Abstract
Purpose
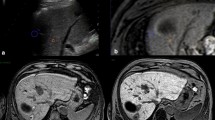
Ultrasound (US)-guided thermal ablation (TA) may cause major biliary complications, particularly in patients with malignant liver tumors (MLTs) adjacent to the bile ducts. Fusion imaging (FI), is postulated to reduce complication rate; however, there is a lack of clinical data to support this theory. Thus, the aim of our study was to evaluate the safety and efficacy of FI for TA of MLTs proximal to the bile ducts.
Methods
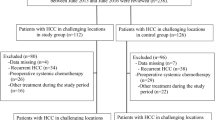
A retrospective single-center review was conducted on a total of 289 patients with 316 MLTs adjacent to the bile ducts. The patients were divided into two groups based on whether FI was used in the ablation procedures. The choice of the FI-assisted procedure always depends on different operation periods and whether registrations will succeed. The baseline demographics and outcomes of these patients were compared. The efficacy was determined at the 1-month follow-up using contrast-enhanced computed tomography/magnetic resonance. Biliary complications and local tumor progression were subsequently followed-up every 3–6 months. The last follow-up visit was before August 30, 2019.
Results
Among the included tumors, the incidence rate of major biliary complications after ablation in the FI group was 1.6%, which was significantly lower than that in the non-FI group (7.9%, p = 0.005). There was no significant difference in the efficacy rates of the techniques [99.5% (185/186) versus 98.4% (123/125), p = 0.56] or local progression rates [3.8% (7/185) versus 5.7% (7/123), p = 0.61] between the FI and non-FI groups.
Conclusion
FI for US-guided TA could be a noninvasive means to decrease major biliary complications.
Trial registration number and date of registration: retrospectively registered.
Graphical abstract




Similar content being viewed by others
Data availability
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
References
Omata M, Cheng AL, Kokudo N, Kudo M, Lee JM, Jia J et al (2017) Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int 11(4):317-370. https://https://doi.org/10.1007/s12072-017-9799-9
Galle PR, Forner A, Llovet JM, Mazzaferro V, Piscaglia F, Raoul JL (2018) EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol 69(1):182-236. https://https://doi.org/10.1016/j.jhep.2018.03.019
Fonseca AZ, Santin S, Gomes LGL, Waisberg J, Ribeiro JMAF (2014) Complications of radiofrequency ablation of hepatic tumors:Frequency and risk factors. World journal of hepatology 6(3):107-113. https://https://doi.org/10.4254/wjh.v6.i3.107
Lin MX, Ye JY, Tian WS, Xu M, Zhuang BW, Lu MD et al (2017) Risk Factors for Bile Duct Injury After Percutaneous Thermal Ablation of Malignant Liver Tumors: A Retrospective Case-Control Study. Dig Dis Sci 62(4):1086-1094. https://https://doi.org/10.1007/s10620-016-4312-1
Liu J, Wu Y, Xu E, Huang Q, Ye H, Tan L et al (2019) Risk factors of intrahepatic biloma and secondary infection after thermal ablation for malignant hepatic tumors. Int J Hyperthermia 36(1):980-985. https://https://doi.org/10.1080/02656736.2019.1660422
Felker ER, Lee-Felker SA, Ajwichai K, Tan N, Lu DS, Durazo FA et al (2015) Intraductal Cooling via a Nasobiliary Tube During Radiofrequency Ablation of Central Liver Tumors Reduces Biliary Injuries. American journal of roentgenology (1976) 204(6):1329.
Imai Y, Hirooka M, Ochi H, Koizumi Y, Ohno Y, Watanabe T et al (2015) A case of hepatocellular carcinoma treated by radiofrequency ablation confirming the adjacent major bile duct under hybrid contrast mode through a biliary drainage catheter. Clin J Gastroenterol 8(5):318-322. https://https://doi.org/10.1007/s12328-015-0599-2
Huang H, Liang P, Yu XL, Cheng ZG, Han ZY, Yu J et al (2015) Safety assessment and therapeutic efficacy of percutaneous microwave ablation therapy combined with percutaneous ethanol injection for hepatocellular carcinoma adjacent to the gallbladder. Int J Hyperthermia 31(1):40-47. https://https://doi.org/10.3109/02656736.2014.999017
Li M, Yu X, Liang P, Dong B, Liu F (2015) Ultrasound-guided percutaneous microwave ablation for hepatic malignancy adjacent to the gallbladder. Int J Hyperthermia 31(6):579-587. https://https://doi.org/10.3109/02656736.2015.1014869
Jiang K, Zhang WZ, Liu Y, Su M, Zhao XQ, Dong JH et al (2014) "One-off" complete radiofrequency ablation for hepatocellular carcinoma in a "high-risk location" adjacent to the major bile duct and hepatic blood vessel. Cell Biochem Biophys 69(3):605-617. https://https://doi.org/10.1007/s12013-014-9840-8
Yu M, Li S (2022) Irreversible electroporation for liver cancer ablation: A meta analysis. Eur J Surg Oncol 48(6):1321-1330. https://https://doi.org/10.1016/j.ejso.2021.12.015
Thamtorawat S, Patanawanitkul R, Rojwatcharapibarn S, Chaiyasoot W, Tongdee T, Yodying J et al (2022) Biliary complications and efficacy after ablation of peribiliary tumors using irreversible electroporation (IRE) or radiofrequency ablation (RFA). Int J Hyperthermia 39(1):751-757. https://https://doi.org/10.1080/02656736.2022.2079733
Carriero S, Della Pepa G, Monfardini L, Vitale R, Rossi D, Masperi A et al (2021) Role of Fusion Imaging in Image-Guided Thermal Ablations. Diagnostics 11(3):549. https://https://doi.org/10.3390/diagnostics11030549
Lee DH, Lee JM (2018) Recent Advances in the Image-Guided Tumor Ablation of Liver Malignancies: Radiofrequency Ablation with Multiple Electrodes, Real-Time Multimodality Fusion Imaging, and New Energy Sources. Korean J Radiol 19(4):545. https://https://doi.org/10.3348/kjr.2018.19.4.545
Kang TW, Rhim H (2015) Recent Advances in Tumor Ablation for Hepatocellular Carcinoma. Liver Cancer 4(3):176-187. https://https://doi.org/10.1159/000367740
Zhang X, He X, Zeng Q, Tan L, Xu E, Li K et al (2021) Utility of Fusion Imaging for Percutaneous Thermal Ablation of Hepatocellular Carcinoma in the Caudate Lobe. J Vasc Interv Radiol 32(8):1209-1214. https://https://doi.org/10.1016/j.jvir.2021.04.028
Long Y, Xu E, Zeng Q, Ju J, Huang Q, Liang P et al (2020) Intra-procedural real-time ultrasound fusion imaging improves the therapeutic effect and safety of liver tumor ablation in difficult cases. Am J Cancer Res 10(7):2174-2184.
