Abstract
Purpose
To evaluate repeatability of ROI-sampling strategies for quantifying hepatic proton density fat fraction (PDFF) and to assess error relative to the 9-ROI PDFF.
Methods
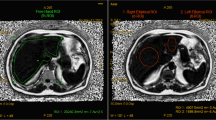
This was a secondary analysis in subjects with known or suspected nonalcoholic fatty liver disease who underwent MRI for magnitude-based hepatic PDFF quantification. Each subject underwent three exams, each including three acquisitions (nine acquisitions total). An ROI was placed in each hepatic segment on the first acquisition of the first exam and propagated to other acquisitions. PDFF was calculated for each of 511 sampling strategies using every combination of 1, 2, …, all 9 ROIs. Intra- and inter-exam intra-class correlation coefficients (ICCs) and repeatability coefficients (RCs) were estimated for each sampling strategy. Mean absolute error (MAE) was estimated relative to the 9-ROI PDFF. Strategies that sampled both lobes evenly (“balanced”) were compared with those that did not (“unbalanced”) using two-sample t tests.
Results
The 29 enrolled subjects (23 male, mean age 24 years) had mean 9-ROI PDFF 11.8% (1.1–36.3%). With more ROIs, ICCs increased, RCs decreased, and MAE decreased. Of the 60 balanced strategies with 4 ROIs, all (100%) achieved inter- and intra-exam ICCs > 0.998, 55 (92%) achieved intra-exam RC < 1%, 50 (83%) achieved inter-exam RC < 1%, and all (100%) achieved MAE < 1%. Balanced sampling strategies had higher ICCs and lower RCs, and lower MAEs than unbalanced strategies in aggregate (p < 0.001 for comparisons between balanced vs. unbalanced strategies).
Conclusion
Repeatability improves and error diminishes with more ROIs. Balanced 4-ROI strategies provide high repeatability and low error.






Similar content being viewed by others
References
Reeder SB, McKenzie CA, Pineda AR et al. (2007) Water–fat separation with IDEAL gradient-echo imaging. J Magn Reson Imaging 25:644–52. https://doi.org/10.1002/jmri.20831
Reeder SB and Sirlin CB (2010) Quantification of liver fat with magnetic resonance imaging. Magn Reson Imaging Clin N Am 18:337–57, ix. https://doi.org/10.1016/j.mric.2010.08.013
Reeder SB, Cruite I, Hamilton G and Sirlin CB (2011) Quantitative assessment of liver fat with magnetic resonance imaging and spectroscopy. J Magn Reson Imaging 34:729–49. https://doi.org/10.1002/jmri.22580
Reeder SB, Hu HH and Sirlin CB (2012) Proton density fat-fraction: a standardized MR-based biomarker of tissue fat concentration. J Magn Reson Imaging 36:1011–4. https://doi.org/10.1002/jmri.23741
Reeder SB, Pineda AR, Wen Z et al. (2005) Iterative decomposition of water and fat with echo asymmetry and least-squares estimation (IDEAL): Application with fast spin-echo imaging. Magn Reson Med 54:636–44. https://doi.org/10.1002/mrm.20624
Hong CW, Fazeli Dehkordy S, Hooker JC, Hamilton G and Sirlin CB (2017) Fat Quantification in the Abdomen. Top Magn Reson Imaging 26:221–7. https://doi.org/10.1097/RMR.0000000000000141
Yokoo T and Browning JD (2014) Fat and Iron Quantification in the Liver. Top Magn Reson Imaging 23:129–50. https://doi.org/10.1097/RMR.0000000000000016
Cassidy FH, Yokoo T, Aganovic L et al. (2009) Fatty Liver Disease: MR Imaging Techniques for the Detection and Quantification of Liver Steatosis. RadioGraphics Radiological Society of North America . 29:231–60. https://doi.org/10.1148/rg.291075123
İdilman İS, Haliloğlu M, Gümrük F and Karçaaltıncaba M (2016) The Feasibility of Magnetic Resonance Imaging for Quantification of Liver, Pancreas, Spleen, Vertebral Bone Marrow, and Renal Cortex R2* and Proton Density Fat Fraction in Transfusion-Related Iron Overload. Turkish J Hematol 33:21–7. https://doi.org/10.4274/tjh.2015.0142
Tang A, Desai A, Hamilton G et al. (2015) Accuracy of MR imaging-estimated proton density fat fraction for classification of dichotomized histologic steatosis grades in nonalcoholic fatty liver disease. Radiology 274:416–25. https://doi.org/10.1148/radiol.14140754
Tyagi A, Yeganeh O, Levin Y et al. (2015) Intra- and inter-examination repeatability of magnetic resonance spectroscopy, magnitude-based MRI, and complex-based MRI for estimation of hepatic proton density fat fraction in overweight and obese children and adults. Abdom Imaging 40:3070–7. https://doi.org/10.1007/s00261-015-0542-5
Bonekamp S, Tang A, Mashhood A et al. (2014) Spatial distribution of MRI-Determined hepatic proton density fat fraction in adults with nonalcoholic fatty liver disease. J Magn Reson Imaging 39:1525–32.
