Abstract
Objective
To compare the efficacy (including blood pressure, medication reduction, serum potassium, and clinical success) and safety parameters (including operative time, length of hospital stay, blood loss, hypertension crisis rate, and complication rate) of radiofrequency ablation (RFA) and laparoscopic adrenalectomy (LA) in the treatment of primary aldosteronism (PA).
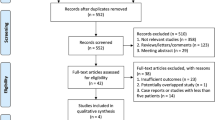
Methods
Literature search was performed on PubMed, EMBASE, The Cochrane Library (Issue 8, 2023), Web of Science, China National Knowledge Infrastructure, and Wanfang from inception to August 2023. Study selection, data extraction, and risk of bias assessment were performed by two independent reviewers. Quality assessment was conducted using the Newcastle–Ottawa scale. The Stata 12.0 software was used for statistical analyses. Pooled odds ratios (OR) with corresponding 95% confidence interval (CI) were calculated for categorical outcomes, while mean difference (MD) with corresponding 95% CI were calculated for continuous outcomes.
Results
A total of 5 studies involving 204 patients (LA, n = 127; and RAF, n = 77) were included. LA had better diastolic blood pressure control than RFA (WMD = 5.19; 95% CI 0.96–9.43); however, the RFA demonstrated better shorter operative time (WMD = − 57.99; 95% CI − 116.54 to 0.57), and shorter length of hospital stay (OR − 1.6; 95% CI − 2.37 to − 0.83) compared to LA. All remaining parameters were comparable between the interventions.
Conclusion
While grossly comparable in efficacy as treatment options for PA, RFA may allow for shorter operative time and hospital stay, less intraoperative blood loss, and lower hospitalization costs. However, LA has better diastolic blood pressure control. Even so, we still need larger prospective studies, specifically with comparative hypertension response (short and long term) and number of post-procedural antihypertensive medication requirement.



Similar content being viewed by others
References
Auchus RJ. Approaching primary aldosteronism as a common disease. Endocr Pract. 2023.
Sudano I, Suter P, Beuschlein F. Secondary hypertension as a cause of treatment resistance. Blood Press. 2023;32(1):2224898.
Nezu K, Kawasaki Y, Morimoto R, Ono Y, Omata K, Tezuka Y, et al. Impact of Adrenalectomy on Diastolic Cardiac Dysfunction in Patients with Primary Aldosteronism. Tohoku J Exp Med. 2023;259(3):229-36.
Buffolo F, Tetti M, Mulatero P, Monticone S. Aldosterone as a Mediator of Cardiovascular Damage. Hypertension. 2022;79(9):1899-911.
Aune A, Gerdts E, Kokorina M, Kringeland E, Midtbø H, Løvås K, et al. Persistent cardiac organ damage in surgically and medically treated primary aldosteronism. J Hypertens. 2022;40(6):1204-11.
Otsuka H, Abe M, Kobayashi H. The Effect of Aldosterone on Cardiorenal and Metabolic Systems. Int J Mol Sci. 2023;24(6).
Calhoun DA. Is there an unrecognized epidemic of primary aldosteronism? Pro. Hypertension. 2007;50(3):447-53; discussion -53.
Libianto R, Stowasser M, Russell G, Fuller PJ, Yang J. Improving Detection Rates for Primary Aldosteronism. Exp Clin Endocrinol Diabetes. 2023;131(7-08):402-8.
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2018;6(1):41-50.
Mete O, Erickson LA, Juhlin CC, de Krijger RR, Sasano H, Volante M, et al. Overview of the 2022 WHO Classification of Adrenal Cortical Tumors. Endocr Pathol. 2022;33(1):155-96.
Young WF, Jr. Diagnosis and treatment of primary aldosteronism: practical clinical perspectives. J Intern Med. 2019;285(2):126-48.
Katsuragawa S, Goto A, Shinoda S, Inoue K, Nakai K, Saito J, et al. Association of Reversal of Renin Suppression With Long-Term Renal Outcome in Medically Treated Primary Aldosteronism. Hypertension. 2023;80(9):1909-20.
Zhou Y, Wang X, Hou J, Wan J, Yang Y, Liu S, et al. A controlled trial of percutaneous adrenal arterial embolization for hypertension in patients with idiopathic hyperaldosteronism. Hypertens Res. 2023.
Mullen N, Curneen J, Donlon PT, Prakash P, Bancos I, Gurnell M, et al. Treating primary aldosteronism-induced hypertension: novel approaches and future outlooks. Endocr Rev. 2023.
Picado O, Whitfield BW, Khan ZF, Jeraq M, Farrá JC, Lew JI. Long-term outcome success after operative treatment for primary aldosteronism. Surgery. 2021;169(3):528-32.
Pang TC, Bambach C, Monaghan JC, Sidhu SB, Bune A, Delbridge LW, et al. Outcomes of laparoscopic adrenalectomy for hyperaldosteronism. ANZ J Surg. 2007;77(9):768-73.
Sukor N, Gordon RD, Ku YK, Jones M, Stowasser M. Role of unilateral adrenalectomy in bilateral primary aldosteronism: a 22-year single center experience. J Clin Endocrinol Metab. 2009;94(7):2437-45.
Tang F, Loh LM, Foo RS, Loh WJ, Lim DST, Zhang M, et al. Tolerability and Efficacy of Long-Term Medical Therapy in Primary Aldosteronism. J Endocr Soc. 2021;5(11):bvab144.
