Abstract
Purpose
To audit the diagnostic accuracy of MRI for staging early and polyp rectal cancers with the purpose of identifying scope for service improvement.
Methods
This is an IRB approved retrospective study of patients who underwent staging MRI for rectal growths followed by upfront TME type surgery or local excision without neoadjuvant therapy between 2018 and 2021. MR-T-stage was compared with surgical histopathology. The degree of stage migration in the multidisciplinary team meetings (MDT) was assessed and training needs were identified.
Results
53 patients (32 males) with a mean (SD) age of 56.7 (13.6) years with 54 rectal lesions and underwent trans-anal excision (n = 18) or upfront surgery (n = 35) were included. Pathology showed < / = pT1 stage in n = 18 and > / = pT2 stage in n = 36. Radio-pathological concordance rate was 38.9% and 74.1%, respectively, for primary reports and MDT reads, respectively, and during MDT, the rates improved by 44.5% and 30.5% for < / = pT1 and > / = pT2 stages ,respectively. The overall T-stage migration rate at MDT was 44.6% (25/54) and the migration rate was higher (61.1%) for < / = pT1 stage lesions. The best sensitivity, specificity, PPV, NPV and accuracy of MRI for T-staging was 83.3%, 91.6%, 83.3%, 91.6% and 88.8%, respectively.
Conclusion
Radio-pathological correlation for MRI T-stage is excellent for MDT reads by experienced radiologists. MDT reads lead to significant down-staging of T-stage in polyp and early rectal cancer thereby improving radio-path correlation.
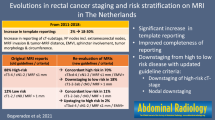
Graphical abstract








Similar content being viewed by others
Abbreviations
- ERUS:
-
Endorectal ultrasound
- EMVI:
-
Extramural vascular invasion
- MDT:
-
Multi-disciplinary team
- CRM:
-
Circumferential resection margin
- TAE:
-
Trans-anal excision
- TAMIS:
-
Trans-anal minimally invasive surgery
References
Morris EJA, Taylor EF, Thomas JD, Quirke P, Finan PJ, Coleman MP, et al. Thirty-day postoperative mortality after colorectal cancer surgery in England. Gut. 2011 60(6):806–13.
East JE, Bhandari P, Dolwani S, MacCarthy F, Rutter MD, Saunders BP. Endoscopic excision of significant polyp and early colorectal cancer lesions. Colorectal Disease. 2019;21(S1):37–40.
Cunningham C. Transanal excision. Colorectal Disease. 2019;21(S1):41–4.
Myint AS, Stewart A, Mills J, Sripadam R, Whitmarsh K, Roy R, et al. Treatment: the role of contact X-ray brachytherapy (Papillon) in the management of early rectal cancer. Colorectal Disease. 2019;21(S1):45–52.
West NP, Langman G, Haboubi N, Carey F, Henry J, Morgan M, et al. Significant polyps and early colorectal cancer: the importance of high-quality standardized histopathology. Colorectal Disease. 2019;21(S1):53–6.
Marusch F, Ptok H, Sahm M, Schmidt U, Ridwelski K, Gastinger I, et al. Endorectal ultrasound in rectal carcinoma--do the literature results really correspond to the realities of routine clinical care? Endoscopy. 2011 May;43(5):425–31.
Ashraf S, Hompes R, Slater A, Lindsey I, Bach S, Mortensen NJ, et al. A critical appraisal of endorectal ultrasound and transanal endoscopic microsurgery and decision-making in early rectal cancer. Colorectal Dis. 2012 Jul;14(7):821–6.
Balyasnikova S, Brown G. The MRI assessment of SPECC (significant polyps and early colorectal cancer) lesions. Colorectal Disease. 2019;21(S1):19–22.
Balyasnikova S, Read J, Wotherspoon A, Rasheed S, Tekkis P, Tait D, et al. Diagnostic accuracy of high-resolution MRI as a method to predict potentially safe endoscopic and surgical planes in patients with early rectal cancer. BMJ Open Gastroenterology. 2017 Jul 1;4(1):e000151.
Beets-Tan RGH, Lambregts DMJ, Maas M, Bipat S, Barbaro B, Curvo-Semedo L, et al. Magnetic resonance imaging for clinical management of rectal cancer: Updated recommendations from the 2016 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol. 2018 Apr;28(4):1465–75.
Chandramohan A, Siddiqi UM, Mittal R, Eapen A, Jesudason MR, Ram TS, et al. (2020) Diffusion weighted imaging improves diagnostic ability of MRI for determining complete response to neoadjuvant therapy in locally advanced rectal cancer. Eur J Radiol Open [Internet] [cited 2021 May 17], Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7044654/
Vaughan-Shaw PG, Wheeler JMD, Borley NR. The impact of a dedicated multidisciplinary team on the management of early rectal cancer. Colorectal Dis. 2015 Aug;17(8):704–9.
De Vargas Macciucca M, Casale A, Manganaro L, Floriani I, Fiore F, Marchetti L, et al. Rectal villous tumors: MR features and correlation with TRUS in the preoperative evaluation. Eur J Radiol. 2010 Feb;73(2):329–33.
Raynaud L, Mege D, Zappa M, Guedj N, Vilgrain V, Panis Y. Is magnetic resonance imaging useful for the management of patients with rectal villous adenoma? A study of 45 consecutive patients treated by transanal endoscopic microsurgery. Int J Colorectal Dis. 2018 Dec;33(12):1695–701.
Royal Marsden NHS Foundation Trust. Mri IN STaging REctal Polyp Planes [Internet]. clinicaltrials.gov; 2018 Sep [cited 2022 Mar 28]. Report No.: NCT02532803. Available from: https://clinicaltrials.gov/ct2/show/NCT02532803
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest or relevant financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chandramohan, A., Patra, A., Eapen, A. et al. MDT stage migration in MRI of significant rectal polyps and early rectal cancers. Abdom Radiol 47, 2760–2769 (2022). https://doi.org/10.1007/s00261-022-03570-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-022-03570-w