive that these patients may do better with the vaccine, historically only 20–30 % of resected stage IV patients are alive at 5 years [29]. This subgroup had a small number of patients and will need to be studied further in future trials, but the data suggest that the dendritoma vaccine may be best used in the setting of fully resected patients at significant risk of recurrence.
The majority of immune therapies discussed here have been tested in late-stage melanoma patients, where treatments are rarely successful. Cancer vaccines have been tested in this setting as well and have, likewise, shown minimal benefit [19, 30–39]. Current data suggest that the best time to intervene with a vaccine, and likely all immunotherapy, is actually the adjuvant setting after patients have been rendered disease-free by standard of care therapies, as appears to be the case with the dendritoma vaccine [19, 39–48]. With this strategy in mind, initial attempts have been made to utilize CPI in completely resected stage III melanoma patients. Ipilimumab was shown to prolong DFS in the EORTC 18071 trial, but only if patients could tolerate the toxicities. The median DFS was extended by 9 months using ipilimumab (DFS 26.1 vs. 17.1 months), with the 3-year DFS of 46.5 % in the ipilimumab group vs. 34.8 % in the control group (p = 0.0013). Within this study, however, 52 % of patients in the ipilimumab arm discontinued treatment secondary to adverse events, and 39 % were unable to complete the induction therapy. Overall, 90 % of patients on ipilimumab experienced an immune-related adverse event, with 42 % experiencing a grade 3–5 immune-related event. There were also five documented deaths (1 %) within the treatment arm related to ipilimumab [49]. While the high level of toxicity associated with CPI may be acceptable in the setting of advanced disease where effective treatment options are limited, the same is not true for the adjuvant setting. Here, the tolerance for significant toxicity in a population that may or may not benefit from therapy is considerably lower. Fortunately, in contrast to CPI, the dendritoma vaccine’s toxicity profile is much more realistic for the adjuvant setting. In the setting of fully resected disease, the dendritoma-induced immune response can attack any minimal residual disease and potentially provide long-term protection through immunologic memory with minimal toxicity.
In further subset analysis, we also noted significant improvement in patients receiving at least 3 inoculations, with a Kaplan–Meier 5-year estimated survival of 43.1 % compared to only 16.7 % in those receiving fewer inoculations (p = 0.02). Even when patients who did not survive >6 months (and, therefore, were unable to complete the vaccinations) were excluded from the same analysis, there was still an 8 months OS advantage (21.5 vs. 13.4 months; p = 0.18) and trend toward improved 5-year estimated survival (43.1 vs. 25.0 %; p = 0.19) in patients receiving ≥3 doses versus <3 doses. While some of this difference is explained by patients who were not able to complete vaccinations due to disease progression, there was clearly an improvement in response to patients receiving more inoculations at a higher frequency, as is also indicated by the increase estimated survival in phase IIa compared with phase I patients (41.1 vs. 10 %, p = 0.01). Even though the phase IIa patients received lower doses of IL-2 and dendritoma, they demonstrated better outcomes. Because there was a non-significant increase in NED patients in the phase IIa group, we re-assessed the estimated survival after excluding the NED patients from both trials and found a persistent benefit in the phase IIa versus phase I (estimated 5-year survival of 26.7 vs. 0 %, p = 0.003). Thus, the increased frequency and higher number of doses likely resulted in the better outcomes in the phase IIa. Based on these cumulative findings from the phase I/IIa trials, autologous tumor/DC vaccines, to include the dendritoma vaccine, should be given with increased frequency, with a higher number of doses and preferably tested in the adjuvant setting.
