Abstract
Purpose
To assess chronic liver disease (CLD) using multiparametric US in a private practice setting in a cohort of patients with increased skin-to-liver distance.
Methods
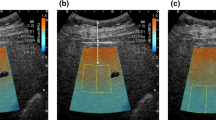
110 consecutive patients with increased skin-to-liver distance scheduled for US assessment of CLD were reviewed for study completion time, liver stiffness values (LS), attenuation imaging, and shear wave dispersion slope. The ROI was placed 2 cm below the liver capsule. The study included patients with NAFLD/NASH (68), hepatitis C (30), prior Fontan surgery (1), elevated liver function tests (5), alcohol abuse (3), hepatitis B (2), and primary biliary cirrhosis (1). IQR/M values were obtained. Comparison of less experienced sonographers (LES) and more experienced sonographers (MES) were evaluated through Student’s t test for independent data. Pearson coefficient r of correlation among quantitative variables was calculated.
Results
The mean time to perform the exam was 129.7 ± 62.1 s. There was a statistically significant difference between LES and MES. The mean IQR/M for LS was 12.3 ± 5.5% m/s. Overall, in a cohort of difficult patients, 4.5% of LS values were not reliable. Fat quantification using attenuation imaging had a mean value of 0.60 ± 0.15 dB/cm/MHz (range 0.35–0.98 cm/dB/MHz) with an IQR/M of 14.7 ± 9.2%. Less reliable measurements of steatosis were obtained in 4.5% of patients. The mean shear wave dispersion slope was 12.74 ± 4.05 (m/s)/kHz (range 7.7–27.5 (m/s)/kHz) with an IQR/M of 38.7 ± 20.2% (range 3–131%). 20.9% of patients had values suggestive of compensated advanced chronic liver disease (cACLD).
Conclusion
Multiparametric US can provide assessment of CLD in less than 3 min in most patients and identify patients at risk for cACLD.



Similar content being viewed by others
References
Asrani, S.K., et al., Burden of liver diseases in the world. J Hepatol, 2019. 70(1): p. 151-171.
Younossi, Z.M., et al., Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology, 2016. 64(1): p. 73-84.
European Association for the Study of the, L., D. European Association for the Study of, and O. European Association for the Study of, EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol, 2016. 64(6): p. 1388–402.
Chalasani, N., et al., The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology, 2018. 67(1): p. 328-357.
Eslam, M., A.J. Sanyal, and J. George, Toward More Accurate Nomenclature for Fatty Liver Diseases. Gastroenterology, 2019. 157(3): p. 590-593.
Barr, R.G., Shear wave liver elastography. Abdom Radiol (NY), 2018. 43(4): p. 800-807.
Barr, R.G., et al., Elastography Assessment of Liver Fibrosis: Society of Radiologists in Ultrasound Consensus Conference Statement. Radiology, 2015. 276(3): p. 845-61.
Lv, S., et al., Noninvasive Quantitative Detection Methods of Liver Fat Content in Nonalcoholic Fatty Liver Disease. J Clin Transl Hepatol, 2018. 6(2): p. 217-221.
Myers, R.P., A. Fong, and A.A. Shaheen, Utilization rates, complications and costs of percutaneous liver biopsy: a population-based study including 4275 biopsies. Liver Int, 2008. 28(5): p. 705-12.
Smith, A.D., et al., Current Imaging Techniques for Noninvasive Staging of Hepatic Fibrosis. AJR Am J Roentgenol, 2019. 213(1): p. 77-89.
Shiina, T., et al., WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 1: basic principles and terminology. Ultrasound Med Biol, 2015. 41(5): p. 1126-47.
Loomba, R. and A.J. Sanyal, The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol, 2013. 10(11): p. 686-90.
Lee, D.H., et al., Accuracy of Two-Dimensional Shear Wave Elastography and Attenuation Imaging for Evaluation of Patients With Nonalcoholic Steatohepatitis. Clin Gastroenterol Hepatol, 2020.
Kwon, E.Y., et al., Usefulness of US attenuation imaging for the detection and severity grading of hepatic steatosis in routine abdominal ultrasonography. Clin Imaging, 2021. 76: p. 53-59.
Koizumi, Y., et al., New diagnostic technique to evaluate hepatic steatosis using the attenuation coefficient on ultrasound B mode. PLoS One, 2019. 14(8): p. e0221548.
Zhang, Y.N., et al., Liver fat imaging-a clinical overview of ultrasound, CT, and MR imaging. Br J Radiol, 2018. 91(1089): p. 20170959.
Raptis, D.A., et al., MRI: the new reference standard in quantifying hepatic steatosis? Gut, 2012. 61(1): p. 117-27.
Ferraioli G, B.A., Barr RG, et. al, Quantification of Liver Fat Content with Ultrasound: A WFUMB Position Paper. UMB, 2021. in press.
Sugimoto, K., et al., The Role of Multiparametric US of the Liver for the Evaluation of Nonalcoholic Steatohepatitis. Radiology, 2020. 296(3): p. 532-540.
Lee, D.H., et al., Shear-Wave Dispersion Slope from US Shear-Wave Elastography: Detection of Allograft Damage after Liver Transplantation. Radiology, 2019. 293(2): p. 327-333.
Byenfeldt, M., A. Elvin, and P. Fransson, On Patient Related Factors and Their Impact on Ultrasound-Based Shear Wave Elastography of the Liver. Ultrasound Med Biol, 2018. 44(8): p. 1606-1615.
