Abstract
Purpose
To compare quantitative biliary measurements obtained with three different magnetic resonance cholangiopancreatography (MRCP) acquisition methods.
Methods
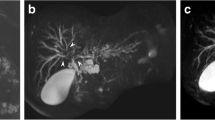
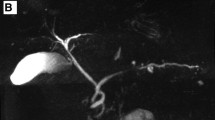
This retrospective study was IRB-approved. Patients with combinations of clinically indicated 3D FSE MRCP with sensitivity encoding (SENSE), 3D FSE SENSE MRCP with compressed sensing (CS-FSE; acceleration factor 8), and 3D gradient and spin-echo (GRASE) MRCP, acquired between October 2018 and March 2020, were included. The MRCP + Tuning Threshold algorithm (Perspectum Ltd., Oxford, UK) was used to segment 3D biliary models from MRCP data, with multiple metrics quantified from the models. Single measure, two-way, mixed-effects intra-class correlations, Bland–Altman analyses, and Wilcoxon signed-rank tests were used to compare quantitative measurements.
Results
From 160 MRCP datasets (25 3D FSE, 67 3D CS-FSE, 68 3D GRASE) in 69 patients, 48 datasets (7 [28%] 3D FSE, 14 [21%] 3D CS-FSE, 27 [40%] 3D GRASE) failed post-processing due to motion artifacts. The remaining 112 MRCP datasets (18 3D FSE, 53 3D CS-FSE, 41 3D GRASE) from 60 patients were included in the analysis. There was good to excellent agreement between 3D FSE and 3D CS-FSE MRCP for diameter of the left and right hepatic ducts, biliary volume, number and length of ducts, and total length of dilations (ICC: 0.83–0.93). The only metrics that exhibited good agreement between 3D FSE and 3D GRASE MRCP were biliary volume (ICC: 0.75) and total number of dilations (ICC: 0.77).
Conclusion
3D CS-FSE MRCP produces comparable biliary diameter metrics and global duct quantification to 3D FSE MRCP at a significantly reduced acquisition time.



Similar content being viewed by others
References
Barish MA, Yucel EK, Ferrucci JT (1999) Magnetic resonance cholangiopancreatography. N Engl J Med 341 (4):258-264. doi:https://doi.org/10.1056/nejm199907223410407
Nandalur KR, Hussain HK, Weadock WJ, Wamsteker EJ, Johnson TD, Khan AS, D'Amico AR, Ford MK, Nandalur SR, Chenevert TL (2008) Possible biliary disease: diagnostic performance of high-spatial-resolution isotropic 3D T2-weighted MRCP. Radiology 249 (3):883-890. doi:https://doi.org/10.1148/radiol.2493080389
Tipnis NA, Werlin SL (2007) The use of magnetic resonance cholangiopancreatography in children. Curr Gastroenterol Rep 9 (3):225-229. doi:https://doi.org/10.1007/s11894-007-0023-2
Masui T, Katayama M, Kobayashi S, Nozaki A, Sugimura M, Ikeda M, Sakahara H (2006) Magnetic resonance cholangiopancreatography: comparison of respiratory-triggered three-dimensional fast-recovery fast spin-echo with parallel imaging technique and breath-hold half-Fourier two-dimensional single-shot fast spin-echo technique. Radiat Med 24 (3):202-209. doi:https://doi.org/10.1007/s11604-005-1528-y
Chavhan GB, Almehdar A, Moineddin R, Gupta S, Babyn PS (2013) Comparison of respiratory-triggered 3-D fast spin-echo and single-shot fast spin-echo radial slab MR cholangiopancreatography images in children. Pediatr Radiol 43 (9):1086-1092. doi:https://doi.org/10.1007/s00247-013-2663-8