Patel V, Lindquester WS, Dhangana R, Medsinge A. Percutaneous ablation of renal tumors versus surgical ablation and partial nephrectomy: Medicare trends and reimbursement cost comparison from 2010 to 2018. Abdom Radiol (NY). 2022;47(2):885-90.
Fu R, Ling W. The current role of radiofrequency ablation in the treatment of intrahepatic recurrent hepatocellular carcinoma. J Surg Oncol. 2023.
Zhang H, Li Q, Liu X, Zhao Z, He H, Sun F, et al. Adrenal artery ablation for primary aldosteronism without apparent aldosteronoma: An efficacy and safety, proof-of-principle trial. J Clin Hypertens (Greenwich). 2020;22(9):1618-26.
Zhao Z, Liu X, Zhang H, Li Q, He H, Yan Z, et al. Catheter-Based Adrenal Ablation Remits Primary Aldosteronism: A Randomized Medication-Controlled Trial. Circulation. 2021;144(7):580-2.
Charoensri S, Turcu AF. Primary Aldosteronism Prevalence - An Unfolding Story. Exp Clin Endocrinol Diabetes. 2023;131(7-08):394-401.
Cook DA, Reed DA. Appraising the quality of medical education research methods: the Medical Education Research Study Quality Instrument and the Newcastle-Ottawa Scale-Education. Acad Med. 2015;90(8):1067-76.
Yang MH, Tyan YS, Huang YH, Wang SC, Chen SL. Comparison of radiofrequency ablation versus laparoscopic adrenalectomy for benign aldosterone-producing adenoma. Radiol Med. 2016;121(10):811-9.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101(5):1889-916.
Gumbs AA, Gagner M. Laparoscopic adrenalectomy. Best Pract Res Clin Endocrinol Metab. 2006;20(3):483-99.
Fu YF, Cao C, Shi YB, Zhang W, Huang YY. Computed tomography-guided cryoablation for functional adrenal aldosteronoma. Minim Invasive Ther Allied Technol. 2021;30(3):169-73.
Lo CH, Tyan YS, Ueng KC. Immediate Results and Long-Term Outcomes Following Percutaneous Radiofrequency Ablation of Unilateral Aldosterone-Producing Adenoma. Acta Cardiol Sin. 2020;36(2):160-7.
Nunes TF, Szejnfeld D, Xavier AC, Kater CE, Freire F, Ribeiro CA, et al. Percutaneous ablation of functioning adrenal adenoma: a report on 11 cases and a review of the literature. Abdom Imaging. 2013;38(5):1130-5.
Chen J, Wu J, Zhu R, Lu L, Ma XJ. Ablation versus laparoscopic adrenalectomy for the treatment of aldosterone‑producing adenoma: a meta-analysis. Abdom Radiol (NY). 2021;46(6):2795-804.
Guo RQ, Li YM, Li XG. Comparison of the radiofrequency ablation versus laparoscopic adrenalectomy for aldosterone-producing adenoma: a meta-analysis of perioperative outcomes and safety. Updates Surg. 2021;73(4):1477-85.
Liu SY, Chu CM, Kong AP, Wong SK, Chiu PW, Chow FC, et al. Radiofrequency ablation compared with laparoscopic adrenalectomy for aldosterone-producing adenoma. Br J Surg. 2016;103(11):1476-86.
Mulatero P, Monticone S, Deinum J, Amar L, Prejbisz A, Zennaro MC, et al. Genetics, prevalence, screening and confirmation of primary aldosteronism: a position statement and consensus of the Working Group on Endocrine Hypertension of The European Society of Hypertension. J Hypertens. 2020;38(10):1919-28.
Yang R, Xu L, Lian H, Gan W, Guo H. Retroperitoneoscopic-guided cool-tip radiofrequency ablation of adrenocortical aldosteronoma. J Endourol. 2014;28(10):1208-14.
Sarwar A, Brook OR, Vaidya A, Sacks AC, Sacks BA, Goldberg SN, et al. Clinical Outcomes following Percutaneous Radiofrequency Ablation of Unilateral Aldosterone-Producing Adenoma: Comparison with Adrenalectomy. J Vasc Interv Radiol. 2016;27(7):961-7.
Mendiratta-Lala M, Brennan DD, Brook OR, Faintuch S, Mowschenson PM, Sheiman RG, et al. Efficacy of radiofrequency ablation in the treatment of small functional adrenal neoplasms. Radiology. 2011;258(1):308-16.
Cano-Valderrama O, González-Nieto J, Abad-Cardiel M, Ochagavía S, Rünkle I, Méndez JV, et al. Laparoscopic adrenalectomy vs. radiofrequency ablation for the treatment of primary aldosteronism. A single center retrospective cohort analysis adjusted with propensity score. Surg Endosc. 2022;36(3):1970-8.
Acknowledgements
We would like to express my gratitude to all those who facilitated with the writing of this manuscript. In addition, thank you to all peer reviewers for their opinions and suggestions.
Funding
This research was supported by the Natural Science Foundation of Gansu Province (21JR1RA130); Science and Technology Program of Lanzhou City (2021-1-77, 2023-2-111); the Innovation Fund of the Gansu Provincial Department of Education (2021B-047), and Cuiying Scientific and Technological Innovation Program of Lanzhou University Second Hospital (CY2020-BJ01).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Patient and public involvement
Patients and/or the public were not involved in any stage of the research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ma, R., Chen, G., Wei, T. et al. Efficacy and safety of radiofrequency ablation and laparoscopic adrenalectomy for primary aldosteronism: a meta‑analysis. Abdom Radiol (2024). https://doi.org/10.1007/s00261-024-04297-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00261-024-04297-6