Abstract
Purpose
In this study, the effects of hypertonic saline and ethanol as a single intracystic agents in the percutaneous treatment of liver hydatid cysts were compared.
Methods
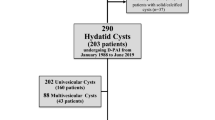
The 50 patients were separated into two groups as those administered 30% hypertonic saline alone as the intracystic agent in percutaneous treatment (33 patients, 52 cysts), and those administered 96% ethanol alone (17 patients, 26 cysts). Both groups were compared in terms of percentage of cyst volume reduction, complications, and treatment success.
Results
The follow-up period was median 17.0 months (11.0–20.0) in the ethanol group and 17.0 (14.0–22.0) in the hypertonic saline group (p = 0.269). Complications were observed in 5 (19.2%) cysts applied with ethanol as the intracystic agent and in 7 (13.5%) of the cysts where hypertonic saline was used (p = 0.521). Clinical success was evaluated as 100% in both groups. The percentage of cyst volume reduction according to the initial volume was determined as mean 75.6 ± 20.43 (28.19–98.13) in the ethanol group cysts and as 68.2 ± 16.45 (26.39–97.48) in the hypertonic saline group (p = 0.427).
Conclusion
The results of this study demonstrated similar efficacy of hypertonic saline and ethanol in the percutaneous treatment of CE1 and CE3A liver hydatid cysts. These results suggest that the use of hypertonic saline as a single intracystic agent in the percutaneous treatment of CE1 and CE3A liver hydatid cysts provides sufficient efficacy of treatment and cyst volume reduction. Nevertheless, there is a need for further prospective, randomized studies to support these findings.




Similar content being viewed by others
References
Deplazes P, Rinaldi, L, Alvarez Rojas C. A. et al (2017) Global Distribution of Alveolar and Cystic Echinococcosis. Advances in parasitology 95, 315–493. https://doi.org/10.1016/bs.apar.2016.11.001
Tamarozzi F, Akhan O, Cretu CM, et al (2018). Prevalence of abdominal cystic echinococcosis in rural Bulgaria, Romania, and Turkey: a cross-sectional, ultrasound-based, population study from the HERACLES project. Lancet Infect Dis 18:769–778. https://doi.org/10.1016/S1473-3099(18)30221-4
Odev K, Paksoy Y, Arslan A, et al (2000) Sonographically guided percutaneous treatment of hepatic hydatid cysts: long-term results. J Clin Ultrasound 28:469-478. https://doi.org/10.1002/1097-0096(200011/12)28:9<469::aid-jcu4>3.0.co;2-f
Bakdik S, Arslan S, Oncu F, Tolu I, Eryilmaz MA (2018) Percutaneous treatment of hepatic cystic echinococcosis: the success of alcohol as a single endocavitary agent in PAIR, catheterization, and modified catheterization techniques. Radiol Med 123:153-160. https://doi.org/10.1007/s11547-017-0820-0
Paksoy Y, Odev K, Sahin M, Arslan A, Koç O (2005) Percutaneous treatment of liver hydatid cysts: comparison of direct injection of albendazole and hypertonic saline solution. AJR Am J Roentgenol 185:727-734. https://doi.org/10.2214/ajr.185.3.01850727
Akhan O, Erdoğan E, Ciftci TT, Unal E, Karaağaoğlu E, Akinci D (2020) Comparison of the Long-Term Results of Puncture, Aspiration, Injection and Re-aspiration (PAIR) and Catheterization Techniques for the Percutaneous Treatment of CE1 and CE3a Liver Hydatid Cysts: A Prospective Randomized Trial. Cardiovasc Intervent Radiol 43:1034-1040. https://doi.org/10.1007/s00270-020-02477-7
Yagci G, Ustunsoz B, Kaymakcioglu N, et al (2005) Results of surgical, laparoscopic, and percutaneous treatment for hydatid disease of the liver: 10 years experience with 355 patients. World J Surg 29:1670-1679. https://doi.org/10.1007/s00268-005-0058-1