Yoon JH, Lee SM, Kang HJ, Weiland E, Raithel E, Son Y, Kiefer B, Lee JM (2017) Clinical Feasibility of 3-Dimensional Magnetic Resonance Cholangiopancreatography Using Compressed Sensing: Comparison of Image Quality and Diagnostic Performance. Invest Radiol 52 (10):612-619. doi:https://doi.org/10.1097/RLI.0000000000000380
Anupindi SA, Victoria T (2008) Magnetic resonance cholangiopancreatography: techniques and applications. Magn Reson Imaging Clin N Am 16 (3):453–466, v. doi:https://doi.org/10.1016/j.mric.2008.04.005
Chandarana H, Doshi AM, Shanbhogue A, Babb JS, Bruno MT, Zhao T, Raithel E, Zenge MO, Li G, Otazo R (2016) Three-dimensional MR Cholangiopancreatography in a Breath Hold with Sparsity-based Reconstruction of Highly Undersampled Data. Radiology 280 (2):585-594. doi:https://doi.org/10.1148/radiol.2016151935
Feng L, Benkert T, Block KT, Sodickson DK, Otazo R, Chandarana H (2017) Compressed sensing for body MRI. J Magn Reson Imaging 45 (4):966-987. doi:https://doi.org/10.1002/jmri.25547
Seo N, Park MS, Han K, Kim D, King KF, Choi JY, Kim H, Kim HJ, Lee M, Bae H, Kim MJ (2017) Feasibility of 3D navigator-triggered magnetic resonance cholangiopancreatography with combined parallel imaging and compressed sensing reconstruction at 3T. J Magn Reson Imaging 46 (5):1289-1297. doi:https://doi.org/10.1002/jmri.25672
Zhu L, Wu X, Sun Z, Jin Z, Weiland E, Raithel E, Qian T, Xue H (2018) Compressed-Sensing Accelerated 3-Dimensional Magnetic Resonance Cholangiopancreatography: Application in Suspected Pancreatic Diseases. Invest Radiol 53 (3):150-157. doi:https://doi.org/10.1097/RLI.0000000000000421
Feinberg DA, Oshio K (1991) GRASE (gradient- and spin-echo) MR imaging: a new fast clinical imaging technique. Radiology 181 (2):597-602. doi:https://doi.org/10.1148/radiology.181.2.1924811
Yoshikawa T, Mitchell DG, Hirota S, Ohno Y, Yoshigi J, Maeda T, Fujii M, Sugimura K (2006) Focal liver lesions: breathhold gradient- and spin-echo T2-weighted imaging for detection and characterization. J Magn Reson Imaging 23 (4):520-528. doi:https://doi.org/10.1002/jmri.20544
Gilligan LA, Trout AT, Lam S, Singh R, Tkach JA, Serai SD, Miethke AG, Dillman JR (2020) Differentiating pediatric autoimmune liver diseases by quantitative magnetic resonance cholangiopancreatography. Abdom Radiol (NY) 45 (1):168-176. doi:https://doi.org/10.1007/s00261-019-02184-z
Goldfinger MH, Ridgway GR, Ferreira C, Langford CR, Cheng L, Kazimianec A, Borghetto A, Wright TG, Woodward G, Hassanali N, Nicholls RC, Simpson H, Waddell T, Vikal S, Mavar M, Rymell S, Wigley I, Jacobs J, Kelly M, Banerjee R, Brady JM (2020) Quantitative MRCP Imaging: Accuracy, Repeatability, Reproducibility, and Cohort-Derived Normative Ranges. J Magn Reson Imaging 52 (3):807-820. doi:https://doi.org/10.1002/jmri.27113
Ralli GP, Ridway GR, Brady M (2020) Segmentation of the biliary tree from MRCP images via the monogenic signal. In: Papież B., Namburete A., Yaqub M., Noble J. (ed) Medical Image Understanding and Analysis. Communications in Computer and Information Science. Springer, Cham. p 105–117
Portney LG, Watkins MP (2000). Foundations of clinical research: applications to practice. New Jersey: Prentice Hall
