Abstract
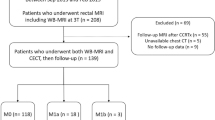
A T1 sequence on routine baseline staging rectal magnetic resonance imaging (MRI) is thought to help detect bone lesions. Our primary aim was to evaluate the incidence of bone lesions encountered on baseline staging rectal MRI, particularly the prevalence of bone metastases. This retrospective study included patients with rectal adenocarcinoma who underwent baseline rectal MRI at our institution between January 2010 and December 2017. The MRI report was reviewed for presence of bone lesions. When found, lesion type, presence of axial T1 non-fat-suppressed sequence, primary tumor T-stage, and presence of other organ metastases were recorded. In the absence of bone biopsy, the reference standard was follow-up imaging via computed tomography (CT), MRI, and/or positron emission tomography/CT (PET/CT) ≥ 1 year after the baseline MRI. The Wilcoxon rank-sum test and Fisher's exact test were used to compare clinicopathologic data of patients with malignant or benign bone lesions. A total of 1197 patients were included. 62/1197 patients (mean age 56.8 years (SD: 13.8), with 39 men) had bone lesions on baseline imaging, with 6 being bone metastases (0.5%, 95% CI 0.2%–1.1%). Of the 6 patients with bone metastases, 5/6 had other metastases (i.e., liver, lung) at baseline. Bone metastases on baseline rectal MRI performed for rectal adenocarcinoma are extremely rare. Furthermore, bone metastases without other organ (i.e., liver, lung) involvement is extremely rare.






Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Change history
20 March 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00261-021-03012-z
References
Meyer JE, Narang T, Schnoll-Sussman FH, Pochapin MB, Christos PJ, Sherr DL (2010) Increasing incidence of rectal cancer in patients aged younger than 40 years: an analysis of the surveillance, epidemiology, and end results database. Cancer 116 (18):4354-4359. https://doi.org/10.1002/cncr.25432
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68 (6):394-424. https://doi.org/10.3322/caac.21492
Ferlay J, Parkin DM, Steliarova-Foucher E (2010) Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer 46 (4):765-781. https://doi.org/10.1016/j.ejca.2009.12.014
Sahni VA, Silveira PC, Sainani NI, Khorasani R (2015) Impact of a Structured Report Template on the Quality of MRI Reports for Rectal Cancer Staging. AJR Am J Roentgenol 205 (3):584-588. https://doi.org/10.2214/AJR.14.14053
Norenberg D, Sommer WH, Thasler W, D'Haese J, Rentsch M, Kolben T, Schreyer A, Rist C, Reiser M, Armbruster M (2017) Structured Reporting of Rectal Magnetic Resonance Imaging in Suspected Primary Rectal Cancer: Potential Benefits for Surgical Planning and Interdisciplinary Communication. Invest Radiol 52 (4):232-239. https://doi.org/10.1097/RLI.0000000000000336
Gollub MJ, Arya S, Beets-Tan RG, dePrisco G, Gonen M, Jhaveri K, Kassam Z, Kaur H, Kim D, Knezevic A, Korngold E, Lall C, Lalwani N, Blair Macdonald D, Moreno C, Nougaret S, Pickhardt P, Sheedy S, Harisinghani M (2018) Use of magnetic resonance imaging in rectal cancer patients: Society of Abdominal Radiology (SAR) rectal cancer disease-focused panel (DFP) recommendations 2017. Abdom Radiol (NY) 43 (11):2893-2902. https://doi.org/10.1007/s00261-018-1642-9
Beets-Tan RGH, Lambregts DMJ, Maas M, Bipat S, Barbaro B, Curvo-Semedo L, Fenlon HM, Gollub MJ, Gourtsoyianni S, Halligan S, Hoeffel C, Kim SH, Laghi A, Maier A, Rafaelsen SR, Stoker J, Taylor SA, Torkzad MR, Blomqvist L (2018) Magnetic resonance imaging for clinical management of rectal cancer: Updated recommendations from the 2016 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol 28 (4):1465-1475. https://doi.org/10.1007/s00330-017-5026-2
NCCN Guidelines for Patients®: Rectal Cancer (2018) National Comprehensive Cancer Network. Rectal Cancer (Version 2.2018). https://www.nccn.org/patients/guidelines/content/PDF/rectal-patient.pdf. Accessed April 11 2020
Disibio G, French SW (2008) Metastatic patterns of cancers: results from a large autopsy study. Arch Pathol Lab Med 132 (6):931-939. https://doi.org/10.1043/1543-2165(2008)132[931:MPOCRF]2.0.CO;2
Hess KR, Varadhachary GR, Taylor SH, Wei W, Raber MN, Lenzi R, Abbruzzese JL (2006) Metastatic patterns in adenocarcinoma. Cancer 106 (7):1624-1633. https://doi.org/10.1002/cncr.21778
Weiss L, Grundmann E, Torhorst J, Hartveit F, Moberg I, Eder M, Fenoglio-Preiser CM, Napier J, Horne CH, Lopez MJ, et al. (1986) Haematogenous metastatic patterns in colonic carcinoma: an analysis of 1541 necropsies. J Pathol 150 (3):195-203. https://doi.org/10.1002/path.1711500308
