Abstract
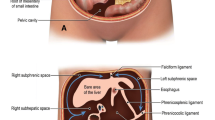
This manuscript focuses on a review of the normal and abnormal sonographic appearance of the surgically created pouch as part of an article series on the topic. It includes information regarding sonographic technique, normal anatomy, and commonly encounter diseases and complications.







Similar content being viewed by others
References
C. Lu, C. Merrill, A. Medellin, K. Novak, and S. R. Wilson, “Bowel Ultrasound State of the Art: Grayscale and Doppler Ultrasound, Contrast Enhancement, and Elastography in Crohn Disease,” J. Ultrasound Med., vol. 38, no. 2, 2019, https://doi.org/10.1002/jum.14920.
F. Castiglione et al., “Noninvasive Diagnosis of Small Bowel Crohn’s Disease,” Inflamm. Bowel Dis., vol. 19, no. 5, pp. 991–998, Apr. 2013, doi: https://doi.org/10.1097/MIB.0b013e3182802b87.
M. L. W. Ziech et al., “Accuracy of abdominal ultrasound and MRI for detection of Crohn disease and ulcerative colitis in children,” Pediatr. Radiol., 2014, doi: https://doi.org/10.1007/s00247-014-3010-4.
D. Roccarina et al., “Diagnosis of bowel diseases: The role of imaging and ultrasonography,” World J Gastroenterol, vol. 19, no. 1914, pp. 2144–2153, 2013, doi: https://doi.org/10.3748/wjg.v19.i14.2144.
A. E. Bohte, J. R. Van Werven, S. Bipat, and J. Stoker, “The diagnostic accuracy of US, CT, MRI and 1H-MRS for the evaluation of hepatic steatosis compared with liver biopsy: A meta-analysis,” Eur. Radiol., vol. 21, no. 1, pp. 87–97, 2011, doi: https://doi.org/10.1007/s00330-010-1905-5.
M. Fraquelli et al., “Role of US in detection of Crohn disease: meta-analysis.,” Radiology, vol. 236, no. 1, pp. 95–101, 2005, doi: https://doi.org/10.1148/radiol.2361040799.
S. A. Taylor et al., “Diagnostic accuracy of magnetic resonance enterography and small bowel ultrasound for the extent and activity of newly diagnosed and relapsed Crohn’s disease (METRIC): a multicentre trial,” Lancet Gastroenterol. Hepatol., vol. 3, no. 8, pp. 548–558, Aug. 2018, doi: https://doi.org/10.1016/S2468-1253(18)30161-4.
D. Cosgrove et al., “EFSUMB Guidelines and Recommendations on the clinical use of ultrasound elastographypart 2: Clinical applications,” Ultraschall in der Medizin, vol. 34, no. 3. 2013. https://doi.org/10.1055/s-0033-1335375.
C. Frias-Gomes, J. Torres, and C. Palmela, “Intestinal Ultrasound in Inflammatory Bowel Disease: A Valuable and Increasingly Important Tool,” GE Portuguese Journal of Gastroenterology, vol. 29, no. 4. S. Karger AG, pp. 223–239, Jul. 23, 2022. https://doi.org/10.1159/000520212.
O. M. Nardone et al., “The Impact of Intestinal Ultrasound on the Management of Inflammatory Bowel Disease: From Established Facts Toward New Horizons,” Front. Med., vol. 9, no. May, pp. 1–9, 2022, doi: https://doi.org/10.3389/fmed.2022.898092.
J. M. Barlow, A. L. Lightner, S. P. Sheedy, D. H. Bruining, C. O. Menias, and J. G. Fletcher, “J Pouch : Imaging Findings , Sur- gical Variations , Natural History , and Common Complications,” 2018.
Z. S. Ardalan et al., “Accuracy of Gastrointestinal Ultrasound and Calprotectin in the Assessment of Inflammation and its Location in Patients with an Ileoanal Pouch,” J. Crohn’s Colitis, vol. 16, no. 1, pp. 79–90, 2022, doi: https://doi.org/10.1093/ecco-jcc/jjab125.