The dendritoma vaccine has potential clinical benefit, but this trial does have limitations. First, the sample size is very small, making definitive statements on survival difficult. Despite this limitation, the findings justify further investigation on a larger scale to truly demonstrate the potential clinical benefit. Second, although the trial was limited to stage IV patients, the enrolled patients included varying amounts of disease burden and the trial was underpowered to show a difference between the NED and patients with residual disease. Another limitation is the lack of data to serve as a surrogate to clinical efficacy, as is customarily presented in a phase I/II trial. The dendritoma technology does not lend itself easily to immunologic monitoring data. We have no ability to know exactly which specific tumor-associated antigen (TAA) is selected and presented with the autologous DC as the entire antigenic repertoire from the autologous tumor is provided to the DC. Thus, tracking T-cell responses to one TAA is not practical nor necessarily relevant. Once the dendritomas are injected intradermally, they will access the subdermal lymphatic plexus and travel to the draining lymph node and activate T-cells. This process does not produce a local reaction to measure. With no immune surrogate to measure, we are left with survival and recurrence data as the only marker of clinical efficacy. In our future trials, we will be testing patients to a panel of known melanoma TAA in an attempt to monitor vaccine-induced immune responses. Though this trial does have limitations, there are findings that cannot be ignored and merit further investigation.
While the dendritoma vaccine holds great promise, particularly with correct dosing and in the adjuvant setting, the dendritoma fusion technology is very labor intensive and not scalable, making it challenging to commercialize. The key underlying principle to the dendritoma vaccine is the introduction of the entire antigenic repertoire of the patient’s tumor cell into the cytoplasm of the dendritic cell. This specific delivery leads to preferential use of the endogenous antigen processing pathway, major histocompatibility complex class I presentation and a subsequent anti-tumor CTL response. Further investigation has led to a novel technology, which requires less tumor tissue and uses a more efficient vaccine production process. Autologous tumor lysate (TL) is loaded into yeast cell wall particles that are naturally and efficiently taken up into the patient’s dendritic cells. These autologous tumor lysate, particle-loaded, dendritic cells (TLPLDC) are then injected intradermally, similar to the dendritoma vaccine. The in vivo effectiveness of the TLPLDC was assessed in a murine melanoma pulmonary metastasis model in which animals were treated with a TLPLDC vaccine, dendritoma vaccine or control. Upon death of the first animal, all were killed, pulmonary metastases were totaled, and groups were compared. This comparison found the TLPLDC to have 0 metastases versus dendritoma with 3.13 metastases versus controls with >112 metastases (p < 0.01) [50]. With this animal study showing the TLPLDC to be as good as or better than the dendritoma vaccine fusion technique [50], we can translate the promising results of the dendritoma vaccine into a more scalable and economically feasible treatment strategy, while maintaining its wide applicability to many types of solid tumors. To this end, an open label trial in patients with any type of solid tumor was started utilizing the TLPLDC vaccine technology [25, 26, 51]. To date, 20 patients have been vaccinated with an autologous TLPLDC vaccine resulting in an overall 60 % clinical beneficial response rate [complete response + partial response + stable disease (CR + PR + SD)], a 30 % objective response rate (CR + PR) among all vaccinated patients; the one CR was seen in a melanoma patient [51].
Using the lessons learned from the dendritoma trial and the newer technology of TLPLDC, we have initiated a phase IIb trial (NCT02301611) utilizing the latter. The trial is a prospective, randomized, double-blinded, placebo-controlled, multi-institution adjuvant trial to prevent recurrence in resected stage III and IV melanoma patients. The study will enroll patients identified prior to definitive surgery and anticipated to be clinically disease-free after surgery. A total of 120 patients will be randomized to autologous TLPLDC versus dendritic cells with unloaded particles. The primary endpoint will be disease-free survival at 24 months. Enrollment started at the beginning of 2015, and trial completion is expected within 3 years. The future of melanoma treatment is rapidly evolving, and it is clear that multiple treatment approaches will be necessary. With this in mind, we have plans for an additional trial in more advanced melanoma patients combining the TLPLDC vaccine to standard of care CPI. We hope combination of these strategies will increase the efficacy of the vaccine by diminishing obstructions to a strong vaccine-induced anti-tumor immune response, while maintaining low toxicity.
Conclusions
In this phase I/IIa trial of the dendritoma vaccine for advanced stage melanoma, we have shown potential promising results compared to historical controls [3]. Importantly, we have shown this vaccine to have a minimal toxicity profile, particularly when compared to recently FDA approved CPI. The greatest benefit from the dendritoma vaccine was demonstrated in patients with stage IV disease, who were rendered disease free prior to initiation of inoculations. With this information and newer DC loading technology, we have initiated a phase IIb trial (NCT02301611) in stage III/IV resected melanoma patients in the adjuvant setting with a goal to prevent recurrence with this non-toxic therapy.
