Abstract
Background
Stereotactic body radiotherapy (SBRT) is a local treatment option for hepatocellular carcinoma (HCC). SBRT-induced focal reactions on the liver parenchyma have not been thoroughly evaluated using quantitative magnetic resonance imaging (MRI).
Purpose
To quantitatively evaluate liver parenchymal changes caused by SBRT for HCC using magnetic resonance elastography (MRE) and diffusion-weighted imaging (DWI).
Method
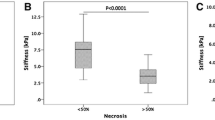
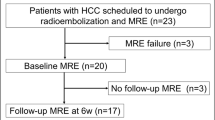
We retrospectively evaluated 22 adult patients who received SBRT for HCC and 27 who received locoregional therapy other than SBRT (controls). Liver stiffness by MRE and apparent diffusion coefficient (ADC) values by DWI of the liver parenchyma were measured before and after SBRT. Regions of interest (ROIs) were drawn on the two areas of radiation dose distribution levels, > 30 Gy and ≤ 30 Gy; a ROI was drawn in the control group. The two indices were compared before and after SBRT using a Wilcoxon matched-pairs signed-rank test.
Results
Liver stiffness and ADC values were significantly increased after SBRT in the dose areas of > 30 Gy compared with those before SBRT (4.05 vs 4.85 kPa; p < 0.05 in liver stiffness, and 1.10 vs 1.40 ×10−3 s/mm2; p < 0.05 in ADC values). In the dose area of ≦ 30 Gy, liver stiffness showed a significant increase in one reader (p = 0.033) but not in another reader (p = 0.085); ADC value showed no significant difference before and after SBRT as per both readers (p > 0.05). The control group demonstrated no significant differences before and after treatment (p > 0.05).
Conclusion
MRE and DWI can be used to detect SBRT-induced liver parenchymal changes.




Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
D.I. Tsilimigras, H. Aziz, T.M. Pawlik (2022) Critical Analysis of the Updated Barcelona Clinic Liver Cancer (BCLC) Group Guidelines. Ann Surg Oncol:29 7231-7234.https://doi.org/10.1245/s10434-022-12242-4
A. Takeda, N. Sanuki, Y. Tsurugai, S. Iwabuchi, K. Matsunaga, H. Ebinuma, K. Imajo, Y. Aoki, H. Saito, E. Kunieda (2016) Phase 2 study of stereotactic body radiotherapy and optional transarterial chemoembolization for solitary hepatocellular carcinoma not amenable to resection and radiofrequency ablation. Cancer:122 2041-9.https://doi.org/10.1002/cncr.30008
F. Wang, K. Numata, A. Takeda, K. Ogushi, H. Fukuda, K. Hara, M. Chuma, T. Eriguchi, Y. Tsurugai, S. Maeda (2021) Safety and efficacy study: Short-term application of radiofrequency ablation and stereotactic body radiotherapy for Barcelona Clinical Liver Cancer stage 0-B1 hepatocellular carcinoma. PLoS One:16 e0245076.https://doi.org/10.1371/journal.pone.0245076
T.S. Lawrence, J.M. Robertson, M.S. Anscher, R.L. Jirtle, W.D. Ensminger, L.F. Fajardo (1995) Hepatic toxicity resulting from cancer treatment. Int J Radiat Oncol Biol Phys:31 1237-48.https://doi.org/10.1016/0360-3016(94)00418-K
C. Guha, B.D. Kavanagh (2011) Hepatic radiation toxicity: avoidance and amelioration. Semin Radiat Oncol:21 256-63.https://doi.org/10.1016/j.semradonc.2011.05.003
A. Mendez Romero, W. Wunderink, S.M. Hussain, J.A. De Pooter, B.J. Heijmen, P.C. Nowak, J.J. Nuyttens, R.P. Brandwijk, C. Verhoef, J.N. Ijzermans, P.C. Levendag (2006) Stereotactic body radiation therapy for primary and metastatic liver tumors: A single institution phase i-ii study. Acta Oncol:45 831-7.https://doi.org/10.1080/02841860600897934
A. Moore, M. Cohen-Naftaly, A. Tobar, Y. Kundel, O. Benjaminov, M. Braun, A. Issachar, E. Mor, M. Sarfaty, D. Bragilovski, R.B. Hur, N. Gordon, S.M. Stemmer, A.M. Allen (2017) Stereotactic body radiation therapy (SBRT) for definitive treatment and as a bridge to liver transplantation in early stage inoperable Hepatocellular carcinoma. Radiat Oncol:12 163.https://doi.org/10.1186/s13014-017-0899-4
