Abstract
Purpose
Treatment for gastroesophageal adenocarcinomas can result in significant morbidity and mortality. The purpose of this study is to supplement methods for choosing treatment strategy by assessing the relationship between CT-derived body composition, patient, and tumor features, and clinical outcomes in this population.
Methods
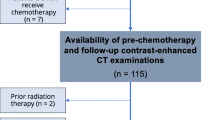
Patients with neoadjuvant treatment, biopsy-proven gastroesophageal adenocarcinoma, and initial staging CTs were retrospectively identified from institutional clinic encounters between 2000 and 2019. Details about patient, disease, treatment, and outcomes (including therapy tolerance and survival) were extracted from electronic medical records. A deep learning semantic segmentation algorithm was utilized to measure cross-sectional areas of skeletal muscle (SM), visceral fat (VF), and subcutaneous fat (SF) at the L3 vertebra level on staging CTs. Univariate and multivariate analyses were performed to assess the relationships between predictors and outcomes.
Results
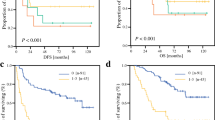
142 patients were evaluated. Median survival was 52 months. Univariate and multivariate analysis showed significant associations between treatment tolerance and SM and VF area, SM to fat and VF to SF ratios, and skeletal muscle index (SMI) (p = 0.004–0.04). Increased survival was associated with increased body mass index (BMI) (p = 0.01) and increased SMI (p = 0.004). A multivariate Cox model consisting of BMI, SMI, age, gender, and stage demonstrated that patients in the high-risk group had significantly lower survival (HR = 1.77, 95% CI = 1.13–2.78, p = 0.008).
Conclusion
CT-based measures of body composition in patients with gastroesophageal adenocarcinoma may be independent predictors of treatment complications and survival and can supplement methods for assessing functional status during treatment planning.
Graphical abstract




Similar content being viewed by others
References
Howlander N, Noone A, Krapcho M, Miller D, Brest A, Yu M, et al. SEER cancer statistics review, 1975–2017. National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2017/, based on November 2019 SEER data submission, posted to the SEER web site, April 2020.
Thrift AP. The epidemic of oesophageal carcinoma: where are we now? Cancer Epidemiol. 2016;41:88-95. doi: https://doi.org/10.1016/j.canep.2016.01.013.
Dicken BJ, Bigam DL, Cass C, Mackey JR, Joy AA, Hamilton SM. Gastric adenocarcinoma: review and considerations for future directions. Ann Surg. 2005;241(1):27. doi: https://doi.org/10.1097/01.sla.0000149300.28588.23.
Shi A, Liao Z, Allen PK, Ho L, Murphy MB, Maru DM, et al. Long-term survival and toxicity outcomes of intensity modulated radiation therapy for the treatment of esophageal cancer: a large single-institutional cohort study. Adv Radiat Oncol. 2017;2(3):316-24. doi: https://doi.org/10.1016/j.adro.2017.04.002.
Sastre J, García-Saenz JA, Díaz-Rubio E. Chemotherapy for gastric cancer. World J Gastroenterol. 2006;12(2):204. doi: https://doi.org/10.3748/wjg.v12.i2.204.
Riccardi D, Allen K. Nutritional management of patients with esophageal and esophagogastric junction cancer. Cancer Control. 1999;6(1):64-72. doi: https://doi.org/10.1177/107327489900600106.
Miller AL, Min LC, Diehl KM, Cron DC, Chan C-L, Sheetz KH, et al. Analytic morphomics corresponds to functional status in older patients. J Surg Res. 2014;192(1):19-26. doi: https://doi.org/10.1016/j.jss.2014.06.011.
Kuwada K, Kuroda S, Kikuchi S, Yoshida R, Nishizaki M, Kagawa S, et al. Sarcopenia and comorbidity in gastric cancer surgery as a useful combined factor to predict eventual death from other causes. Ann Surg Oncol. 2018;25(5):1160-6. doi: https://doi.org/10.1245/s10434-018-6354-4.
Hay CM, Donovan HS, Campbell GB, Taylor SE, Wang L, Courtney-Brooks M. Chemotherapy in older adult gynecologic oncology patients: Can a phenotypic frailty score predict tolerance? Gynecol Oncol. 2019;152(2):304-9. doi: https://doi.org/10.1016/j.ygyno.2018.11.031.
Heus C, Smorenburg A, Stoker J, Rutten MJ, Amant FCH, van Lonkhuijzen L. Visceral obesity and muscle mass determined by CT scan and surgical outcome in patients with advanced ovarian cancer. A retrospective cohort study. Gynecol Oncol. 2021;160(1):187-92. doi: https://doi.org/10.1016/j.ygyno.2020.10.015.
Lafata KJ, Wang Y, Konkel B, Yin FF, Bashir MR. Radiomics: a primer on high-throughput image phenotyping. Abdom Radiol. 2021:1–17. doi: https://doi.org/10.1007/s00261-021-03254-x.
Kok DE, Winkels RM, van Herpen CM, Kampman E. Toxicity-induced modification of treatment: what is in a name? Eur J Cancer. 2018;104:145-50. doi: https://doi.org/10.1016/j.ejca.2018.09.018.
van den Berg M, Kok DE, Posthuma L, Kamps L, Kelfkens CS, Buist N, et al. Body composition is associated with risk of toxicity-induced modifications of treatment in women with stage I-IIIB breast cancer receiving chemotherapy. Breast Cancer Res Treat. 2019;173(2):475-81. doi: https://doi.org/10.1007/s10549-018-5014-5.