Abbreviations
- CPI:
-
Checkpoint inhibitors
- CR:
-
Complete response
- CTLA-4:
-
Cytotoxic T-lymphocyte-associated antigen 4
- DC:
-
Dendritic cell
- ED:
-
Evidence of disease
- FDA:
-
Food and Drug Administration
- IL-2:
-
Interleukin-2
- IQR:
-
Interquartile range
- NED:
-
No evidence of disease
- OS:
-
Overall survival
- PR:
-
Partial response
- SD:
-
Stable disease
- SEM:
-
Standard error of means
- TAA:
-
Tumor-associated antigen
- TL:
-
Tumor lysate
- TLPLDC:
-
Tumor lysate particle-loaded dendritic cells
References
Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63(1):11–30
Miller AJ, Mihm MC Jr (2006) Melanoma. N Engl J Med 355(1):51–65
Tsao H, Atkins MB, Sober AJ (2004) Management of cutaneous melanoma. N Engl J Med 351(10):998–1012
Sasse AD, Sasse EC, Clark LG, Ulloa L, Clark OA (2007) Chemoimmunotherapy versus chemotherapy for metastatic malignant melanoma. Cochrane Database Syst Rev 1:CD005413
Atkins MB, Kunkel L, Sznol M, Rosenberg SA (2000) High-dose recombinant interleukin-2 therapy in patients with metastatic melanoma: long-term survival update. Cancer J Sci Am 6(Suppl 1):S11–S14
Keilholz U, Punt CJ, Gore M et al (2005) Dacarbazine, cisplatin, and interferon-alfa-2b with or without interleukin-2 in metastatic melanoma: a randomized phase III trial (18951) of the European organisation for research and treatment of cancer melanoma group. J Clin Oncol 23(27):6747–6755
Naidoo J, Page DB, Wolchok JD (2014) Immune checkpoint blockade. Hematol Oncol Clin North Am 28(3):585–600
Sharma P, Wagner K, Wolchok JD, Allison JP (2011) Novel cancer immunotherapy agents with survival benefit: recent successes and next steps. Nat Rev Cancer 11(11):805–812
Hodi FS, O’Day SJ, McDermott DF et al (2010) Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 363(8):711–723
Robert C, Ribas A, Wolchok JD et al (2014) Anti-programmed-death-receptor-1 treatment with pembrolizumab in ipilimumab-refractory advanced melanoma: a randomised dose-comparsion cohort of a phase 1 trial. Lancet 384(9948):1109–1117
Robert C, Long GV, Brady B et al (2015) Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med 372(4):320–330
Robert C, Thomas L, Bondarenko I et al (2011) Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med 364(26):2517–2526
Wolchok JD, Kluger H, Callahan MK et al (2013) Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med 369(2):122–133
Ott PA, Hodi FS, Robert C (2013) CTLA-4 and PD-1/PD-L1 blockade: new immunotherapeutic modalities with durable clinical benefit in melanoma patients. Clin Cancer Res 19(19):5300–5309
McDermott D, Haanen J, Chen TT, Lorigan P, O’Day S, Investigators MDX (2013) Efficacy and safety of ipilimumab in metastatic melanoma patients surviving more than 2 years following treatment in a phase III trial (MDX010-20). Ann Oncol 24(10):2694–2698
Hamid O, Robert C, Daud A et al (2013) Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med 369(2):134–144
Kantoff PW, Higano CS, Shore ND et al (2010) Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med 363(5):411–422
Kantoff PW, Schuetz TJ, Blumenstein BA et al (2010) Overall survival analysis of a phase II randomized controlled trial of a Poxviral-based PSA-targeted immunotherapy in metastatic castration-resistant prostate cancer. J Clin Oncol 28(7):1099–1105
Schneble EJ, Yu X, Wagner T, Peoples GE (2014) Novel dendritic cell-based vaccination in late stage melanoma. Human Vaccines Immunother 10(11):3132–3138
Holmes LM, Li J, Sticca RP, Wagner TE, Wei Y (2001) A rapid, novel strategy to induce tumor cell-specific cytotoxic T lymphocyte responses using instant dentritomas. J Immunother 24(2):122–129
Gong J, Chen D, Kufe D (1997) Induction of antitumor activity by immunization with fusions of dendritic carcinoma cells. Nat Med 3:558–561