K.K. Herfarth, H. Hof, M.L. Bahner, F. Lohr, A. Hoss, G. van Kaick, M. Wannenmacher, J. Debus (2003) Assessment of focal liver reaction by multiphasic CT after stereotactic single-dose radiotherapy of liver tumors. Int J Radiat Oncol Biol Phys:57 444-51.https://doi.org/10.1016/s0360-3016(03)00586-8
N. Sanuki, A. Takeda, Y. Oku, T. Eriguchi, S. Nishimura, Y. Aoki, T. Mizuno, S. Iwabuchi, E. Kunieda (2014) Threshold doses for focal liver reaction after stereotactic ablative body radiation therapy for small hepatocellular carcinoma depend on liver function: evaluation on magnetic resonance imaging with Gd-EOB-DTPA. Int J Radiat Oncol Biol Phys:88 306-11.https://doi.org/10.1016/j.ijrobp.2013.10.045
S.H. Jung, J.I. Yu, H.C. Park, D.H. Lim, Y. Han (2016) A feasibility study evaluating the relationship between dose and focal liver reaction in stereotactic ablative radiotherapy for liver cancer based on intensity change of Gd-EOB-DTPA-enhanced magnetic resonance images. Radiat Oncol J:34 64-75.https://doi.org/10.3857/roj.2016.34.1.64
M.J. Park, S.Y. Kim, S.M. Yoon, J.H. Kim, S.H. Park, S.S. Lee, Y. Lee, M.G. Lee (2014) Stereotactic body radiotherapy-induced arterial hypervascularity of non-tumorous hepatic parenchyma in patients with hepatocellular carcinoma: potential pitfalls in tumor response evaluation on multiphase computed tomography. PLoS One:9 e90327.https://doi.org/10.1371/journal.pone.0090327
S. Takamatsu, K. Kozaka, S. Kobayashi, N. Yoneda, K. Yoshida, D. Inoue, A. Kitao, T. Ogi, T. Minami, W. Kouda, T. Kumano, N. Fuwa, O. Matsui, T. Gabata (2018) Pathology and images of radiation-induced hepatitis: a review article. Jpn J Radiol:36 241-256.https://doi.org/10.1007/s11604-018-0728-1
M.M. Haddad, K.W. Merrell, C.L. Hallemeier, G.B. Johnson, T. Mounajjed, K.R. Olivier, J.L. Fidler, S.K. Venkatesh (2016) Stereotactic body radiation therapy of liver tumors: post-treatment appearances and evaluation of treatment response: a pictorial review. Abdom Radiol (NY):41 2061-77.https://doi.org/10.1007/s00261-016-0768-x
P.J. Navin, M.C. Olson, M. Mendiratta-Lala, C.L. Hallemeier, M.S. Torbenson, S.K. Venkatesh (2022) Imaging Features in the Liver after Stereotactic Body Radiation Therapy. Radiographics 220084.https://doi.org/10.1148/rg.220084
M. Yin, K.J. Glaser, A. Manduca, T. Mounajjed, H. Malhi, D.A. Simonetto, R. Wang, L. Yang, S.A. Mao, J.M. Glorioso, F.M. Elgilani, C.J. Ward, P.C. Harris, S.L. Nyberg, V.H. Shah, R.L. Ehman (2017) Distinguishing between Hepatic Inflammation and Fibrosis with MR Elastography. Radiology:284 694-705.https://doi.org/10.1148/radiol.2017160622
J.J. Yoo, Y.S. Seo, Y.S. Kim, S.W. Jeong, J.Y. Jang, S.J. Suh, H.J. Yim, K.T. Suk, D.J. Kim, K.H. Han, S.U. Kim, B. Lee, S.G. Kim (2019) The Influence of Histologic Inflammation on the Improvement of Liver Stiffness Values Over 1 and 3 Years. J Clin Med:8.https://doi.org/10.3390/jcm8122065
B. Taouli, M. Chouli, A.J. Martin, A. Qayyum, F.V. Coakley, V. Vilgrain (2008) Chronic hepatitis: role of diffusion-weighted imaging and diffusion tensor imaging for the diagnosis of liver fibrosis and inflammation. J Magn Reson Imaging:28 89-95.https://doi.org/10.1002/jmri.21227
M. Franca, L. Marti-Bonmati, A. Alberich-Bayarri, P. Oliveira, S. Guimaraes, J. Oliveira, J. Amorim, J.S. Gonzalez, J.R. Vizcaino, H.P. Miranda (2017) Evaluation of fibrosis and inflammation in diffuse liver diseases using intravoxel incoherent motion diffusion-weighted MR imaging. Abdom Radiol (NY):42 468-477.https://doi.org/10.1007/s00261-016-0899-0