Gupta N, Javed A, Puri S, Jain S, Singh S, Agarwal AK (2011) Hepatic hydatid: PAIR, drain or resect? J Gastrointest Surg 15:1829-1836. https://doi.org/10.1007/s11605-011-1649-9
Kabaalioglu A, Ceken K, Alimoglu E, Apaydin A (2006) Percutaneous imaging-guided treatment of hydatid liver cysts: do long-term results make it a first choice? Eur J Radiol 59:65–73. https://doi.org/10.1016/j.ejrad.2006.01.014
Firpo G, Vola A, Lissandrin R, Tamarozzi F, Brunetti E (2017) Preliminary Evaluation of Percutaneous Treatment of Echinococcal Cysts without Injection of Scolicidal Agent. Am J Trop Med Hyg 97:1818-1826. https://doi.org/10.4269/ajtmh.17-0468
Acunas B, Rozanes I, Celik L, Minareci O, Acunas G, Alper A, Ariogul O, Gökmen E (1992) Purely cystic hydatid disease of the liver: treatment with percutaneous aspiration and injection of hypertonic saline. Radiology 182:541-543. https://doi.org/10.1148/radiology.182.2.1732977
Erzurumlu K, Ozdemir M, Mihmanli M, Cevikbaş U (1995) The effect of intraoperative mebendazole-albendazole applications on the hepatobiliary system. Eur Surg Res 27(5):340-345. https://doi.org/10.1159/000129418
Yetim I, Erzurumlu K, Hokelek M, et al (2005) Results of alcohol and albendazole injections in hepatic hydatidosis: experimental study. J Gastroenterol Hepatol20:1442-1447. https://doi.org/10.1111/j.1440-1746.2005.03843.x
Houry S, Languille O, Huguier M, Benhamou JP, Belghiti J, Msika S (1990) Sclerosing cholangitis induced by formaldehyde solution injected into the biliary tree of rats. Arch Surg 125:1059-1061. https://doi.org/10.1001/archsurg.1990.01410200123020
Hosseini SV, Al-Qanbar MH, Khazraei H, Khodaei S, Mokhtari M, Iranpour P (2020) Evaluation the Effects of Eucalyptus Essential Oil and Hypertonic Saline as Scolicidal Agents in Induction of Sclerosing Cholangitis in Rabbits. Adv Biomed Res 2020;9:9. https://doi.org/10.4103/abr.abr_210_19
Ramia JM, Figueras J, De la Plaza R, García-Parreño J (2012) Cysto-biliary communication in liver hydatidosis. Langenbecks Arch Surg 397:881-887. https://doi.org/10.1007/s00423-012-0926-8
Kayaalp C, Bzeizi K, Demirbag AE, Akoglu M (2002) Biliary complications after hydatid liver surgery: incidence and risk factors. J Gastrointest Surg 6:706-712. https://doi.org/10.1016/s1091-255x(02)00046-x
Demircan O, Baymus M, Seydaoglu G, Akinoglu A, Sakman G (2006) Occult cystobiliary communication presenting as postoperative biliary leakage after hydatid liver surgery: are there significant preoperative clinical predictors? Can J Surg 49:177-184.
Zeybek N, Dede H, Balci D, Coskun AK, Ozerhan IH, Peker S, Peker Y (2013) Biliary fistula after treatment for hydatid disease of the liver: when to intervene. World J Gastroenterol 19:355-361. https://doi.org/10.3748/wjg.v19.i3.355
Acknowledgements
Not applicable.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: AK, Methodology: AK, MU, Formal analysis and investigation: AK, MU Writing—original draft preparation: AK, MU Writing—review and editing: AK Supervision: AK, MU.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by Hatay Mustafa Kemal University Ethics Committee (Date: 17/06/2021. No:17).
Informed consent
For this type of study, informed consent is not required.
Consent for publication
For this type of study, consent for publication is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kayalı, A., Uğur, M. Comparison of ethanol and hypertonic saline as a single ıntracystic agent in the percutaneous treatment of liver hydatid cysts. Abdom Radiol 48, 1148–1153 (2023). https://doi.org/10.1007/s00261-022-03795-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-022-03795-9