Larson SP, Bowers SP, Palekar NA et al. (2007) Histopathologic variability between the right and left lobes of the liver in morbidly obese patients undergoing Roux-en-Y bypass. Clin Gastroenterol Hepatol 5:1329–32. https://doi.org/10.1016/j.cgh.2007.06.005
Merriman RB, Ferrell LD, Patti MG et al. (2006) Correlation of paired liver biopsies in morbidly obese patients with suspected nonalcoholic fatty liver disease. Hepatology 44:874–80. https://doi.org/10.1002/hep.21346
Vu K-N, Gilbert G, Chalut M et al. (2016) MRI-determined liver proton density fat fraction, with MRS validation: Comparison of regions of interest sampling methods in patients with type 2 diabetes. J Magn Reson Imaging 43:1090–9. https://doi.org/10.1002/jmri.25083
Cui J, Philo L, Nguyen P et al. (2016) Sitagliptin vs. placebo for non-alcoholic fatty liver disease: A randomized controlled trial. J Hepatol 65:369–76. https://doi.org/10.1016/j.jhep.2016.04.021
Middleton MS, Heba ER, Hooker CA et al. (2017) Agreement Between Magnetic Resonance Imaging Proton Density Fat Fraction Measurements and Pathologist-Assigned Steatosis Grades of Liver Biopsies From Adults With Nonalcoholic Steatohepatitis. Gastroenterology W.B. Saunders. 153:753–61. https://doi.org/10.1053/j.gastro.2017.06.005
Loomba R, Sirlin CB, Ang B et al. (2015) Ezetimibe for the treatment of nonalcoholic steatohepatitis: assessment by novel magnetic resonance imaging and magnetic resonance elastography in a randomized trial (MOZART trial). Hepatology 61:1239–50. https://doi.org/10.1002/hep.27647
Fazeli Dehkordy S, Fowler KJ, Mamidipalli A et al. (2018) Hepatic steatosis and reduction in steatosis following bariatric weight loss surgery differs between segments and lobes. Eur Radiol. https://doi.org/10.1007/s00330-018-5894-0
Le T-A, Chen J, Changchien C et al. (2012) Effect of colesevelam on liver fat quantified by magnetic resonance in nonalcoholic steatohepatitis: a randomized controlled trial. Hepatology 56:922–32. https://doi.org/10.1002/hep.25731
Permutt Z, Le TA, Peterson MR et al. (2012) Correlation between liver histology and novel magnetic resonance imaging in adult patients with non-alcoholic fatty liver disease - MRI accurately quantifies hepatic steatosis in NAFLD. Aliment Pharmacol Ther. https://doi.org/10.1111/j.1365-2036.2012.05121.x
Tang A, Tan J, Sun M et al. (2013) Nonalcoholic fatty liver disease: MR imaging of liver proton density fat fraction to assess hepatic steatosis. Radiology 267:422–31. https://doi.org/10.1148/radiol.12120896
Hong CW, Wolfson T, Sy EZ et al. (2018) Optimization of region-of-interest sampling strategies for hepatic MRI proton density fat fraction quantification. J Magn Reson Imaging 47:988–94. https://doi.org/10.1002/jmri.25843
Negrete LM, Middleton MS, Clark L et al. (2014) Inter-examination precision of magnitude-based MRI for estimation of segmental hepatic proton density fat fraction in obese subjects. J Magn Reson Imaging 39:1265–71. https://doi.org/10.1002/jmri.24284