S. Ichikawa, U. Motosugi, M. Oguri, H. Onishi (2017) Magnetic resonance elastography for prediction of radiation-induced liver disease after stereotactic body radiation therapy. Hepatology:66 664-665.https://doi.org/10.1002/hep.29128
C.C. Olsen, J. Welsh, B.D. Kavanagh, W. Franklin, M. McCarter, H.R. Cardenes, L.E. Gaspar, T.E. Schefter (2009) Microscopic and macroscopic tumor and parenchymal effects of liver stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys:73 1414-24.https://doi.org/10.1016/j.ijrobp.2008.07.032
F.F. Guglielmo, S.K. Venkatesh, D.G. Mitchell (2019) Liver MR Elastography Technique and Image Interpretation: Pearls and Pitfalls. Radiographics:39 1983-2002.https://doi.org/10.1148/rg.2019190034
J.R. Landis, G.G. Koch (1977) The measurement of observer agreement for categorical data. Biometrics:33 159-74
C.W. Song, E. Glatstein, L.B. Marks, B. Emami, J. Grimm, P.W. Sperduto, M.S. Kim, S. Hui, K.E. Dusenbery, L.C. Cho (2021) Biological Principles of Stereotactic Body Radiation Therapy (SBRT) and Stereotactic Radiation Surgery (SRS): Indirect Cell Death. Int J Radiat Oncol Biol Phys:110 21-34.https://doi.org/10.1016/j.ijrobp.2019.02.047
T. Kimura, S. Takahashi, I. Takahashi, I. Nishibuchi, Y. Doi, M. Kenjo, Y. Murakami, Y. Honda, H. Aikata, K. Chayama, Y. Nagata (2015) The Time Course of Dynamic Computed Tomographic Appearance of Radiation Injury to the Cirrhotic Liver Following Stereotactic Body Radiation Therapy for Hepatocellular Carcinoma. PLoS One:10 e0125231.https://doi.org/10.1371/journal.pone.0125231
C.L. Eccles, E.A. Haider, M.A. Haider, S. Fung, G. Lockwood, L.A. Dawson (2009) Change in diffusion weighted MRI during liver cancer radiotherapy: preliminary observations. Acta Oncol:48 1034-43.https://doi.org/10.1080/02841860903099972
M. Okada, K. Numata, H. Nihonmatsu, K. Tomita, A. Takeda, K. Tago, T. Hyodo, T. Eriguchi, M. Nakano (2022) Pathological Appearance of Focal Liver Reactions after Radiotherapy for Hepatocellular Carcinoma. Diagnostics (Basel):12.https://doi.org/10.3390/diagnostics12051072
T.R. Chapman, A.R. Kumarapeli, M.J. Nyflot, S.R. Bowen, R.S. Yeung, H.J. Vesselle, M.M. Yeh, S. Apisarnthanarax (2015) Functional imaging of radiation liver injury in a liver metastasis patient: imaging and pathologic correlation. J Gastrointest Oncol:6 E44-7.https://doi.org/10.3978/j.issn.2078-6891.2015.002
M. Sorensen, M.M. Fode, J.B. Petersen, M.I. Holt, M. Hoyer (2021) Effect of stereotactic body radiotherapy on regional metabolic liver function investigated in patients by dynamic [(18)F]FDGal PET/CT. Radiat Oncol:16 192.https://doi.org/10.1186/s13014-021-01909-z
M. Kong, S.E. Hong (2015) Optimal follow-up duration for evaluating objective response to radiotherapy in patients with hepatocellular carcinoma: a retrospective study. Chin J Cancer:34 79-85.https://doi.org/10.5732/cjc.014.10136
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
There is no financial support related to this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Since this study was an observational study based on medical records, information on the implementation of the study including the purpose was posted on the website of the Ethics Committee of University of Yamanashi to guarantee the opportunity for the research subjects to refuse.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Omiya, Y., Morisaka, H., Matsuda, M. et al. Liver parenchymal changes detected by MR elastography and diffusion-weighted imaging after stereotactic body radiotherapy for hepatocellular carcinoma. Abdom Radiol 48, 3353–3361 (2023). https://doi.org/10.1007/s00261-023-03995-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-023-03995-x