Ahn SJ, Lee JM, Lee DH, Lee SM, Yoon J, Kim YJ et al (2017) Real-time US-CT/MR fusion imaging for percutaneous radiofrequency ablation of hepatocellular carcinoma. J Hepatol 66(2):347-354. https://https://doi.org/10.1016/j.jhep.2016.09.003
Beleù A, Drudi A, Giaretta A, De Robertis R, Fedrigo I, Martone E et al (2021) Operator Evaluation of Ultrasound Fusion Imaging Usefulness in the Percutaneous Ablation of Hepatic Malignancies: A Prospective Study. Ultrasound in Medicine & Biology 47(11):3159-3169. https://https://doi.org/10.1016/j.ultrasmedbio.2021.07.008
Minami Y, Kudo M (2020) Ultrasound fusion imaging technologies for guidance in ablation therapy for liver cancer. J Med Ultrason 47(2):257-263. https://https://doi.org/10.1007/s10396-020-01006-w
Calandri M, Mauri G, Yevich S, Gazzera C, Basile D, Gatti M et al (2019) Fusion Imaging and Virtual Navigation to Guide Percutaneous Thermal Ablation of Hepatocellular Carcinoma: A Review of the Literature. Cardiovasc Inter Rad 42(5):639-647. https://https://doi.org/10.1007/s00270-019-02167-z
Song KD, Lee MW, Rhim H, Kang TW, Cha DI, Sinn DH et al (2018) Percutaneous US/MRI Fusion-guided Radiofrequency Ablation for Recurrent Subcentimeter Hepatocellular Carcinoma: Technical Feasibility and Therapeutic Outcomes. Radiology 288(3):878-886. https://https://doi.org/10.1148/radiol.2018172743
Bo X, Xu H, Guo L, Sun L, Li X, Zhao C et al (2017) Ablative safety margin depicted by fusion imaging with post-treatment contrast-enhanced ultrasound and pre-treatment CECT/CEMRI after radiofrequency ablation for liver cancers. Brit J Radiol 90(1078):20170063. https://https://doi.org/10.1259/bjr.20170063
Dong Y, Wang W, Mao F, Ji Z, Huang B (2016) Application of imaging fusion combining contrast-enhanced ultrasound and magnetic resonance imaging in detection of hepatic cellular carcinomas undetectable by conventional ultrasound. J Gastroen Hepatol 31(4):822-828. https://https://doi.org/10.1111/jgh.13202
Yoon JH, Lee JM, Klotz E, Woo H, Yu MH, Joo I et al (2018) Prediction of Local Tumor Progression after Radiofrequency Ablation (RFA) of Hepatocellular Carcinoma by Assessment of Ablative Margin Using Pre-RFA MRI and Post-RFA CT Registration. Korean J Radiol 19(6):1053-1065. https://https://doi.org/10.3348/kjr.2018.19.6.1053
Ma QP, Xu EJ, Zeng QJ, Su ZZ, Tan L, Chen JX et al (2019) Intraprocedural computed tomography/magnetic resonance-contrast-enhanced ultrasound fusion imaging improved thermal ablation effect of hepatocellular carcinoma: Comparison with conventional ultrasound. Hepatol Res 49(7):799-809. https://https://doi.org/10.1111/hepr.13336
Khalilzadeh O, Baerlocher MO, Shyn PB, Connolly BL, Devane AM, Morris CS et al (2017) Proposal of a New Adverse Event Classification by the Society of Interventional Radiology Standards of Practice Committee. J Vasc Interv Radiol 28(10):1432-1437. https://https://doi.org/10.1016/j.jvir.2017.06.019
Funding
This work was supported by Science and Technology Planning Program of Guangzhou, China (No. 201704020164).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
There are no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, J., Li, L., Zeng, Q. et al. Prevention of major biliary complications by fusion imaging for thermal ablation of malignant liver tumors adjacent to the bile ducts: a preliminary comparative study. Abdom Radiol 47, 4245–4253 (2022). https://doi.org/10.1007/s00261-022-03631-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-022-03631-0