Barr, R.G., et al., Update to the Society of Radiologists in Ultrasound Liver Elastography Consensus Statement. Radiology, 2020. 296(2): p. 263-274.
Ferraioli, G., et al., Detection of Liver Steatosis With a Novel Ultrasound-Based Technique: A Pilot Study Using MRI-Derived Proton Density Fat Fraction as the Gold Standard. Clin Transl Gastroenterol, 2019. 10(10): p. e00081.
Ferraioli, G. and R.G. Barr, Ultrasound liver elastography beyond liver fibrosis assessment. World Journal of Gastroenterology, 2020. in press.
Ferraioli, G., R.G. Barr, and J.R. Dillman, Elastography for Pediatric Chronic Liver Disease: A Review and Expert Opinion. J Ultrasound Med, 2020.
Ferraioli, G., et al., Evaluation of Inter-System Variability in Liver Stiffness Measurements. Ultraschall Med, 2019. 40(1): p. 64-75.
Ferraioli, G., et al., Ruling-in and Ruling-out Significant Fibrosis and Cirrhosis in Patients with Chronic Hepatitis C Using a Shear Wave Measurement Method. J Gastrointestin Liver Dis, 2017. 26(2): p. 139-143.
Ferraioli, G., et al., Liver Ultrasound Elastography: An Update to the World Federation for Ultrasound in Medicine and Biology Guidelines and Recommendations. Ultrasound Med Biol, 2018. 44(12): p. 2419-2440.
Morishita, N., et al., Liver stiffness measurement by acoustic radiation force impulse is useful in predicting the presence of esophageal varices or high-risk esophageal varices among patients with HCV-related cirrhosis. J Gastroenterol, 2014. 49(7): p. 1175-82.
Park, Y., et al., A novel model to predict esophageal varices in patients with compensated cirrhosis using acoustic radiation force impulse elastography. PLoS One, 2015. 10(3): p. e0121009.
Attia, D., et al., Evaluation of Liver and Spleen Stiffness with Acoustic Radiation Force Impulse Quantification Elastography for Diagnosing Clinically Significant Portal Hypertension. Ultraschall Med, 2015. 36(6): p. 603-10.
Jansen, C., et al., Algorithm to rule out clinically significant portal hypertension combining Shear-wave elastography of liver and spleen: a prospective multicentre study. Gut, 2016. 65(6): p. 1057-8.
Jeon, S.K., et al., Prospective Evaluation of Hepatic Steatosis Using Ultrasound Attenuation Imaging in Patients with Chronic Liver Disease with Magnetic Resonance Imaging Proton Density Fat Fraction as the Reference Standard. Ultrasound Med Biol, 2019. 45(6): p. 1407-1416.
Yoo, J., et al., Reproducibility of ultrasound attenuation imaging for the noninvasive evaluation of hepatic steatosis. Ultrasonography, 2020. 39(2): p. 121-129.
Bae, J.S., et al., Assessment of hepatic steatosis by using attenuation imaging: a quantitative, easy-to-perform ultrasound technique. Eur Radiol, 2019. 29(12): p. 6499-6507.
Dioguardi Burgio, M., et al., Quantification of hepatic steatosis with ultrasound: promising role of attenuation imaging coefficient in a biopsy-proven cohort. Eur Radiol, 2020. 30(4): p. 2293-2301.
Ferraioli, G., et al., Performance of the Attenuation Imaging Technology in the Detection of Liver Steatosis. J Ultrasound Med, 2020.
Tada, T., et al., Usefulness of Attenuation Imaging with an Ultrasound Scanner for the Evaluation of Hepatic Steatosis. Ultrasound Med Biol, 2019. 45(10): p. 2679-2687.
Ferraioli, G., CAP for the detection of hepatic steatosis in clinical practice. Lancet Gastroenterol Hepatol, 2021. 6(3): p. 151-152.
Lee, D.H., et al., Accuracy of Two-Dimensional Shear Wave Elastography and Attenuation Imaging for Evaluation of Patients With Nonalcoholic Steatohepatitis. Clin Gastroenterol Hepatol, 2021. 19(4): p. 797–805 e7.
Yoo, J., et al., Prospective Validation of Repeatability of Shear Wave Dispersion Imaging for Evaluation of Non-alcoholic Fatty Liver Disease. Ultrasound Med Biol, 2019. 45(10): p. 2688-2696.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
RGB has research grants from Siemens Ultrasound, Philips Ultrasound, Samsung Ultrasound, Mindray Ultrasound, and GE Medical. He is on the speakers bureaus for Siemens Ultrasound, Philips Ultrasound, Mindray, and Canon Medical Systems. He receives royalties from Thieme Publishers. He is one of the advisory panels of Hologic. VA and AD declare that they have no conflict of interest.
Ethical approval
Approved by our local IRB and HIPAA compliant.
Consent to participate
This was a retrospective study and IRB waived consent to participate.
Consent for publication
All authors agree to sole publication of this manuscript in Abdominal Radiology. The manuscript or patient data has not been previously published or presently under review by any other publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aitharaju, V., De Silvestri, A. & Barr, R.G. Assessment of chronic liver disease by multiparametric ultrasound: results from a private practice outpatient facility. Abdom Radiol 46, 5152–5161 (2021). https://doi.org/10.1007/s00261-021-03225-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-021-03225-2