Mannes I, Dallongeville A, Badat N, Beaussier H, Chatellier G, Zins M (2020) Breath-hold compressed-sensing 3D MR cholangiopancreatography compared to free-breathing 3D MR cholangiopancreatography: prospective study of image quality and diagnostic performance in pancreatic disorders. Abdom Radiol (NY) 45 (4):1082-1091. doi:https://doi.org/10.1007/s00261-019-02254-2
Tokoro H, Yamada A, Suzuki T, Kito Y, Adachi Y, Hayashihara H, Nickel MD, Maruyama K, Fujinaga Y (2020) Usefulness of breath-hold compressed sensing accelerated three-dimensional magnetic resonance cholangiopancreatography (MRCP) added to respiratory-gating conventional MRCP. Eur J Radiol 122:108765. doi:https://doi.org/10.1016/j.ejrad.2019.108765
Morimoto D, Hyodo T, Kamata K, Kadoba T, Itoh M, Fukushima H, Chiba Y, Takenaka M, Mochizuki T, Ueda Y, Miyagoshi K, Kudo M, Ishii K (2020) Navigator-triggered and breath-hold 3D MRCP using compressed sensing: image quality and method selection factor assessment. Abdom Radiol (NY) 45 (10):3081-3091. doi:https://doi.org/10.1007/s00261-020-02403-y
Taron J, Weiss J, Notohamiprodjo M, Kuestner T, Bamberg F, Weiland E, Kuehn B, Martirosian P (2018) Acceleration of Magnetic Resonance Cholangiopancreatography Using Compressed Sensing at 1.5 and 3 T: A Clinical Feasibility Study. Invest Radiol 53 (11):681–688. doi:https://doi.org/10.1097/RLI.0000000000000489
Zhu L, Xue H, Sun Z, Qian T, Weiland E, Kuehn B, Asbach P, Hamm B, Jin Z (2018) Modified breath-hold compressed-sensing 3D MR cholangiopancreatography with a small field-of-view and high resolution acquisition: Clinical feasibility in biliary and pancreatic disorders. J Magn Reson Imaging 48 (5):1389-1399. doi:https://doi.org/10.1002/jmri.26049
Nam JG, Lee JM, Kang HJ, Lee SM, Kim E, Peeters JM, Yoon JH (2018) GRASE Revisited: breath-hold three-dimensional (3D) magnetic resonance cholangiopancreatography using a Gradient and Spin Echo (GRASE) technique at 3T. Eur Radiol 28 (9):3721-3728. doi:https://doi.org/10.1007/s00330-017-5275-0
Yoshida M, Nakaura T, Inoue T, Tanoue S, Takada S, Utsunomiya D, Tsumagari S, Harada K, Yamashita Y (2018) Magnetic resonance cholangiopancreatography with GRASE sequence at 3.0T: does it improve image quality and acquisition time as compared with 3D TSE? Eur Radiol 28 (6):2436–2443. doi:https://doi.org/10.1007/s00330-017-5240-y
Funding
Perspectum Ltd. provided in-kind research support for this project to Drs. Jonathan R. Dillman and Andrew T. Trout.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. Jonathan R. Dillman and Andrew T. Trout have received grant support from Perspectum Ltd, Siemens Medical Solutions, and Canon Medical Systems. Dr. Dillman has also received in-kind research support from Resoundant, Inc. and Philips Heathcare. No other authors have conflicts of interest to report.
Ethical approval
This study was approved by our institutional review board and was compliant with the Health Insurance Portability and Accountability Act.
Consent to participate
The requirement for participant informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mahalingam, N., Ralli, G.P., Trout, A.T. et al. Comparison of quantitative 3D magnetic resonance cholangiography measurements obtained using three different image acquisition methods. Abdom Radiol 47, 196–208 (2022). https://doi.org/10.1007/s00261-021-03330-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-021-03330-2