Abstract
Purpose
To determine how clinical and imaging features affect the positive predictive values (PPV) of US-3 observations.
Methods
In this retrospective study, 10,546 adult patients who were high risk for hepatocellular carcinoma (HCC) from 2017 to 2021 underwent ultrasound screening/surveillance. Of these, 225 adult patients (100 women, 125 men) with an US-3 observation underwent diagnostic characterization with multiphasic CT (93; 41%), MRI (130; 58%), or contrast-enhanced ultrasound (2; 1%). US-3 observations included focal observations ≥ 10 mm in 216 patients and new venous thrombi in 9 patients. PPV with 95% confidence intervals were calculated using diagnostic characterization as the reference standard. Multivariable analysis of clinical and imaging features was performed to determine the strongest associations with cancer.
Results
Overall PPV for an US-3 observation was 33% (27–39%) for at least intermediate probability of cancer (≥ LR-3) and 15% (10–20%) for at least probable cancer (≥ LR-4). At multivariable analysis, cirrhosis had the strongest effect size for at least probable cancer (p < 0.001; odds ratio OR 20.4), followed by observation size (p < 0.001; OR 2.65) and age (p = 0.004; OR 1.05). Alpha-fetoprotein, visualization score, and observation echogenicity were not statistically significant associations. Modality (MRI versus CT) did not affect PPV. Due to the large effect of cirrhosis, PPV was then stratified by the presence (n = 116; 52%) or absence (n = 109; 48%) of cirrhosis. For at least probable cancer (≥ LR-4), PPV increased from 4% (0–7%; non-cirrhotic) to 26% (18–34%; p < 0.001; cirrhosis).
Conclusion
Cirrhosis most strongly affects PPV of US-3 observations for at least probable cancer at diagnostic characterization among high-risk patients, increasing to 1 in 4 among cirrhotic patients from 1 in 25 among non-cirrhotic patients.
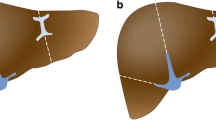
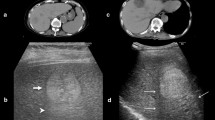
Graphical Abstract





Similar content being viewed by others
References
Marrero JA, Kulik LM, Sirlin CB et al (2018) Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 68(2):723–750.
American College of Radiology Committee on LI-RADS. US LI-RADS v2017 Core. Available at https://www.acr.org/-/media/ACR/Files/RADS/LI-RADS/LI-RADS-US-Algorithm-Portrait-2017.pdf. Accessed on June 5, 2021.
Rodgers SK, Fetzer DT, Gabriel H et al (2019) Role of US LI-RADS in the LI-RADS algorithm. RadioGraphics 39:690–708.
Morgan TA, Maturen KE, Dahiya N, Sun MRM, Kamaya A; American College of Radiology Ultrasound Liver Imaging and Reporting Data System (US LI-RADS) Working Group (2018) US LI-RADS: Ultrasound Liver Imaging Reporting and Data System for screening and surveillance of hepatocellular carcinoma. Abdom Radiol (NY) 43:41–55.
Sevco TJ, Masch WR, Maturen KE, Mendiratta-Lala M, Wasnik AP, Millet JD (2021) Ultrasound (US) LI-RADS: Outcomes of Category US-3 Observations. AJR Am J Roentgenol; 217(3): 644–650.
American College of Radiology Committee on LI-RADS. LI-RADS v2018 CT/MRI Core. https://www.acr.org/-/media/ACR/Files/RADS/LI-RADS/LI-RADS-2018-Core.pdf. Accessed on January 5, 2021.
American College of Radiology Committee on LI-RADS. CEUS LI-RADS v2017 Core. https://www.acr.org/-/media/ACR/Files/RADS/LI-RADS/CEUS-LI-RADS-2017-Core.pdf. Accessed on June 5, 2021.
