Abstract
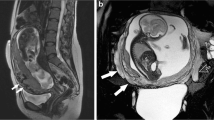
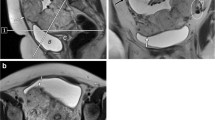
Placenta accreta spectrum disorder (PASD) encompasses various types of abnormal placentation in which chorionic villi directly adhere to or invade the myometrium. The incidence of PASD has dramatically risen in the US over the past 3 decades owing to the increased rates of patients undergoing cesarean sections. While PASD remains a significant cause of maternal morbidity and mortality, accurate prenatal identification and characterization of PASD is associated with improved outcomes. Although ultrasound is the first-line imaging modality in the evaluation of PASD, with MRI serving as an adjunct, computed tomography angiography (CTA) may also offer unique diagnostic advantages in cases of advanced PASD by providing superior visualization of placental and abdominopelvic vasculature and enabling the creation of comprehensive vascular maps to roadmap complex surgical interventions. This paper represents the first evaluation of CTA as a diagnostic tool and operative planning aid in this context. Appropriate indications and diagnostic advantages of CTA in this setting are reviewed, and key multimodal imaging features of normal and abnormal placentation are highlighted.
Graphical abstract










Similar content being viewed by others
References
Jauniaux E, Ayres-de-Campos D, Langhoff-Roos J, Fox KA, Collins S, FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. FIGO classification for the clinical diagnosis of placenta accreta spectrum disorders. Int J Gynaecol Obstet. 2019 Jul;146(1):20–4.
Cahill AG, Beigi R, Heine RP, Silver RM, Wax JR. Placenta Accreta Spectrum. American Journal of Obstetrics and Gynecology. 2018 Dec 1;219(6):B2–16.
Jauniaux E, Chantraine F, Silver RM, Langhoff-Roos J, FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. FIGO consensus guidelines on placenta accreta spectrum disorders: Epidemiology. Int J Gynaecol Obstet. 2018 Mar;140(3):265–73.
D’Antonio F, Iacovella C, Bhide A. Prenatal identification of invasive placentation using ultrasound: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2013 Nov;42(5):509–17.
Stirnemann JJ, Mousty E, Chalouhi G, Salomon LJ, Bernard JP, Ville Y. Screening for placenta accreta at 11-14 weeks of gestation. Am J Obstet Gynecol. 2011 Dec;205(6):547.e1-6.
Publications Committee, Society for Maternal-Fetal Medicine, Belfort MA. Placenta accreta. Am J Obstet Gynecol. 2010 Nov;203(5):430–9.
Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006 Jun;107(6):1226–32.
Thurn L, Lindqvist PG, Jakobsson M, Colmorn LB, Klungsoyr K, Bjarnadóttir RI, et al. Abnormally invasive placenta-prevalence, risk factors and antenatal suspicion: results from a large population-based pregnancy cohort study in the Nordic countries. BJOG. 2016 Jul;123(8):1348–55.
Clark SL, Koonings PP, Phelan JP. Placenta previa/accreta and prior cesarean section. Obstet Gynecol. 1985 Jul;66(1):89–92.
Vintzileos AM, Ananth CV, Smulian JC. Using ultrasound in the clinical management of placental implantation abnormalities. Am J Obstet Gynecol. 2015 Oct;213(4 Suppl):S70-77.
Jauniaux E, Bunce C, Grønbeck L, Langhoff-Roos J. Prevalence and main outcomes of placenta accreta spectrum: a systematic review and meta-analysis. Am J Obstet Gynecol. 2019 Sep;221(3):208–18.
Habek D, Becareviç R. Emergency peripartum hysterectomy in a tertiary obstetric center: 8-year evaluation. Fetal Diagn Ther. 2007;22(2):139–42.
Rahman J, Al-Ali M, Qutub HO, Al-Suleiman SS, Al-Jama FE, Rahman MS. Emergency obstetric hysterectomy in a university hospital: A 25-year review. J Obstet Gynaecol. 2008 Jan;28(1):69–72.
Glaze S, Ekwalanga P, Roberts G, Lange I, Birch C, Rosengarten A, et al. Peripartum hysterectomy: 1999 to 2006. Obstet Gynecol. 2008 Mar;111(3):732–8.