Wang J, Saffold S, Cao X et al (1998) Eliciting T cell immunity against poorly immunogenic tumors by immunization with dendritic cell-tumor fusion vaccines. J Immunol 161:5516–5524
Lespagnard L, Mettens P, Verheyden A et al (1998) Dendritic cells fused with mastocytoma cells elicit therapeutic antitumor immunity. Int J Cancer 76:250–258
Cao X, Zhang W, Wang J et al (1999) Therapy of established tumor with a hybrid cellular vaccine generated by using granulocyte-macrophage colony-stimulating factor genetically modified dendritic cells. Immunology 97:616–625
Wei Y, Sticca RP, Holmes LM et al (2006) Dendritoma vaccination combined with low dose interleukin-2 in metastatic melanoma patients induced immunological and clinical responses. Int J Oncol 28(3):585–593
Wei YC, Sticca RP, Li J et al (2007) Combined treatment of dendritoma vaccine and low-dose interleukin-2 in stage IV renal cell carcinoma patients induced clinical response: a pilot study. Oncol Rep 18(3):665–671
Mahoney KM, Freeman GJ, McDermott DF (2015) The next immune-checkpoint inhibitors: PD-1/PD-L1 blockade in melanoma. Clin Ther 37(4):764–782
Postow MA, Chesney J, Pavlick AC et al (2015) Novolumab and ipilimumab versus ipilimumab in untreated melanoma. N Engl J Med 372:2006–2017
Wasif N, Bagaria S, Ray P, Morton D (2011) Does metastectomy improve survival in patients with stage IV melanoma? A cancer registry analysis of outcomes. J Surg Oncol 104(2):111–115
Kaufman HL (2012) Vaccines for melanoma and renal cell carcinoma. Semin Oncol 39:263–275
Klein O, Schmidt C, Knights A et al (2011) Melanoma vaccines: developments over the past 10 years. Expert Rev Vaccines 10:853–873
Kawakami Y, Robbins PF, Wang RF et al (1998) The use of melanosomal proteins in the immunotherapy of melanoma. J Immunother 21:237–246
Slingluff CL Jr, Petroni GR, Yamshchikov GV et al (2003) Clinical and immunologic results of a randomized phase II trial of vaccination using four peptides either administered in granulocyte-macrophage colony-stimulating factor in adjuvant or pulsed on dendritic cells. J Clin Oncol 21:4016–4026
Slingluff CL Jr, Petroni GR, Olson WC et al (2009) Effect of granulocyte/macrophage colony-stimulating factor on circulating CD8+ and CD4+ T-cell responses to a multi-peptide melanoma vaccine: outcome of a multicenter randomized trial. Clin Cancer Res 15:7036–7044
Block MS, Suman VJ, Nevala WK et al (2011) Pilot study of granulocyte-macrophage colony-stimulating factor and interleukin-2 as immune adjuvants for a melanoma peptide vaccine. Melanoma Res 21:438–445
Kruit WH, van Ojik HH, Brichard VG et al (2005) Phase I/2 study of subcutaneous and intradermal immunization with a recombinant MAGE-3 protein in patients with detectable metastatic melanoma. Int J Cancer 117:596–604
Kruit WH, Suciu S, Dreno B et al (2013) Selection of immunostimulant AS15 for active immunization with MAGE-A3 protein: results of a randomized phase II study of the European organisation for research and treatment of cancer melanoma group in metastatic melanoma. J Clin Oncol 31:2413–2421
Sabado RL, Pavlick AC, Gnjatic S, et al (2012) Phase I/II study of resiquimod as an immunologic adjuvant for NY-ESO-1 protein vaccination in patients with melanoma. ASCO Annual Meeting Abstracts. J Clin Oncol 30:Abstract 2589
Weiss SA, Chandra S, Pavlick AC (2014) Update on vaccine for high-risk melanoma. Curr Treat Options Oncol 15:269–280
Kirkwood JM, Dreno B, Hauschild A, et al. (2011) DERMA phase III trial of MAGE-A3 antigen-specific cancer immunotherapeutic (ASCI) as adjuvant therapy in patients with MAGE-A3-positive resected stage III melanoma. ASCO Annual Meeting Abstracts. J Clin Oncol 29:Suppl Abstract TPS232
