Abstract
Purpose
To investigate various anatomical features of the prostate using preoperative MRI and patients’ clinical factors to identify predictors of successful Holmium:YAG laser enucleation of the prostate (HoLEP).
Methods
71 patients who had received HoLEP and undergone a 3.0-T prostate MRI scan within 6 months before surgery were retrospectively enrolled. MRI features (e.g., total prostate and transitional zone volume, peripheral zone thickness [PZT], BPH patterns, prostatic urethral angle, intravesical prostatic protrusion, etc.) and clinical data (e.g., age, body mass index, surgical technique, etc.) were analyzed using univariable and multivariable logistic regression to identify predictors of successful HoLEP. Successful HoLEP was defined as achieving the Trifecta, characterized by the contemporary absence of postoperative complications within 3 months, a 3-month postoperative maximum flow rate (Qmax) > 15 mL/s, and no urinary incontinence at 3 months postoperatively.
Results
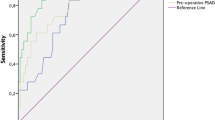
Trifecta achievement at 3 months post-surgery was observed in 37 (52%) patients. Patients with Trifecta achievement exhibited a lower preoperative IPSS-quality of life score (QoL) (4.1 vs. 4.5, P = 0.016) and a thinner preoperative peripheral zone thickness (PZT) on MRI (7.9 vs.10.3 mm, P < 0.001). In the multivariable regression analysis, a preoperative IPSS-QoL score < 5 (OR 3.98; 95% CI, 1.21–13.07; P = 0.017) and PZT < 9 mm (OR 11.51; 95% CI, 3.51–37.74; P < 0.001) were significant predictors of Trifecta achievement after HoLEP.
Conclusions
Alongside the preoperative QoL score, PZT measurement in prostate MRI can serve as an objective predictor of successful HoLEP. Our results underscore an additional utility of prostate MRI beyond its role in excluding concurrent prostate cancer.



Similar content being viewed by others
Code availability
The datasets and codes used in this study are available from the corresponding author on reasonable request.
References
Fraundorfer MR, Gilling PJ (1998) Holmium: YAG laser enucleation of the prostate combined with mechanical morcellation: preliminary results. Eur Urol. 33:69–72. https://doi.org/10.1159/000019535.
Gravas S, Gacci M, Gratzke C, Herrmann TRW, Karavitakis M, Kyriazis I, et al. (2023) Summary Paper on the 2023 European Association of Urology Guidelines on the Management of Non-neurogenic Male Lower Urinary Tract Symptoms. Eur Urol. 84:207–22. https://doi.org/10.1016/j.eururo.2023.04.008.
Zhong J, Feng Z, Peng Y, Liang H (2019) A Systematic Review and Meta-analysis of Efficacy and Safety Following Holmium Laser Enucleation of Prostate and Transurethral Resection of Prostate for Benign Prostatic Hyperplasia. Urology. 131:14–20. https://doi.org/10.1016/j.urology.2019.03.034.
Jeon BJ, Chung H, Bae JH, Jung H, Lee JG, Choi H (2019) Analysis of Present Status for Surgery of Benign Prostatic Hyperplasia in Korea Using Nationwide Healthcare System Data. Int Neurourol J. 23:22–9. https://doi.org/10.5213/inj.1836198.099.
Tsuboi I, Maruyama Y, Sadahira T, Ando N, Nishiyama Y, Araki M, et al. (2021) Efficacy of holmium laser enucleation in patients with a small (less than 30 mL) prostate volume. Investig Clin Urol. 62:298–304. https://doi.org/10.4111/icu.20200450.
Grosso AA, Di Maida F, Nardoni S, Salvi M, Giudici S, Lambertini L, et al. (2023) Patterns and Predictors of Optimal Surgical and Functional Outcomes after Holmium Laser Enucleation of the Prostate (HoLEP): Introducing the Concept of “Trifecta”. World J Mens Health. 41:603–11. https://doi.org/10.5534/wjmh.220042.
Ryoo HS, Suh YS, Kim TH, Sung HH, Jeong J, Lee KS (2015) Efficacy of Holmium Laser Enucleation of the Prostate Based on Patient Preoperative Characteristics. Int Neurourol J. 19:278–85. https://doi.org/10.5213/inj.2015.19.4.278.
Yu J, Jeong BC, Jeon SS, Lee SW, Lee KS (2021) Comparison of Efficacy of Different Surgical Techniques for Benign Prostatic Obstruction. Int Neurourol J. 25:252–62. https://doi.org/10.5213/inj.2040314.157.
Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, et al. (2015) EAU Guidelines on the Assessment of Non-neurogenic Male Lower Urinary Tract Symptoms including Benign Prostatic Obstruction. Eur Urol. 67:1099–109. https://doi.org/10.1016/j.eururo.2014.12.038.
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 240:205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Garvey B, Türkbey B, Truong H, Bernardo M, Periaswamy S, Choyke PL (2014) Clinical value of prostate segmentation and volume determination on MRI in benign prostatic hyperplasia. Diagn Interv Radiol. 20:229–33. https://doi.org/10.5152/dir.2014.13322.
Kaplan SA, Te AE, Pressler LB, Olsson CA (1995) Transition zone index as a method of assessing benign prostatic hyperplasia: correlation with symptoms, urine flow and detrusor pressure. J Urol. 154:1764–9.
Ku JH, Ko DW, Cho JY, Oh SJ (2010) Correlation between prostatic urethral angle and bladder outlet obstruction index in patients with lower urinary tract symptoms. Urology. 75:1467–71. https://doi.org/10.1016/j.urology.2009.08.049.