Zelop CM, Harlow BL, Frigoletto FD, Safon LE, Saltzman DH. Emergency peripartum hysterectomy. Am J Obstet Gynecol. 1993 May;168(5):1443–8.
Dashe JS, McIntire DD, Ramus RM, Santos-Ramos R, Twickler DM. Persistence of placenta previa according to gestational age at ultrasound detection. Obstet Gynecol. 2002 May;99(5 Pt 1):692–7.
Baughman WC, Corteville JE, Shah RR. Placenta accreta: spectrum of US and MR imaging findings. Radiographics. 2008;28(7):1905–16.
Poder L, Weinstein S, Maturen KE, Feldstein VA, Mackenzie DC, Oliver ER, et al. ACR Appropriateness Criteria® Placenta Accreta Spectrum Disorder. Journal of the American College of Radiology. 2020 May 1;17(5, Supplement):S207–14.
Maxwell C, Glanc P. Imaging and Obesity: A Perspective During Pregnancy. American Journal of Roentgenology. 2011 Feb;196(2):311–9.
Kilcoyne A, Shenoy-Bhangle AS, Roberts DJ, Sisodia RC, Gervais DA, Lee SI. MRI of Placenta Accreta, Placenta Increta, and Placenta Percreta: Pearls and Pitfalls. American Journal of Roentgenology. 2017 Jan;208(1):214–21.
Bhosale PR, Javitt MC, Atri M, Harris RD, Kang SK, Meyer BJ, et al. ACR Appropriateness Criteria® Acute Pelvic Pain in the Reproductive Age Group. Ultrasound Q. 2016 Jun;32(2):108–15.
Ghuman N, Fishman EK, Gomez E. 3D and cinematic rendering of abdominopelvic pathology in the peripartum period. Abdom Radiol. 2023 Apr 1;48(4):1383–94.
Rowe SP, Fishman EK. Fetal and placental anatomy visualized with cinematic rendering from volumetric CT data. Radiol Case Rep. 2018 Feb;13(1):281–3.
Wei SH, Helmy M, Cohen AJ. CT evaluation of placental abruption in pregnant trauma patients. Emerg Radiol. 2009 Sep;16(5):365–73.
Elsayes KM, Trout AT, Friedkin AM, Liu PS, Bude RO, Platt JF, et al. Imaging of the placenta: a multimodality pictorial review. Radiographics. 2009;29(5):1371–91.
McCollough CH, Schueler BA, Atwell TD, Braun NN, Regner DM, Brown DL, et al. Radiation exposure and pregnancy: when should we be concerned? Radiographics. 2007;27(4):909–17; discussion 917-918.
Raptis CA, Mellnick VM, Raptis DA, Kitchin D, Fowler KJ, Lubner M, et al. Imaging of trauma in the pregnant patient. Radiographics. 2014;34(3):748–63.
Sadro C, Bernstein MP, Kanal KM. Imaging of trauma: Part 2, Abdominal trauma and pregnancy--a radiologist’s guide to doing what is best for the mother and baby. AJR Am J Roentgenol. 2012 Dec;199(6):1207–19.
Angel E, Wellnitz CV, Goodsitt MM, Yaghmai N, DeMarco JJ, Cagnon CH, et al. Radiation dose to the fetus for pregnant patients undergoing multidetector CT imaging: Monte Carlo simulations estimating fetal dose for a range of gestational age and patient size. Radiology. 2008 Oct;249(1):220–7.
Hecht JL, Baergen R, Ernst LM, Katzman PJ, Jacques SM, Jauniaux E, et al. Classification and reporting guidelines for the pathology diagnosis of placenta accreta spectrum (PAS) disorders: recommendations from an expert panel. Mod Pathol. 2020 Dec;33(12):2382–96.
Vasbinder GBC, Nelemans PJ, Kessels AGH, Kroon AA, Maki JH, Leiner T, et al. Accuracy of Computed Tomographic Angiography and Magnetic Resonance Angiography for Diagnosing Renal Artery Stenosis. Ann Intern Med. 2004 Nov 2;141(9):674–82.
Bhatti AA, Chugtai A, Haslam P, Talbot D, Rix DA, Soomro NA. Prospective study comparing three-dimensional computed tomography and magnetic resonance imaging for evaluating the renal vascular anatomy in potential living renal donors. BJU Int. 2005 Nov;96(7):1105–8.
