Abstract
Purpose
In patients presenting with blunt hepatic injury (BHI), the utility of CT for triage to hepatic angiography remains uncertain since simple binary assessment of contrast extravasation (CE) as being present or absent has only modest accuracy for major arterial injury on digital subtraction angiography (DSA). American Association for the Surgery of Trauma (AAST) liver injury grading is coarse and subjective, with limited diagnostic utility in this setting. Volumetric measurements of hepatic injury burden could improve prediction. We hypothesized that in a cohort of patients that underwent catheter-directed hepatic angiography following admission trauma CT, a deep learning quantitative visualization method that calculates % liver parenchymal disruption (the LPD index, or LPDI) would add value to CE assessment for prediction of major hepatic arterial injury (MHAI).
Methods
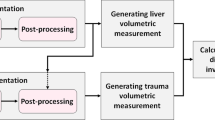
This retrospective study included adult patients with BHI between 1/1/2008 and 5/1/2017 from two institutions that underwent admission trauma CT prior to hepatic angiography (n = 73). Presence (n = 41) or absence (n = 32) of MHAI (pseudoaneurysm, AVF, or active contrast extravasation on DSA) served as the outcome. Voxelwise measurements of liver laceration were derived using an existing multiscale deep learning algorithm trained on manually labeled data using cross-validation with a 75–25% split in four unseen folds. Liver volume was derived using a pre-trained whole liver segmentation algorithm. LPDI was automatically calculated for each patient by determining the percentage of liver involved by laceration. Classification and regression tree (CART) analyses were performed using a combination of automated LPDI measurements and either manually segmented CE volumes, or CE as a binary sign. Performance metrics for the decision rules were compared for significant differences with binary CE alone (the current standard of care for predicting MHAI), and the AAST grade.
Results
36% of patients (n = 26) had contrast extravasation on CT. Median [Q1–Q3] automated LPDI was 4.0% [1.0–12.1%]. 41/73 (56%) of patients had MHAI. A decision tree based on auto-LPDI and volumetric CE measurements (CEvol) had the highest accuracy (0.84, 95% CI 0.73–0.91) with significant improvement over binary CE assessment (0.68, 95% CI 0.57–0.79; p = 0.01). AAST grades at different cut-offs performed poorly for predicting MHAI, with accuracies ranging from 0.44–0.63. Decision tree analysis suggests an auto-LPDI cut-off of ≥ 12% for minimizing false negative CT exams when CE is absent or diminutive.
Conclusion
Current CT imaging paradigms are coarse, subjective, and limited for predicting which BHIs are most likely to benefit from AE. LPDI, automated using deep learning methods, may improve objective personalized triage of BHI patients to angiography at the point of care.


Similar content being viewed by others
References
Matthes G, Stengel D, Seifert J, Rademacher G, Mutze S, Ekkernkamp A. Blunt liver injuries in polytrauma: results from a cohort study with the regular use of whole-body helical computed tomography. World journal of surgery. 2003;27(10):1124-30.
Dreizin D, Munera F. Blunt polytrauma: evaluation with 64-section whole-body CT angiography. Radiographics. 2012;32(3):609-31.
Kozar RA, Feliciano DV, Moore EE, Moore FA, Cocanour CS, West MA, Davis JW, McIntyre Jr RC. Western Trauma Association/critical decisions in trauma: operative management of adult blunt hepatic trauma. Journal of Trauma and Acute Care Surgery. 2011;71(1):1-5.
Kutcher ME, Weis JJ, Siada SS, Kaups KL, Kozar RA, Wawrose RA, Summers JI, Eriksson EA, Leon SM, Carrick MM. The role of computed tomographic scan in ongoing triage of operative hepatic trauma: A Western Trauma Association multicenter retrospective study. Journal of Trauma and Acute Care Surgery. 2015;79(6):951-6.
Letoublon C, Morra I, Chen Y, Monnin V, Voirin D, Arvieux C. Hepatic arterial embolization in the management of blunt hepatic trauma: indications and complications. Journal of Trauma and Acute Care Surgery. 2011;70(5):1032-7.