K. L. Novak et al., “A Simple Ultrasound Score for the Accurate Detection of Inflammatory Activity in Crohnʼs Disease,” Inflamm. Bowel Dis., vol. 0, no. 0, p. 1, 2017, doi: https://doi.org/10.1097/MIB.0000000000001174.
A. Medellin, C. Merrill, and S. R. Wilson, “Role of contrast-enhanced ultrasound in evaluation of the bowel,” Abdom. Radiol., 2017, doi: https://doi.org/10.1007/s00261-017-1399-6.
A. Medellin-Kowalewski, R. Wilkens, A. Wilson, J. Ruan, and S. R. Wilson, “Quantitative contrast-enhanced ultrasound parameters in Crohn disease: Their role in disease activity determination with ultrasound,” Am. J. Roentgenol., vol. 206, no. 1, pp. 64–73, 2016, doi: https://doi.org/10.2214/AJR.15.14506.
T. Ripollés, M. J. Martínez, J. M. Paredes, E. Blanc, L. Flors, and F. Delgado, “Crohn Disease: Correlation of Findings at Contrast-enhanced US with Severity at Endoscopy,” Radiology, vol. 253, no. 1, pp. 241–248, 2009, doi: https://doi.org/10.1148/radiol.2531082269.
B. H. Drews et al., “Comparison of sonographically measured bowel wall vascularity, histology, and disease activity in Crohn’s disease.,” Eur. Radiol., vol. 19, no. 6, pp. 1379–86, Jun. 2009, doi: https://doi.org/10.1007/s00330-008-1290-5.
A. Albuquerque and E. Pereira, “Current applications of transperineal ultrasound in gastroenterology,” World J. Radiol., vol. 8, no. 4, p. 370, 2016, doi: https://doi.org/10.4329/wjr.v8.i4.370.
K. P. Dhamanaskar, W. Thurston, and S. R. Wilson, “Transvaginal sonography as an adjunct to endorectal sonography in the staging of rectal cancer in women,” Am. J. Roentgenol., vol. 187, no. 1, pp. 90–98, 2006, doi: https://doi.org/10.2214/AJR.04.1363.
M. J. Kim, “Transrectal ultrasonography of anorectal diseases: Advantages and disadvantages,” Ultrasonography, vol. 34, no. 1, pp. 19–31, Nov. 2014, doi: https://doi.org/10.14366/usg.14051.
Y. Sun, L.-G. Cui, J.-B. Liu, J.-R. Wang, H. Ping, and Z.-W. Chen, “Utility of 360° Real-time Endoanal Sonography for Evaluation of Perianal Fistulas,” J. Ultrasound Med., vol. 37, no. 1, pp. 93–98, Jan. 2018, doi: https://doi.org/10.1002/jum.14307.
E. Panel et al., “APPROPRIATE USE CRITERIA ACR Appropriateness Criteria â Anorectal Disease,” J. Am. Coll. Radiol., vol. 18, no. 11, pp. S268–S282, 2021, doi: https://doi.org/10.1016/j.jacr.2021.08.009.
F. Cao et al., “Correlation between Disease Activity and Endorectal Ultrasound Findings of Chronic Radiation Proctitis.,” Ultrasound Med. Biol., vol. 43, no. 10, pp. 2182–2191, Oct. 2017, doi: https://doi.org/10.1016/j.ultrasmedbio.2017.06.025.
A. Sharma, P. Yadav, M. Sahu, and A. Verma, “Current imaging techniques for evaluation of fistula in ano: a review,” Egypt. J. Radiol. Nucl. Med., vol. 51, no. 1, 2020, https://doi.org/10.1186/s43055-020-00252-9.
C. Lu, X. Gui, W. Chen, T. Fung, K. Novak, and S. R. Wilson, “Ultrasound Shear Wave Elastography and Contrast Enhancement: Effective Biomarkers in Crohn’s Disease Strictures.,” Inflamm. Bowel Dis., vol. 0, no. 0, pp. 1–10, 2017, https://doi.org/10.1097/MIB.0000000000001020.