Baek SJ, Hur H, Min BS, Baik SH, Lee KY, Kim NK (2016) The Characteristics of Bone Metastasis in Patients with Colorectal Cancer: A Long-Term Report from a Single Institution. World J Surg 40 (4):982-986. https://doi.org/10.1007/s00268-015-3296-x
Roth ES, Fetzer DT, Barron BJ, Joseph UA, Gayed IW, Wan DQ (2009) Does colon cancer ever metastasize to bone first? a temporal analysis of colorectal cancer progression. BMC Cancer 9:274. https://doi.org/10.1186/1471-2407-9-274
Katoh M, Unakami M, Hara M, Fukuchi S (1995) Bone metastasis from colorectal cancer in autopsy cases. J Gastroenterol 30 (5):615-618. https://doi.org/10.1007/BF02367787
Kanthan R, Loewy J, Kanthan SC (1999) Skeletal metastases in colorectal carcinomas: a Saskatchewan profile. Dis Colon Rectum 42 (12):1592-1597. https://doi.org/10.1007/BF02236213
Hwang S, Panicek DM (2007) Magnetic resonance imaging of bone marrow in oncology, Part 1. Skeletal Radiol 36 (10):913-920. https://doi.org/10.1007/s00256-007-0309-3
Bernard S, Walker E, Raghavan M (2017) An Approach to the Evaluation of Incidentally Identified Bone Lesions Encountered on Imaging Studies. AJR Am J Roentgenol 208 (5):960-970. https://doi.org/10.2214/AJR.16.17434
Schweitzer ME LC, Mitchell DG, Gannon FH, Gomella LG. (1993) Bull’s-eyes and halos: useful MR discriminators of osseous metastases. Radiology 188:249-252
Ghazizadeh S, Foss EW, Didier R, Fung A, Panicek DM, Coakley FV (2014) Musculoskeletal pitfalls and pseudotumours in the pelvis: a pictorial review for body imagers. Br J Radiol 87 (1042):20140243. https://doi.org/10.1259/bjr.20140243
Simpfendorfer CS, Ilaslan H, Davies AM, James SL, Obuchowski NA, Sundaram M (2008) Does the presence of focal normal marrow fat signal within a tumor on MRI exclude malignancy? An analysis of 184 histologically proven tumors of the pelvic and appendicular skeleton. Skeletal Radiol 37 (9):797-804. https://doi.org/10.1007/s00256-008-0523-7
Nascimento D, Suchard G, Hatem M, de Abreu A (2014) The role of magnetic resonance imaging in the evaluation of bone tumours and tumour-like lesions. Insights Imaging 5 (4):419-440. https://doi.org/10.1007/s13244-014-0339-z
Bangera S, Dunkow P, Weerasinghe S, Murugesan SV (2016) An unusual pain in the hip. Oxf Med Case Reports 2016 (9):omw072. https://doi.org/10.1093/omcr/omw072
Udare A, Sable N, Kumar R, Thakur M, Juvekar S (2015) Solitary osseous metastasis of rectal carcinoma masquerading as osteogenic sarcoma on post-chemotherapy imaging: a case report. Korean J Radiol 16 (1):175-179. https://doi.org/10.3348/kjr.2015.16.1.175
Chalkidou AS, Boutis AL, Padelis P (2009) Management of a Solitary Bone Metastasis to the Tibia from Colorectal Cancer. Case Rep Gastroenterol 3 (3):354-359. https://doi.org/10.1159/000239626
Expert Panel on Gastrointestinal I, Fowler KJ, Kaur H, Cash BD, Feig BW, Gage KL, Garcia EM, Hara AK, Herman JM, Kim DH, Lambert DL, Levy AD, Peterson CM, Scheirey CD, Small W, Jr., Smith MP, Lalani T, Carucci LR (2017) ACR Appropriateness Criteria((R)) Pretreatment Staging of Colorectal Cancer. J Am Coll Radiol 14 (5S):S234-S244. https://doi.org/10.1016/j.jacr.2017.02.012
Horvat N, Hope TA, Pickhardt PJ, Petkovska I (2019) Mucinous rectal cancer: concepts and imaging challenges. Abdom Radiol (NY) 44 (11):3569-3580. https://doi.org/10.1007/s00261-019-02019-x
Acknowledgments
The authors thank Joanne Chin, MFA, ELS, for editorial support and Natalie Gangai for assistance on this article.
Funding
This research was funded in part by the NIH/NCI Cancer Center Support Grant P30 CA008748.
Author information
Authors and Affiliations
Contributions
Conceptualization: JG, MG, IP, JL. Data curation: JL. Investigation: JL. Methodology: JL, JL, JG, IP, MG, MC, JZ. Formal analysis: JL, JG, MC, JZ. Project administration: JL, JG. Resources: N/A. Supervision: JG, IP. Visualization: JL, JG. Writing—original draft: JL. Writing—review & editing: JG, IP, MG, VP, DB, MC, JZ, LF.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee institutional review board at Memorial Sloan Kettering cancer Center and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Levine, J., Petkovska, I., Landa, J. et al. Bone lesions on baseline staging rectal MRI: prevalence and significance in patients with rectal adenocarcinoma. Abdom Radiol 46, 2423–2431 (2021). https://doi.org/10.1007/s00261-020-02923-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02923-7