Eggermont AMM, Suciu S, Rutkowski P et al (2013) Adjuvant ganglioside GM2-KLH/QS-21 vaccination vs observation after resection of primary tumor 1.5 mm in patients with stage II melanoma: results of the EORTC 18961 randomized phase III trial. J Clin Oncol 31:3831–3840
Morton DL, Hseuh EC, Essner R et al (2002) Prolonged survival of patients receiving active immunotherapy with canvaxin therapeutic polyvalent vaccine after complete resection of melanoma metastatic to regional lymph nodes. Ann Surg 236:438–449
Hsueh EC, Essner R, Foshag LJ et al (2002) Prolonged survival after complete resection of disseminated melanoma and active immunotherapy with a therapeutic cancer vaccine. J Clin Oncol 20:4549–4554
Tsioulias GJ, Gupta RK, Tisman G et al (2001) Serum TA90 Antigen-antibody complex as a surrogate marker for the efficacy of a polyvalent allogeneic whole-cell vaccine (CancerVax) in melanoma. Ann Surg Oncol 8:198–203
Mackiewic A, Mackiewicz J, Wysocki PJ et al (2012) Longterm survival of high-risk melanoma patients immunized with a Hyper-IL-6-modified allogeneic whole-cell vaccine after complete resection. Expert Opin Investig Drugs 21:773–783
Markowicz S, Nowecki ZI, Rutkowski P et al (2012) Adjuvant vaccination with melanoma antigen-pulsed dendritic cells in stage III melanoma patients. Med Oncol 29:2966–2977
Petenko NN, Mikhaylova IN, Chkadua GZ et al (2012) Adjuvant dendritic cell (DC)-based vaccine therapy of melanoma patients. ASCO Annual Meeting Abstracts. J Clin Oncol. 30:Abstract 2524
Andtbacka RHI, Collichio F, Amatruda T, et al. (2013) OPTIM: a randomized phase 3 trial of talimogene laherparepvec (T-VEC) vs subcutaneous granulocyte macrophage colony-stimulating factor for the treatment of unresectable stage IIIB/C and IV melanoma. ASCO Annual Meeting Abstracts. J Clin Oncol 31:Abstract LBA9008
Eggermont A, Chairion-Sileni V, Grob JJ et al (2015) Adjuvant ipilimumab versus placebo after complete resection of high-risk stage III melanoma (EORTC 18071): a randomised, double-blind phase 3 trial. Lancet Oncol 16:522–530
Jackson D, Greene J, Hale D et al (2015) Preclinical testing of a novel personalized cancer vaccine for all solid tumors and all patients. J ImmunoTherapy Cancer 3(Suppl 2):P208
Greene JM, Hale DF, Schneble EJ, et al. (2015) Initial phase I/IIa trial results of an autologous tumor lysate + yeast cell wall particles + dendritic cells vaccine (TLPLDC) in patients with solid tumors. In: CRI-CIMT-EATI-AACR: the inaugural international cancer immunotherapy conference: translating science into survival. New York. AACR:Abstract A044
Acknowledgments
We would like to thank the patients for participating and all of the study personnel for their diligent work and efforts in the conduction of this trial. We are especially indebted to Dr. Samuel W. Smith for his invaluable assistance and advice throughout these studies.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Dr. Thomas Wagner is the Chief Executive Officer and Dr. George Peoples is the Chief Medical Officer of Orbis Health Solutions. All other authors declare no conflicts of interest.
Additional information
The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of San Antonio Military Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, Department of Defense or the U.S. Government.
Rights and permissions
About this article
Cite this article
Greene, J.M., Schneble, E.J., Jackson, D.O. et al. A phase I/IIa clinical trial in stage IV melanoma of an autologous tumor–dendritic cell fusion (dendritoma) vaccine with low dose interleukin-2. Cancer Immunol Immunother 65, 383–392 (2016). https://doi.org/10.1007/s00262-016-1809-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-016-1809-6