Abstract
Purpose
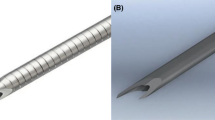
To compare clinical efficacy, subjective radiologist preference, and complication rates for two different core biopsy needles, the Achieve® and Marquee®.
Methods
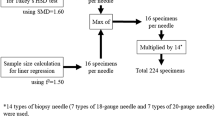
Retrospective review included consecutive patients who underwent 18 gauge non-targeted core liver biopsy, 30 with Achieve® (Merit Medical) and 30 with Marquee® (BD Bard) Pathologist (blinded to needle type) reviewed specimen total length, maximum width, and portal triad count. Sixteen radiologists subjectively rated (1 to 5(best)) each needle for cocking, firing, recoil, chamber exposure, handling, and overall. A medical records search of all (targeted and non-targeted) core liver biopsies 1/1/17–9/30/2020 compared rates of major (requiring transfusion and/or embolization) and minor (self-limited bleeding) hemorrhagic complications. Comparison between needle types was performed using t-test.
Results
For Achieve® and Marquee® needles, the respective mean (SD) for total length(mm) was 29.7(7.0) and 31.9(4.6), p = 0.1; max width(mm) was 0.78(0.1) and 0.85(0.1), p < 0.01; and number of portal triads was 15.3(5.3) and 17.3(5.3), p = 0.2. Radiologists subjectively preferred the Marquee® for several measures including cocking, chamber exposure, and overall (p < 0.02 for each), while the needles were rated similarly for firing, recoil, and handling. Review of 800 cases showed no difference in major (1.0% Achieve®, 1.9% Marquee®, p = 0.5) or minor (1.5% Achieve®, 0.5% Marquee®, p = 0.3) rates of hemorrhagic complications.
Conclusion
Liver biopsy specimens were significantly wider with Marquee® compared to Achieve®. Radiologists preferred the Marquee® for multiple tactile measures, while the major complication rate was not significantly different. While both needles have a similar side-notch design, the Marquee® needle demonstrates better sample quality and higher user preference, without compromising safety.
Graphic abstract



Similar content being viewed by others
References
Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD (2009) Liver biopsy. Hepatology 49: 1017-1044
Hall TC, Deakin C, Atwal GS, Sigh RK (2017) Adequacy of percutaneous non-targeted liver biopsy under real-time ultrasound guidance when comparing the Biopince and Achieve biopsy needle. Br J Radiol 90: 20170397
Hopper KD, Abendroth CS, Sturtz KW, Matthews YL, Stevens LA, Shirk SJ (1993) Automated biopsy devices: a blinded evaluation. Radiology 187: 653-660
Midia M, Odedra D, Shuster A, Midea R, Muir J (2019) Predictors of bleeding complications following percutaneous image-guided liver biopsy: a scoping review. Diagn Interv Radiol 25: 71-80
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40: 373-383
Development Core Team (2017) R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria. Available from https://www.R-project.org
Karam AR, Nugent W, Khan A, Desai D, Shankar S (2010) Curved stylet core biopsy results in larger cores. AJR Am J Roentgenol 195: 242-244
Yuen HY, Lee Y, Bhatia K, Wong KT, Ahuja AT (2012) Use of end-cutting needles in ultrasound-guided biopsy of neck lesions. Eur Radiol 22: 832-836
Schaible J, Utpatel K, Verloh N, Pregler B, Zeman F, Wiggermann P, Schreyer AG, Stroszczynski C, Beyer LP (2020) Full-Core Biopsy Systems Take Larger Liver Tissue Samples with Lower Fragmentation Rates Than Conventional Side-Notch Systems: A Randomized Trial. Cancer Manag Res 12: 1121-1128
Hopper KD, Abendroth CS, Sturtz KW, Matthews YL, Hartzel JS, Potok PS (1995) CT percutaneous biopsy guns: comparison of end-cut and side-notch devices in cadaveric specimens. AJR Am J Roentgenol, 164: 195-199
Colloredo G, Guido M, Sonzogni A, Leandro G (2003) Impact of liver biopsy size on histological evaluation of chronic viral hepatitis: the smaller the sample, the milder the disease. J Hepatol 39: 239-244
Bedossa P, Dargere D, Paradis V (2003) Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology 38: 1449-1457
Boyum JH, Atwell TD, Wall DJ, Mansfield AS, Kerr SE, Gunderson TM, Rumilla KM, Weisbrod AJ, Kurup AN (2016) Incidence and Risk Factors for Adverse Events Related to Image-Guided Liver Biopsy. Mayo Clin Proc 91: 329-335
Atwell TD, Spanbauer JC, McMenomy BP, Stockland AH, Hesley GK, Schleck CD, Harmsen WS, Welch TJ (2015) The Timing and Presentation of Major Hemorrhage After 18,947 Image-Guided Percutaneous Biopsies. AJR Am J Roentgenol 205: 190-195
Padia SA, Baker ME, Schaeffer CJ, Remer EM, Obuchowski NA, Winans C, Herts BR (2009) Safety and efficacy of sonographic-guided random real-time core needle biopsy of the liver. J Clin Ultrasound 37: 138-143
Mueller M, Kratzer W, Oeztuerk S, Wilhelm M, Mason RA, Mao R, Haenle MM (2012) Percutaneous ultrasonographically guided liver punctures: an analysis of 1961 patients over a period of ten years. BMC Gastroenterol 12: 173
Constantin A, Brisson M, Kwan J, Proulx F (2010) Percutaneous US-guided renal biopsy: a retrospective study comparing the 16-gauge end-cut and 14-gauge side-notch needles. J Vasc Interv Radiol 21: 357-361
Ho LM, Pendse AA, Ronald J, Luciano M, Marin D, Jaffe TA, Nelson RC (2020) Ultrasound-guided non-targeted liver core biopsy: comparison of the efficacy of two different core needle biopsy systems using an ex-vivo animal model and retrospective review of clinical experience. Clin Imaging 61: 36-42
Fotiadis N, Paepe KN, Bonne L, et al. (2020) Comparison of a coaxial versus non-coaxial liver biopsy technique in an oncological setting: diagnostic yield, complications and seeding risk. Eur Radiol 30: 6702-6708
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Rendon C. Nelson—Research support from Bracco Diagnostics, Inc. Lisa M. Ho, Avani A. Pendse, James Ronald, Hemant Desai, Rui Dai, Cole Ziegler and Benjamin Wildman-Tobriner declares no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ho, L.M., Pendse, A.A., Ronald, J. et al. Comparison of clinical efficacy, subjective user experience, and safety for two different core biopsy needles, the Achieve® and Marquee®. Abdom Radiol 47, 2632–2639 (2022). https://doi.org/10.1007/s00261-021-03187-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-021-03187-5