Leonhardt H, Thilander-Klang A, Båth J, Johannesson M, Kvarnström N, Dahm-Kähler P, et al. Imaging evaluation of uterine arteries in potential living donors for uterus transplantation: a comparative study of MRA, CTA, and DSA. Eur Radiol. 2022;32(4):2360–71.
Shih MCP, Hagspiel KD. CTA and MRA in Mesenteric Ischemia: Part 1, Role in Diagnosis and Differential Diagnosis. American Journal of Roentgenology. 2007 Feb;188(2):452–61.
Vertinsky AT, Schwartz NE, Fischbein NJ, Rosenberg J, Albers GW, Zaharchuk G. Comparison of Multidetector CT Angiography and MR Imaging of Cervical Artery Dissection. AJNR Am J Neuroradiol. 2008 Oct;29(9):1753–60.
Sentilhes L, Kayem G, Chandraharan E, Palacios-Jaraquemada J, Jauniaux E, FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. FIGO consensus guidelines on placenta accreta spectrum disorders: Conservative management. Int J Gynaecol Obstet. 2018 Mar;140(3):291–8.
Bird ST, Gelperin K, Sahin L, Bleich KB, Fazio-Eynullayeva E, Woods C, et al. First-Trimester Exposure to Gadolinium-based Contrast Agents: A Utilization Study of 4.6 Million U.S. Pregnancies. Radiology. 2019 Oct;293(1):193–200.
Oh KY, Roberts VHJ, Schabel MC, Grove KL, Woods M, Frias AE. Gadolinium Chelate Contrast Material in Pregnancy: Fetal Biodistribution in the Nonhuman Primate. Radiology. 2015 Jul;276(1):110–8.
Ray JG, Vermeulen MJ, Bharatha A, Montanera WJ, Park AL. Association Between MRI Exposure During Pregnancy and Fetal and Childhood Outcomes. JAMA. 2016 Sep 6;316(9):952–61.
McDonald RJ, McDonald JS, Kallmes DF, Jentoft ME, Murray DL, Thielen KR, et al. Intracranial Gadolinium Deposition after Contrast-enhanced MR Imaging. Radiology. 2015 Jun;275(3):772–82.
Prola-Netto J, Woods M, Roberts VHJ, Sullivan EL, Miller CA, Frias AE, et al. Gadolinium Chelate Safety in Pregnancy: Barely Detectable Gadolinium Levels in the Juvenile Nonhuman Primate after in Utero Exposure. Radiology. 2018 Jan;286(1):122–8.
Committee Opinion No. 723: Guidelines for Diagnostic Imaging During Pregnancy and Lactation. Obstetrics & Gynecology. 2017 Oct;130(4):e210.
Perelli F, Turrini I, Giorgi MG, Renda I, Vidiri A, Straface G, et al. Contrast Agents during Pregnancy: Pros and Cons When Really Needed. Int J Environ Res Public Health. 2022 Dec 12;19(24):16699.
Jose O, Stoeckl EM, Miles RC, Mango VL, Reid NJ, Wagner ASB, et al. The Impact of Extreme Neighborhood Socioeconomic Deprivation on Access to American College of Radiology–accredited Advanced Imaging Facilities. Radiology. 2023 May;307(3):e222182.
Arditi B, Purisch SE, Friedman AM, Gyamfi-Bannerman C. Maternal Perioperative Morbidity and Race in Women with Placenta Accreta [28C]. Obstetrics & Gynecology. 2019 May;133:39S.
Vestal NL, Sangara RN, Mandelbaum RS, Matsuzaki S, McCarthy LE, Matsushima K, et al. Racial and ethnic disparity in characteristics and outcomes of women with placenta accreta spectrum: a comparative study. Reprod Sci. 2022 Jul 1;29(7):1988–2000.
Sensakovic WF, Royall I, Hough M, Potrebko P, Grekoski V, Vicenti R. Fetal Dosimetry at CT: A Primer. RadioGraphics. 2020 Jul;40(4):1061–70.
Funding
No funding was required for this study
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no disclosures
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gomez, E.N., Ahmed, T.M., Macura, K. et al. CT angiography for characterization of advanced placenta accreta spectrum: indications, risks, and benefits. Abdom Radiol 49, 842–854 (2024). https://doi.org/10.1007/s00261-023-04105-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-023-04105-7