Nose H, Foo KT, Lim KB, Yokoyama T, Ozawa H, Kumon H (2005) Accuracy of two noninvasive methods of diagnosing bladder outlet obstruction using ultrasonography: intravesical prostatic protrusion and velocity-flow video urodynamics. Urology. 65:493–7. https://doi.org/10.1016/j.urology.2004.10.014.
Guneyli S, Ward E, Thomas S, Yousuf AN, Trilisky I, Peng Y, et al. (2016) Magnetic resonance imaging of benign prostatic hyperplasia. Diagn Interv Radiol. 22:215–9. https://doi.org/10.5152/dir.2015.15361.
Wasserman NF (2006) Benign prostatic hyperplasia: a review and ultrasound classification. Radiol Clin North Am. 44:689–710, viii. https://doi.org/10.1016/j.rcl.2006.07.005.
Boschheidgen M, Al-Monajjed R, Minko P, Jannusch K, Ullrich T, Radke KL, et al. (2023) Influence of benign prostatic hyperplasia patterns detected with MRI on the clinical outcome after prostatic artery embolization. CVIR Endovasc. 6:9. https://doi.org/10.1186/s42155-023-00357-y.
Little MW, Boardman P, Macdonald AC, Taylor N, Macpherson R, Crew J, et al. (2017) Adenomatous-Dominant Benign Prostatic Hyperplasia (AdBPH) as a Predictor for Clinical Success Following Prostate Artery Embolization: An Age-Matched Case-Control Study. Cardiovasc Intervent Radiol. 40:682–9. https://doi.org/10.1007/s00270-017-1602-8.
Kwon JK, Han JH, Choi HC, Kang DH, Lee JY, Kim JH, et al. (2016) Clinical significance of peripheral zone thickness in men with lower urinary tract symptoms/benign prostatic hyperplasia. BJU Int. 117:316–22. https://doi.org/10.1111/bju.13130.
Oh MM, Kim JW, Kim JJ, Moon du G (2012) Is there a correlation between the outcome of transurethral resection of prostate and preoperative degree of bladder outlet obstruction? Asian J Androl. 14:556–9. https://doi.org/10.1038/aja.2011.157.
Pyun JH, Kang SG, Kang SH, Cheon J, Kim JJ, Lee JG (2017) Efficacy of holmium laser enucleation of the prostate (HoLEP) in men with bladder outlet obstruction (BOO) and non-neurogenic bladder dysfunction. Kaohsiung J Med Sci. 33:458–63. https://doi.org/10.1016/j.kjms.2017.06.010.
Scoffone CM, Cracco CM (2016) The en-bloc no-touch holmium laser enucleation of the prostate (HoLEP) technique. World J Urol. 34:1175–81. https://doi.org/10.1007/s00345-015-1741-y.
Tuccio A, Grosso AA, Sessa F, Salvi M, Tellini R, Cocci A, et al. (2021) En-Bloc Holmium Laser Enucleation of the Prostate with Early Apical Release: Are We Ready for a New Paradigm? J Endourol. 35:1675–83. https://doi.org/10.1089/end.2020.1189.
de Figueiredo FCA, Cracco CM, de Marins RL, Scoffone CM (2020) Holmium laser enucleation of the prostate: Problem-based evolution of the technique. Andrologia. 52:e13582. https://doi.org/10.1111/and.13582.
Jaeger CD, Mitchell CR, Mynderse LA, Krambeck AE (2015) Holmium laser enucleation (HoLEP) and photoselective vaporisation of the prostate (PVP) for patients with benign prostatic hyperplasia (BPH) and chronic urinary retention. BJU Int. 115:295–9. https://doi.org/10.1111/bju.12674.
Watanabe H (1998) New concept of BPH: PCAR theory. Prostate. 37:116 – 25. https://doi.org/10.1002/(sici)1097-0045(19981001)37:2<116::aid-pros8>3.0.co;2-e.
Matsugasumi T, Fujihara A, Ushijima S, Kanazawa M, Yamada Y, Shiraishi T, et al. (2017) Morphometric analysis of prostate zonal anatomy using magnetic resonance imaging: impact on age-related changes in patients in Japan and the USA. BJU Int. 120:497–504. https://doi.org/10.1111/bju.13823.
Wang Q, Alshayyah R, He Y, Wen L, Yu Y, Yang B (2021) Is the Peripheral Zone Thickness an Indicator of a Learning Curve in Bipolar Transurethral Plasma Enucleation of the Prostate?-A Single Center Cohort Study. Front Surg. 8:795705. https://doi.org/10.3389/fsurg.2021.795705.
Tanaka Y, Masumori N, Itoh N, Furuya S, Ogura H, Tsukamoto T (2006) Is the short-term outcome of transurethral resection of the prostate affected by preoperative degree of bladder outlet obstruction, status of detrusor contractility or detrusor overactivity? Int J Urol. 13:1398–404. https://doi.org/10.1111/j.1442-2042.2006.01589.x.
Acknowledgements
none.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by J.H.P. and J.Y. The first draft of the manuscript was written by J.H.P., J.Y., and I.P. and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the institutional review board of Severance Hospital (IRB No. 2023-2003-001).
Consent to participate
Written informed consent was waived due to the retrospective nature of the study.
Consent for publication
This study does not involve images or materials that require the consent of a participant.
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
: Supplementary Table S1 and Supplementary Fig. S1–S4
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Park, J.H., Yoon, J., Park, I. et al. Peripheral zone thickness in preoperative MRI is predictive of Trifecta achievement after Holmium laser enucleation of the prostate (HoLEP).. Abdom Radiol (2024). https://doi.org/10.1007/s00261-024-04233-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00261-024-04233-8