Abstract
Purpose
Hepatobiliary phase (HBP) hypointense nodules without arterial phase hyperenhancement (APHE) on gadoxetic acid-enhanced MRI (GA-MRI) may be nonmalignant cirrhosis-associated nodules or hepatocellular carcinomas (HCCs). We aimed to characterize HBP hypointense nodules without APHE on GA-MRI by performing contrast-enhanced ultrasound using perfluorobutane (PFB-CEUS).
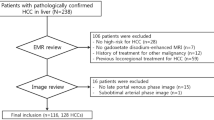
Methods
In this prospective, single-center study, participants at high-risk of HCC having HBP hypointense nodules without APHE at GA-MRI were enrolled. All participants underwent PFB-CEUS; if APHE and late, mild washout or washout in the Kupffer phase were present, the diagnosis of HCC was established according to the v2022 Korean guidelines. The reference standard consisted of histopathology or imaging. The sensitivity, specificity, and positive/negative predictive values of PFB-CEUS for detecting HCC were calculated. Associations between clinical/imaging features and the diagnosis of HCC were evaluated with logistic regression analyses.
Results
In total, 67 participants (age, 67.0 years ± 8.4; 56 men) with 67 HBP hypointense nodules without APHE (median size, 1.5 cm [range, 1.0–3.0 cm]) were included. The prevalence of HCC was 11.9% (8/67). The sensitivity, specificity, and positive and negative predictive values of PFB-CEUS for detecting HCC were 12.5%(1/8), 96.6%(57/59), 33.3%(1/3) and 89.1%(57/64), respectively. Mild-moderate T2 hyperintensity on GA-MRI (odds ratio, 5.756; P = 0.042) and washout in the Kupffer phase on PFB-CEUS (odds ratio, 5.828; P = 0.048) were independently associated with HCC.
Conclusion
Among HBP hypointense nodules without APHE, PFB-CEUS was specific for detecting HCC, which had a low prevalence. Mild-moderate T2 hyperintensity on GA-MRI and washout in the Kupffer phase on PFB-CEUS may be useful to detect HCC in those nodules.
Graphical abstract




Similar content being viewed by others
References
Duncan JK, Ma N, Vreugdenburg TD, Cameron AL, Maddern G (2017) Gadoxetic acid-enhanced MRI for the characterization of hepatocellular carcinoma: A systematic review and meta-analysis. J Magn Reson Imaging 45:281-290. https://doi.org/10.1002/jmri.25345
Zech CJ, Ba-Ssalamah A, Berg T et al (2020) Consensus report from the 8th International Forum for Liver Magnetic Resonance Imaging. Eur Radiol 30:370-382. https://doi.org/10.1007/s00330-019-06369-4
Choi JY, Lee JM, Sirlin CB (2014) CT and MR imaging diagnosis and staging of hepatocellular carcinoma: part I. Development, growth, and spread: key pathologic and imaging aspects. Radiology 272:635-654. https://doi.org/10.1148/radiol.14132361
Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, Roberts LR, Heimbach JK (2018) Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 68:723-750. https://doi.org/10.1002/hep.29913
European Association for the Study of the Liver. Electronic address eee, European Association for the Study of the L (2018) EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol 69:182-236. https://doi.org/10.1016/j.jhep.2018.03.019
Korean Liver Cancer A, National Cancer Center K (2022) 2022 KLCA-NCC Korea Practice Guidelines for the Management of Hepatocellular Carcinoma. Korean J Radiol 23:1126-1240. https://doi.org/10.3348/kjr.2022.0822
Joo I, Kim SY, Kang TW et al (2020) Radiologic-pathologic correlation of hepatobiliary phase hypointense nodules without arterial phase hyperenhancement at gadoxetic acid–enhanced MRI: A multicenter study. Radiology 296:335–345
Yoon JH, Lee JM, Yang HK, Lee KB, Jang J-J, Han JK, Choi BI (2014) Non-hypervascular hypointense nodules≥ 1 cm on the hepatobiliary phase of gadoxetic acid-enhanced magnetic resonance imaging in cirrhotic livers. Digestive Diseases 32:678–689
Nakamura S, Nouso K, Kobayashi Y et al (2013) The diagnosis of hypovascular hepatic lesions showing hypo-intensity in the hepatobiliary phase of Gd-EOB-DTPA-enhanced MR imaging in high-risk patients for hepatocellular carcinoma. Acta medica Okayama 67:239–244
Davenport MS, Caoili EM, Kaza RK, Hussain HK (2014) Matched within-patient cohort study of transient arterial phase respiratory motion-related artifact in MR imaging of the liver: gadoxetate disodium versus gadobenate dimeglumine. Radiology 272:123-131. https://doi.org/10.1148/radiol.14132269
Pietryga JA, Burke LM, Marin D, Jaffe TA, Bashir MR (2014) Respiratory motion artifact affecting hepatic arterial phase imaging with gadoxetate disodium: examination recovery with a multiple arterial phase acquisition. Radiology 271:426-434. https://doi.org/10.1148/radiol.13131988
