Abstract
Objective
The intraductal papillary mucinous neoplasm (IPMN) of the pancreas is regarded as a precursor to pancreatic cancer; this study aimed to develop and validate a model based on CT characteristics for the non-invasive prediction of the high-risk IPMN of the pancreas.
Materials and methods
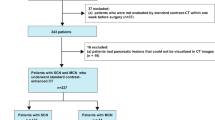
In this retrospective study, all patients underwent multidetector CT and surgical resection. A prediction model was developed based on a training set consisting of 136 patients with low-risk IPMN and 85 patients with high-risk IPMN between October 2012 and April 2019, and a multivariable logistic regression model was adopted to establish a nomogram. The nomogram performance was determined by its discrimination, calibration, and clinical usefulness. The model was validated in 80 consecutive patients between May 2019 and April 2020, of which 47 and 33 patients had low-risk and high-risk IPMNs, respectively.
Results
The multivariable logistic regression model of CT characteristics included the enhancing mural nodule size, the main pancreatic duct (MPD) diameter, the abrupt change in caliber of the MPD with distal pancreatic atrophy, cyst size, thickened enhancing cyst wall, and the presence of lymphadenopathy. The individualized prediction nomogram using these predictors of the high-risk IPMN achieved an area under the curve (AUC) of 0.92 (95% CI 0.88–0.95) in the training set and 0.87 (95% CI 0.79–0.95) in the validation set. The decision curve analysis demonstrated that the nomogram was clinically useful.
Conclusion
The CT nomogram, which is a non-invasive predictive tool, can preoperatively predict the risk of malignant IPMN and help identify patients who require a surgical procedure.





Similar content being viewed by others
References
van Huijgevoort NCM, Del Chiaro M, Wolfgang CL, et al. (2019) Diagnosis and management of pancreatic cystic neoplasms: current evidence and guidelines. Nat Rev Gastroenterol Hepatol 16 (11):676–89. https://doi.org/10.1038/s41575-019-0195-x
European Study Group on Cystic Tumours of the P. (2018) European evidence-based guidelines on pancreatic cystic neoplasms. Gut 67 (5):789–804. https://doi.org/10.1136/gutjnl-2018-316027
Choi SH, Park SH, Kim KW, et al. (2017) Progression of Unresected Intraductal Papillary Mucinous Neoplasms of the Pancreas to Cancer: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol 15 (10):1509–20 e4. https://doi.org/10.1016/j.cgh.2017.03.020
Tanaka M, Fernandez-del Castillo C, Adsay V, et al. (2012) International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology 12 (3):183–97. https://doi.org/10.1016/j.pan.2012.04.004
Sugimoto M, Elliott IA, Nguyen AH, et al. (2017) Assessment of a Revised Management Strategy for Patients With Intraductal Papillary Mucinous Neoplasms Involving the Main Pancreatic Duct. JAMA Surg 152 (1):e163349. https://doi.org/10.1001/jamasurg.2016.3349
Tanaka M, Fernandez-Del Castillo C, Kamisawa T, et al. (2017) Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology 17 (5):738–53. https://doi.org/10.1016/j.pan.2017.07.007
Shimizu Y, Kanemitsu Y, Sano T, et al. (2010) A nomogram for predicting the probability of carcinoma in patients with intraductal papillary-mucinous neoplasm. World J Surg 34 (12):2932–8. https://doi.org/10.1007/s00268-010-0785-9
Correa-Gallego C, Do R, Lafemina J, et al. (2013) Predicting dysplasia and invasive carcinoma in intraductal papillary mucinous neoplasms of the pancreas: development of a preoperative nomogram. Ann Surg Oncol 20 (13):4348–55. https://doi.org/10.1245/s10434-013-3207-z
Shimizu Y, Yamaue H, Maguchi H, et al. (2015) Validation of a nomogram for predicting the probability of carcinoma in patients with intraductal papillary mucinous neoplasm in 180 pancreatic resection patients at 3 high-volume centers. Pancreas 44 (3):459–64. https://doi.org/10.1097/MPA.0000000000000269
Goh BK, Teo JY, Allen JC, Jr., et al. (2016) Preoperative platelet-to-lymphocyte ratio improves the performance of the international consensus guidelines in predicting malignant pancreatic cystic neoplasms. Pancreatology 16 (5):888–92. https://doi.org/10.1016/j.pan.2016.06.660
Jang JY, Park T, Lee S, et al. (2017) Proposed Nomogram Predicting the Individual Risk of Malignancy in the Patients With Branch Duct Type Intraductal Papillary Mucinous Neoplasms of the Pancreas. Ann Surg 266 (6):1062–8. https://doi.org/10.1097/SLA.0000000000001985
