Abstract
Purpose
To investigate the proportion of clinically significant adrenal lesions in patients with a subcentimeter adrenal lesion, and the sensitivity of a cutoff size of 10 mm on computed tomography (CT).
Methods
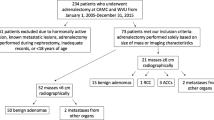
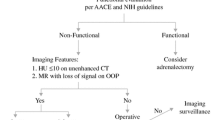
This retrospective study included consecutive 547 non-oncologic patients who underwent adrenal CT. Clinically significant adrenal lesions were defined as those that were biochemically abnormal (n = 99) or surgically resected according to the clinician’s decision (n = 23). Long-axis diameters (LDs) and short-axis diameters (SDs) of the lesions were measured on CT by two independent readers. Likelihood of the focal lesion was analyzed using a five-point scale (1 = very low; 5 = very high). 66 Sensitivities for clinically significant lesions were analyzed according to cutoff size. Proportions of the clinically significant lesions for subcentimeter lesions were analyzed according to the visual score.
Results
Sensitivities for clinically significant lesions for cutoffs of 10, 15, and 20 mm were 93%, 79%, and 63% for LD and 85%, 61%, and 49% for SD for Reader 1 and 89%, 78%, and 65% for LD and 80%, 65%, and 48% for SD for Reader 2, respectively (p < 0.001 for 10 mm versus the other cutoffs). In subcentimeter lesions with visual scores of 1–3, the proportions of clinically significant lesions were 5.4% for LD or SD for Reader 1 and 6.6% for LD and 7.7% for SD for Reader 2, respectively.
Conclusion
A lesion LD of ≥ 10 mm was a reasonable cutoff for determining adrenal abnormality. Subcentimeter lesions without visually high suspicion had a low risk of clinical significant lesions in our study cohort. Higher cutoffs significantly decreased sensitivity.




Similar content being viewed by others
References
Mayo-Smith WW, Song JH, Boland GL, Francis IR, Israel GM, Mazzaglia PJ, Berland LL, Pandharipande PV (2017) Management of Incidental Adrenal Masses: A White Paper of the ACR Incidental Findings Committee. J Am Coll Radiol 14:1038-1044. https://doi.org/10.1016/j.jacr.2017.05.001
Glazer DI, Mayo-Smith WW (2020) Management of incidental adrenal masses: an update. Abdom Radiol (NY) 45:892-900. https://doi.org/10.1007/s00261-019-02149-2
Expert Panel on Urological I, Mody RN, Remer EM, Nikolaidis P, Khatri G, Dogra VS, Ganeshan D, Gore JL, Gupta RT, Heilbrun ME, Lyshchik A, Mayo-Smith WW, Purysko AS, Savage SJ, Smith AD, Wang ZJ, Wolfman DJ, Wong-You-Cheong JJ, Yoo DC, Lockhart ME (2021) ACR Appropriateness Criteria(R) Adrenal Mass Evaluation: 2021 Update. J Am Coll Radiol 18:S251-S267. https://doi.org/10.1016/j.jacr.2021.08.010
Fassnacht M, Arlt W, Bancos I, Dralle H, Newell-Price J, Sahdev A, Tabarin A, Terzolo M, Tsagarakis S, Dekkers OM (2016) Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol 175:G1-G34. https://doi.org/10.1530/EJE-16-0467
Nieman LK (2010) Approach to the patient with an adrenal incidentaloma. J Clin Endocrinol Metab 95:4106-4113. https://doi.org/10.1210/jc.2010-0457
Kang S, Oh YL, Park SY (2021) Distinguishing pheochromocytoma from adrenal adenoma by using modified computed tomography criteria. Abdom Radiol (NY) 46:1082–1090. https://doi.org/10.1007/s00261-020-02764-4
Koo TK, Li MY (2016) A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med 15:155-163. https://doi.org/10.1016/j.jcm.2016.02.012
Jakobsson U, Westergren A (2005) Statistical methods for assessing agreement for ordinal data. Scand J Caring Sci 19:427-431. https://doi.org/10.1111/j.1471-6712.2005.00368.x
Vincent JM, Morrison ID, Armstrong P, Reznek RH (1994) The size of normal adrenal glands on computed tomography. Clin Radiol 49:453-455. https://doi.org/10.1016/s0009-9260(05)81739-8
Mayo-Smith WW, Boland GW, Noto RB, Lee MJ (2001) State-of-the-art adrenal imaging. Radiographics 21:995-1012. https://doi.org/10.1148/radiographics.21.4.g01jl21995
John R, Putta T, Simon B, Eapen A, Jebasingh F, Thomas N, Rajaratnam S (2018) Normal adrenal gland thickness on computerized tomography in an Asian Indian adult population. Indian J Radiol Imaging 28:465-469. https://doi.org/10.4103/ijri.IJRI_129_18
Montagne JP, Kressel HY, Korobkin M, Moss AA (1978) Computed tomography of the normal adrenal glands. AJR Am J Roentgenol 130:963-966. https://doi.org/10.2214/ajr.130.5.963
Schneller J, Reiser M, Beuschlein F, Osswald A, Pallauf A, Riester A, Tietze JK, Reincke M, Degenhart C (2014) Linear and volumetric evaluation of the adrenal gland--MDCT-based measurements of the adrenals. Acad Radiol 21:1465-1474. https://doi.org/10.1016/j.acra.2014.06.008
Kebebew E (2021) Adrenal Incidentaloma. N Engl J Med 384:1542-1551. https://doi.org/10.1056/NEJMcp2031112
Kawashima A, Sandler CM, Fishman EK, Charnsangavej C, Yasumori K, Honda H, Ernst RD, Takahashi N, Raval BK, Masuda K, Goldman SM (1998) Spectrum of CT findings in nonmalignant disease of the adrenal gland. Radiographics 18:393-412. https://doi.org/10.1148/radiographics.18.2.9536486
Park SY, Oh YT, Jung DC, Rhee Y (2015) Prediction of Adrenal Adenomas With Hypercortisolism by Using Adrenal Computed Tomography: Emphasis on Contralateral Adrenal Thinning. J Comput Assist Tomogr 39:741-746. https://doi.org/10.1097/RCT.0000000000000269
Lattin GE, Jr., Sturgill ED, Tujo CA, Marko J, Sanchez-Maldonado KW, Craig WD, Lack EE (2014) From the radiologic pathology archives: Adrenal tumors and tumor-like conditions in the adult: radiologic-pathologic correlation. Radiographics 34:805-829. https://doi.org/10.1148/rg.343130127
Szolar DH, Korobkin M, Reittner P, Berghold A, Bauernhofer T, Trummer H, Schoellnast H, Preidler KW, Samonigg H (2005) Adrenocortical carcinomas and adrenal pheochromocytomas: mass and enhancement loss evaluation at delayed contrast-enhanced CT. Radiology 234:479-485. https://doi.org/10.1148/radiol.2342031876
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, M.K., Kang, K.A. & Park, S.Y. Clinical significance of a 10-mm cutoff size for adrenal lesions: a retrospective study with 547 non-oncologic patients undergoing adrenal computed tomography. Abdom Radiol 47, 1091–1097 (2022). https://doi.org/10.1007/s00261-021-03405-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-021-03405-0