Yoon JH, Lee JM, Yu MH, Kim EJ, Han JK (2016) Triple arterial phase MR imaging with gadoxetic acid using a combination of contrast enhanced time robust angiography, keyhole, and viewsharing techniques and two-dimensional parallel imaging in comparison with conventional single arterial phase. Korean Journal of Radiology 17:522–532
Seale MK, Catalano OA, Saini S, Hahn PF, Sahani DV (2009) Hepatobiliary-specific MR contrast agents: role in imaging the liver and biliary tree. Radiographics 29:1725-1748. https://doi.org/10.1148/rg.296095515
Durot I, Wilson SR, Willmann JK (2018) Contrast-enhanced ultrasound of malignant liver lesions. Abdom Radiol (NY) 43:819-847. https://doi.org/10.1007/s00261-017-1360-8
Wilson SR, Kim TK, Jang H-J, Burns PN (2007) Enhancement patterns of focal liver masses: discordance between contrast-enhanced sonography and contrast-enhanced CT and MRI. American Journal of Roentgenology 189:W7-W12
Yanagisawa K, Moriyasu F, Miyahara T, Yuki M, Iijima H (2007) Phagocytosis of ultrasound contrast agent microbubbles by Kupffer cells. Ultrasound Med Biol 33:318-325. https://doi.org/10.1016/j.ultrasmedbio.2006.08.008
Kim BR, Lee JM, Lee DH, Yoon JH, Hur BY, Suh KS, Yi N-J, Lee KB, Han JKJR (2017) Diagnostic performance of gadoxetic acid–enhanced liver MR imaging versus multidetector CT in the detection of dysplastic nodules and early hepatocellular carcinoma. 285:134–146
Joo I, Lee JM, Koh YH, Choi SH, Lee S, Chung JWJKJoR (2023) 2022 Korean Liver Cancer Association-National Cancer Center Korea Practice Guidelines for Imaging Diagnosis of Hepatocellular Carcinoma: What’s New? 24:1–5
Chernyak V, Fowler KJ, Kamaya A et al (2018) Liver Imaging Reporting and Data System (LI-RADS) version 2018: imaging of hepatocellular carcinoma in at-risk patients. Radiology 289:816–830
Yoon JH, Chang W, Lee ES, Lee SM, Lee JMJIr (2020) Double low-dose dual-energy liver CT in patients at high-risk of HCC: a prospective, randomized, single-center study. 55:340–348
Lee DH, Lee JM, Lee JY et al (2015) Non-hypervascular hepatobiliary phase hypointense nodules on gadoxetic acid-enhanced MRI: risk of HCC recurrence after radiofrequency ablation. Journal of Hepatology 62:1122–1130
Lee DH, Lee JM, Yu MH et al (2019) Non-hypervascular hepatobiliary phase hypointense nodules on gadoxetic acid-enhanced MR can help determine the treatment method for HCC. European Radiology 29:3122–3131
Kim T-H, Woo S, Han S, Suh CH, Lee DH, Lee JM (2020) Hepatobiliary phase hypointense nodule without arterial phase hyperenhancement: are they at risk of HCC recurrence after ablation or surgery? A systematic review and meta-analysis. European Radiology 30:1624–1633
Sugimoto K, Moriyasu F, Saito K, Taira J, Saguchi T, Yoshimura N, Oshiro H, Imai Y, Shiraishi J (2012) Comparison of Kupffer-phase Sonazoid-enhanced sonography and hepatobiliary-phase gadoxetic acid-enhanced magnetic resonance imaging of hepatocellular carcinoma and correlation with histologic grading. J Ultrasound Med 31:529-538. https://doi.org/10.7863/jum.2012.31.4.529
Yang WY, Park HS, Kim YJ, Yu MH, Jung SI, Jeon HJ (2017) Visibility of focal liver lesions: Comparison between kupffer phase of CEUS with sonazoid and hepatobiliary phase of gadoxetic acid–enhanced MRI. Journal of Clinical Ultrasound 45:542–550
Kawada N, Ohkawa K, Tanaka S et al (2010) Improved diagnosis of well‐differentiated hepatocellular carcinoma with gadolinium ethoxybenzyl diethylene triamine pentaacetic acid‐enhanced magnetic resonance imaging and Sonazoid contrast‐enhanced ultrasonography. Hepatology Research 40:930–936
Ohama H, Imai Y, Nakashima O et al (2014) Images of Sonazoid-enhanced ultrasonography in multistep hepatocarcinogenesis: comparison with Gd-EOB-DTPA-enhanced MRI. 49:1081–1093
Kojiro M, Roskams T. Early hepatocellular carcinoma and dysplastic nodules. Seminars in liver disease: Copyright© 2005 by Thieme Medical Publishers, Inc., 333 Seventh Avenue, New …; 2005. p. 133–142
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This work was financially supported by GE Healthcare. However, the data were completely under the control of the authors. Otherwise, the authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bae, J.S., Lee, J.Y., Suh, KS. et al. Characterization of hepatobiliary phase hypointense nodules without arterial phase hyperenhancement on gadoxetic acid-enhanced MRI via contrast-enhanced ultrasound using perfluorobutane. Abdom Radiol 48, 2321–2330 (2023). https://doi.org/10.1007/s00261-023-03901-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-023-03901-5