Moon AM, Singal AG, Tapper EB (2020) Global Epidemiology of Chronic Liver Disease. Contemporary Epidemiology of Chronic Liver Disease and Cirrhosis. Clin Gastroenterol Hepatol 18(12): 2650–2666.
Bosch FX, Ribes J, Diaz M, Cleries R (2004) Primary liver cancer: worldwide incidence and trends. Gastroenterology 127: S5–S16.
Millet JD, Kamaya A, Choi HH, et al (2019) ACR Ultrasound Liver Reporting and Data System: multicenter assessment of clinical performance at one year. J Am Coll Radiol 16:1656–1662.
Son JH, Choi SH, Kim SY, et al (2019) Validation of US Liver Imaging Reporting and Data System version 2017 in patients at high risk for hepatocellular carcinoma. Radiology 292:390–397.
Chiang CJ, Yang YW, You SL, Lai MS, Chen CJ (2013) Thirty-year outcomes of the national hepatitis B immunization program in Taiwan. JAMA 2013; 310:974–976.
Brechot C. Pathogenesis of hepatitis B virus—related hepatocellular carcinoma: old and new paradigms (2004) Gastroenterology 127(5): S56–S61.
Fattovich G, Stroffolini T, Zagni I, Donato F (2004) Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology 127(5 Suppl 1):S35–S50.
Frenette CT, Isaacson AJ, Bargellini I, Saab S, Singal AG (2019) A Practical Guideline for Hepatocellular Carcinoma Screening in Patients at Risk. Mayo Clin Proc Innov Qual Outcomes 3(3):302–310.
Kokudo N, Takemura N, Hasegawa K et al (2019) Clinical practice guidelines for hepatocellular carcinoma: The Japan Society of Hepatology 2017 (4th JSH-HCC guidelines) 2019 update. Hepatology Research 49:1109–1113.
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma (2018) J Hepatol 69(1):182–236.
Omata M, Cheng AL, Kokudo N et al (2017) Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int 11(4):317–370.
Kudo M, Kawamura Y, Hasegawa K et al (2021) Management of Hepatocellular Carcinoma in Japan: JSH Consensus Statements and Recommendations 2021 Update. Liver Cancer 10(3):181–223.
Asrani SK, Ghabril MS, Kuo A (2022) Quality measures in HCC care by the Practice Metrics Committee of the American Association for the Study of Liver Diseases. Hepatology 75(5):1289–1299.
Heimbach JK, Kulik LM, Finn RS et al (2017) AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 67:358–380.
Roberts LR, Sirlin CB, Zaiem F et al. Imaging for the diagnosis of hepatocellular carcinoma: A systematic review and meta-analysis. Hepatology 2018; 67:401–421.
Hertzberg BS, Middleton WD (2016) Ultrasound: The Requisites, 3rd Edition. Elsevier. Amsterdam, Netherlands.
Shao YY, Wang SY, Lin SM (2021) Diagnosis Group; Systemic Therapy Group. Management consensus guideline for hepatocellular carcinoma: 2020 update on surveillance, diagnosis, and systemic treatment by the Taiwan Liver Cancer Association and the Gastroenterological Society of Taiwan. J Formos Med Assoc 120(4):1051–1060.
Fetzer DT, Browning T, Xi Y, Yokoo T, Singal AG (2022) Associations of Ultrasound LI-RADS Visualization Score With Examination, Sonographer, and Radiologist Factors: Retrospective Assessment in Over 10,000 Examinations. AJR Am J Roentgenol 218(6):1010–1020.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Aya Kamaya receives book royalties from Elsevier and has a grant from Canon Medical Systems. Justin Tse has a pending grant from Bayer Healthcare. The remaining authors do not have any disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tse, J.R., Shen, L., Tiyarattanachai, T. et al. Positive predictive value of LI-RADS US-3 observations: multivariable analysis of clinical and imaging features. Abdom Radiol 48, 271–281 (2023). https://doi.org/10.1007/s00261-022-03681-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-022-03681-4