D. Ślósarz, E. Poniewierka, K. Neubauer, and R. Kempiński, “Ultrasound elastography in the assessment of the intestinal changes in inflammatory bowel disease—systematic review,” Journal of Clinical Medicine, vol. 10, no. 18. MDPI, Sep. 01, 2021. https://doi.org/10.3390/jcm10184044.
P. P. Tekkis, “A systematic review and meta-analysis comparing adverse events and functional outcomes of different pouch designs after restorative proctocolectomy,” pp. 664–675, 2018, https://doi.org/10.1111/codi.14104.
K. P. Quinn, A. L. Lightner, W. A. Faubion, and L. E. Raffals, “A Comprehensive Approach to Pouch Disorders,” vol. 25, no. 3, pp. 460–471, 2019, https://doi.org/10.1093/ibd/izy267.
M. Prudhomme, R. R. Dozois, G. Godlewski, S. Mathison, and P. Fabbro-Peray, “Anal canal strictures after ileal pouch-anal anastomosis.,” Dis. Colon Rectum, vol. 46, no. 1, pp. 20–3, Jan. 2003, doi: https://doi.org/10.1007/s10350-004-6491-7.
B. Shen et al., “Endoscopic and histologic evaluation together with symptom assessment are required to diagnose pouchitis,” Gastroenterology, vol. 121, no. 2, pp. 261–267, 2001, doi: https://doi.org/10.1053/gast.2001.26290.
F. Khan and B. Shen, “Complications Related to J-Pouch Surgery,” vol. 14, no. 10, pp. 571–576, 2018.
A. L. Lightner, J. H. Pemberton, and E. J. Loftus, “Crohn’s Disease of the Ileoanal Pouch.,” Inflamm. Bowel Dis., vol. 22, no. 6, pp. 1502–8, Jun. 2016, doi: https://doi.org/10.1097/MIB.0000000000000712.
A. L. Lightner, J. G. Fletcher, J. H. Pemberton, K. L. Mathis, L. E. Raffals, and T. Smyrk, “Crohn’s Disease of the Pouch: A True Diagnosis or an Oversubscribed Diagnosis of Exclusion?,” Dis. Colon Rectum, vol. 60, no. 11, pp. 1201–1208, Nov. 2017, doi: https://doi.org/10.1097/DCR.0000000000000918.
E. L. Barnes, B. Kochar, and H. R. Jessup, “The Incidence and Definition of Crohn ’ s Disease of the Pouch : A Systematic Review and Meta-analysis,” vol. 25, no. 9, pp. 1474–1480, 2019, https://doi.org/10.1093/ibd/izz005.
B. Shen et al., “Diagnosis and classification of ileal pouch disorders: consensus guidelines from the International Ileal Pouch Consortium,” The Lancet Gastroenterology and Hepatology, vol. 6, no. 10. Elsevier Ltd, pp. 826–849, Oct. 01, 2021. https://doi.org/10.1016/S2468-1253(21)00101-1.
F. Berton, G. Gola, and S. R. Wilson, “Perspective on the role of transrectal and transvaginal sonography of tumors of the rectum and anal canal,” Am. J. Roentgenol., vol. 190, no. 6, pp. 1495–1504, 2008, doi: https://doi.org/10.2214/AJR.07.3188.
Author information
Authors and Affiliations
Contributions
SW and AM (authors) contributed to the manuscript, material selection and preparation. The first draft of the manuscript was written by AM and SW commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Alexandra Medellin have received book royalties from Elsevier. Stephanie R. Wilson: Advisory Board, Definity. Lantheus Medical Imaging Speakers Bureau, Philips. Equipment support: Philips, Siemens, Samsung.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Medellin, A., Wilson, S. Sonographic evaluation of a surgically created pouch. Abdom Radiol 48, 2986–2999 (2023). https://doi.org/10.1007/s00261-023-03941-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-023-03941-x