Isensee F, Jaeger PF, Kohl SAA, Petersen J, Maier-Hein KH. nnU-Net: a self-configuring method for deep learning-based biomedical image segmentation. Nat Methods. 2021;18(2):203-11. doi: https://doi.org/10.1038/s41592-020-01008-z.
Botev A, Lever G, Barber D. Nesterov's accelerated gradient and momentum as approximations to regularised update descent. 2017 International Joint Conference on Neural Networks (IJCNN). 2017:1899-903. doi: https://doi.org/10.1109/IJCNN.2017.7966082.
Chen L-C, Papandreou G, Kokkinos I, Murphy K, Yuille AL. Deeplab: Semantic image segmentation with deep convolutional nets, atrous convolution, and fully connected crfs. IEEE Trans Pattern Anal Mach Intell. 2017;40(4):834-48. doi: https://doi.org/10.1109/TPAMI.2017.2699184.
Kuwada K, Kuroda S, Kikuchi S, Yoshida R, Nishizaki M, Kagawa S, et al. Clinical impact of sarcopenia on gastric cancer. Anticancer Res. 2019;39(5):2241-9. doi: https://doi.org/10.21873/anticanres.13340.
Buettner S, Wagner D, Kim Y, Margonis GA, Makary MA, Wilson A, et al. Inclusion of sarcopenia outperforms the modified frailty index in predicting 1-Year mortality among 1,326 patients undergoing gastrointestinal surgery for a malignant indication. J Am Coll Surg. 2016;222(4):397–407 e2. doi: https://doi.org/10.1016/j.jamcollsurg.2015.12.020.
Ma BW, Chen XY, Fan SD, Zhang FM, Huang DD, Li B, et al. Impact of sarcopenia on clinical outcomes after radical gastrectomy for patients without nutritional risk. Nutrition. 2019;61:61-6. doi: https://doi.org/10.1016/j.nut.2018.10.025.
Lee JS, Kim YS, Kim EY, Jin W. Prognostic significance of CT-determined sarcopenia in patients with advanced gastric cancer. PLoS One. 2018;13(8):e0202700. doi: https://doi.org/10.1371/journal.pone.0202700.
Boshier PR, Heneghan R, Markar SR, Baracos VE, Low DE. Assessment of body composition and sarcopenia in patients with esophageal cancer: a systematic review and meta-analysis. Dis Esophagus. 2018;31(8). doi: https://doi.org/10.1093/dote/doy047.
Wang SL, Ma LL, Chen XY, Zhou DL, Li B, Huang DD, et al. Impact of visceral fat on surgical complications and long-term survival of patients with gastric cancer after radical gastrectomy. Eur J Clin Nutr. 2018;72(3):436-45. doi: https://doi.org/10.1038/s41430-017-0032-7.
Gu L, Zhang Y, Hong J, Xu B, Yang L, Yan K, et al. Prognostic value of pretreatment overweight/obesity and adipose tissue distribution in resectable gastric cancer: a retrospective cohort study. Front Oncol. 2021;11:680190. doi: https://doi.org/10.3389/fonc.2021.680190.
Doyle SL, Mongan AM, Donohoe CL, Pidgeon GP, Sherlock M, Reynolds JV, et al. Impact of visceral obesity and metabolic syndrome on the postoperative immune, inflammatory, and endocrine response following surgery for esophageal adenocarcinoma. Dis Esophagus. 2017;30(6):1-11. doi: https://doi.org/10.1093/dote/dox008.
Feng F, Zheng G, Guo X, Liu Z, Xu G, Wang F, et al. Impact of body mass index on surgical outcomes of gastric cancer. BMC Cancer. 2018;18(1):151. doi: https://doi.org/10.1186/s12885-018-4063-9.
Zhang SS, Yang H, Luo KJ, Huang QY, Chen JY, Yang F, et al. The impact of body mass index on complication and survival in resected oesophageal cancer: a clinical-based cohort and meta-analysis. Br J Cancer. 2013;109(11):2894-903. doi: https://doi.org/10.1038/bjc.2013.666.
Kim J, Hurria A. Determining chemotherapy tolerance in older patients with cancer. J Natl Compr Canc Netw. 2013;11(12):1494-502. doi: https://doi.org/10.6004/jnccn.2013.0176.
Bredella MA. Sex differences in body composition. Adv Exp Med Biol. 2017;1043:9-27. doi: https://doi.org/10.1007/978-3-319-70178-3_2.
Derstine BA, Holcombe SA, Ross BE, Wang NC, Su GL, Wang SC. Optimal body size adjustment of L3 CT skeletal muscle area for sarcopenia assessment. Sci Rep. 2021;11(1):279. doi: https://doi.org/10.1038/s41598-020-79471-z.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declares that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
DeFreitas, M.R., Toronka, A., Nedrud, M.A. et al. CT-derived body composition measurements as predictors for neoadjuvant treatment tolerance and survival in gastroesophageal adenocarcinoma. Abdom Radiol 48, 211–219 (2023). https://doi.org/10.1007/s00261-022-03695-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-022-03695-y