Yokoo T, Bydder M, Hamilton G et al. (2009) Nonalcoholic fatty liver disease: diagnostic and fat-grading accuracy of low-flip-angle multiecho gradient-recalled-echo MR imaging at 1.5 T. Radiology 251:67–76. https://doi.org/10.1148/radiol.2511080666
Yokoo T, Shiehmorteza M, Hamilton G et al. (2011) Estimation of hepatic proton-density fat fraction by using MR imaging at 3.0 T. Radiology 258:749–59. https://doi.org/10.1148/radiol.10100659
Kühn J-P, Hernando D, Mensel B et al. (2014) Quantitative chemical shift-encoded MRI is an accurate method to quantify hepatic steatosis. J Magn Reson Imaging 39:1494–501. https://doi.org/10.1002/jmri.24289
Bydder M, Yokoo T, Hamilton G et al. (2008) Relaxation effects in the quantification of fat using gradient echo imaging. Magn Reson Imaging 26:347–59. https://doi.org/10.1016/j.mri.2007.08.012
Hamilton G, Schlein AN, Middleton MS et al. (2016) In vivo triglyceride composition of abdominal adipose tissue measured by (1) H MRS at 3T. J Magn Reson Imaging. https://doi.org/10.1002/jmri.25453
Hernando D, Hines CDG, Yu H and Reeder SB (2012) Addressing phase errors in fat-water imaging using a mixed magnitude/complex fitting method. Magn Reson Med NIH Public Access. 67:638–44. https://doi.org/10.1002/mrm.23044
Yu H, Shimakawa A, Hines CDG et al. (2011) Combination of complex-based and magnitude-based multiecho water-fat separation for accurate quantification of fat-fraction. Magn Reson Med 66:199–206. https://doi.org/10.1002/mrm.22840
Raunig DL, McShane LM, Pennello G et al. (2015) Quantitative imaging biomarkers: a review of statistical methods for technical performance assessment. Stat Methods Med Res 24:27–67. https://doi.org/10.1177/0962280214537344
Neyman J and Scott EL (1948) Consistent Estimates Based on Partially Consistent Observations. Econometrica JSTOR. 16:1. https://doi.org/10.2307/1914288
Campo CA, Hernando D, Schubert T et al. (2017) Standardized Approach for ROI-Based Measurements of Proton Density Fat Fraction and R2* in the Liver. Am J Roentgenol 209:592–603. https://doi.org/10.2214/AJR.17.17812
Hooker JC, Hamilton G, Park CC et al. (2018) Inter-reader agreement of magnetic resonance imaging proton density fat fraction and its longitudinal change in a clinical trial of adults with nonalcoholic steatohepatitis. Abdom Radiol. https://doi.org/10.1007/s00261-018-1745-3
Wang K, Mamidipalli A, Retson T et al. (2019) Automated CT and MRI Liver Segmentation and Biometry Using a Generalized Convolutional Neural Network. Radiol Artif Intell Radiological Society of North America (RSNA). 1:180022. https://doi.org/10.1148/ryai.2019180022
Acknowledgements
The authors would like to acknowledge grant support from the National Institutes of Health T32 EB005970-09 and R01 DK106419-02. We also acknowledge Gilead Sciences and GE Healthcare which provide research support to UCSD.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hong, C.W., Cui, J.Y., Batakis, D. et al. Repeatability and accuracy of various region-of-interest sampling strategies for hepatic MRI proton density fat fraction quantification. Abdom Radiol 46, 3105–3116 (2021). https://doi.org/10.1007/s00261-021-02965-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-021-02965-5