Attiyeh MA, Fernandez-Del Castillo C, Al Efishat M, et al. (2018) Development and Validation of a Multi-institutional Preoperative Nomogram for Predicting Grade of Dysplasia in Intraductal Papillary Mucinous Neoplasms (IPMNs) of the Pancreas: A Report from The Pancreatic Surgery Consortium. Ann Surg 267 (1):157–63. https://doi.org/10.1097/SLA.0000000000002015
Shimizu Y, Hijioka S, Hirono S, et al. (2020) New Model for Predicting Malignancy in Patients With Intraductal Papillary Mucinous Neoplasm. Ann Surg 272 (1):155–62. https://doi.org/10.1097/SLA.0000000000003108
Moons KG, Altman DG, Reitsma JB, et al. (2015) Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med 162 (1):W1–73. https://doi.org/10.7326/M14-0698
Lee JE, Choi SY, Min JH, et al. (2019) Determining Malignant Potential of Intraductal Papillary Mucinous Neoplasm of the Pancreas: CT versus MRI by Using Revised 2017 International Consensus Guidelines. Radiology 293 (1):134–43. https://doi.org/10.1148/radiol.2019190144
Chiu SS, Lim JH, Lee WJ, et al. (2006) Intraductal papillary mucinous tumour of the pancreas: differentiation of malignancy and benignancy by CT. Clin Radiol 61 (9):776–83. https://doi.org/10.1016/j.crad.2006.04.008
Kang HJ, Lee JM, Joo I, et al. (2016) Assessment of Malignant Potential in Intraductal Papillary Mucinous Neoplasms of the Pancreas: Comparison between Multidetector CT and MR Imaging with MR Cholangiopancreatography. Radiology 279 (1):128–39. https://doi.org/10.1148/radiol.2015150217
Dorfman RE, Alpern MB, Gross BH, et al. (1991) Upper abdominal lymph nodes: criteria for normal size determined with CT. Radiology 180 (2):319–22. https://doi.org/10.1148/radiology.180.2.2068292
Nagtegaal ID, Odze RD, Klimstra D, et al. (2020) The 2019 WHO classification of tumours of the digestive system. Histopathology 76 (2):182-8. https://doi.org/10.1111/his.13975
Shrout PE, Fleiss JL. (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86 (2):420–8. https://doi.org/10.1037//0033-2909.86.2.420
Howard TJ, Chin AC, Streib EW, et al. (1997) Value of helical computed tomography, angiography, and endoscopic ultrasound in determining resectability of periampullary carcinoma. Am J Surg 174 (3):237–41.
Imai H, Doi R, Kanazawa H, et al. (2010) Preoperative assessment of para-aortic lymph node metastasis in patients with pancreatic cancer. Int J Clin Oncol 15 (3):294–300. https://doi.org/10.1007/s10147-010-0066-5
Midwinter MJ, Beveridge CJ, Wilsdon JB, et al. (1999) Correlation between spiral computed tomography, endoscopic ultrasonography and findings at operation in pancreatic and ampullary tumours. Br J Surg 86 (2):189–93. https://doi.org/10.1046/j.1365-2168.1999.01042.x
Nanashima A, Tobinaga S, Abo T, et al. (2012) Evaluation of surgical resection for pancreatic carcinoma at a Japanese single cancer institute. Hepatogastroenterology 59 (115):911–5. https://doi.org/10.5754/hge10038
Igarashi T, Ashida H, Morikawa K, et al. (2018) Evaluating the malignant potential of intraductal papillary mucinous neoplasms of the pancreas: added value of non-enhanced endoscopic ultrasound to supplement non-enhanced magnetic resonance imaging. Pol J Radiol 83:e426-e36. https://doi.org/10.5114/pjr.2018.79617
Kwong WT, Lawson RD, Hunt G, et al. (2015) Rapid Growth Rates of Suspected Pancreatic Cyst Branch Duct Intraductal Papillary Mucinous Neoplasms Predict Malignancy. Dig Dis Sci 60 (9):2800–6. https://doi.org/10.1007/s10620-015-3679-8
Kang HJ, Lee DH, Lee JM, et al. (2020) Clinical Feasibility of Abbreviated Magnetic Resonance With Breath-Hold 3-Dimensional Magnetic Resonance Cholangiopancreatography for Surveillance of Pancreatic Intraductal Papillary Mucinous Neoplasm. Invest Radiol 55 (5):262–9. https://doi.org/10.1097/RLI.0000000000000636
Funding
This work was supported in part by the National Natural Science Foundation of China (81871352); Major Clinical Research Project of Shanghai Shenkang Hospital Development Center (SHDC2020CR4073); The Natural Science Foundation of Shanghai Science and Technology Innovation Action Plan (21ZR1478500); 234 Platform Discipline Consolidation Foundation Project (2019YPT001).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fang, X., Liu, F., Li, J. et al. Computed tomography nomogram to predict a high-risk intraductal papillary mucinous neoplasm of the pancreas. Abdom Radiol 46, 5218–5228 (2021). https://doi.org/10.1007/s00261-021-03247-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-021-03247-w