Fang J-F, Chen R-J, Wong Y-C, Lin B-C, Hsu Y-B, Kao J-L, Chen M-F. Classification and treatment of pooling of contrast material on computed tomographic scan of blunt hepatic trauma. Journal of Trauma and Acute Care Surgery. 2000;49(6):1083-8.
Coccolini F, Catena F, Moore EE, Ivatury R, Biffl W, Peitzman A, Coimbra R, Rizoli S, Kluger Y, Abu-Zidan FM. WSES classification and guidelines for liver trauma. World Journal of Emergency Surgery. 2016;11(1):50.
Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: spleen and liver (1994 revision). Journal of Trauma and Acute Care Surgery. 1995;38(3):323-4.
Coccolini F, Montori G, Catena F, Di Saverio S, Biffl W, Moore EE, Peitzman AB, Rizoli S, Tugnoli G, Sartelli M. Liver trauma: WSES position paper. World Journal of Emergency Surgery. 2015;10(1):39.
Mohr AM, Lavery RF, Barone A, Bahramipour P, Magnotti LJ, Osband AJ, Sifri Z, Livingston DH. Angiographic embolization for liver injuries: low mortality, high morbidity. Journal of Trauma and Acute Care Surgery. 2003;55(6):1077-82.
Bala M, Gazalla SA, Faroja M, Bloom AI, Zamir G, Rivkind AI, Almogy G. Complications of high grade liver injuries: management and outcomewith focus on bile leaks. Scandinavian journal of trauma, resuscitation and emergency medicine. 2012;20(1):20.
Dabbs DN, Stein DM, Scalea TM. Major hepatic necrosis: a common complication after angioembolization for treatment of high-grade liver injuries. Journal of Trauma and Acute Care Surgery. 2009;66(3):621-9.
Patil S, Udupi V. Preprocessing to be considered for MR and CT images containing tumors. IOSR journal of electrical and electronics engineering. 2012;1(4):54-7.
Zhou Y, Li Z, Bai S, Wang C, Chen X, Han M, Fishman E, Yuille AL, editors. Prior-aware neural network for partially-supervised multi-organ segmentation. Proceedings of the IEEE International Conference on Computer Vision; 2019.
Zhou Y, Dreizin D, Li Y, Zhang Z, Wang Y, Yuille A, editors. Multi-Scale Attentional Network for multi-focal segmentation of active bleed after pelvic fractures. International Workshop on Machine Learning in Medical Imaging; 2019: Springer.
Dreizin D, Zhou Y, Fu S, Wang Y, Li G, Champ K, Siegel E, Wang Z, Chen T, Yuille AL. A Multiscale Deep Learning Method for Quantitative Visualization of Traumatic Hemoperitoneum at CT: Assessment of Feasibility and Comparison with Subjective Categorical Estimation. Radiology: Artificial Intelligence. 2020;2(6):e190220.
Chen L-C, Papandreou G, Kokkinos I, Murphy K, Yuille AL. Deeplab: Semantic image segmentation with deep convolutional nets, atrous convolution, and fully connected crfs. IEEE transactions on pattern analysis and machine intelligence. 2017;40(4):834-48.
Zhou Y, Dreizin D, Li Y, Zhang Z, Wang Y, Yuille A. Multi-Scale Attentional Network for Multi-Focal Segmentation of Active Bleed after Pelvic Fractures. arXiv preprint arXiv:190609540. 2019.
Chartrand G, Cheng PM, Vorontsov E, Drozdzal M, Turcotte S, Pal CJ, Kadoury S, Tang A. Deep learning: a primer for radiologists. Radiographics. 2017;37(7):2113-31.
Zou KH, Tuncali K, Silverman SG. Correlation and simple linear regression. Radiology. 2003;227(3):617-28.
Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological assessment. 1994;6(4):284.
Breiman L, Friedman J, Olshen R, Stone C. Classification and regression trees. Wadsworth & Brooks. Cole Statistics/Probability Series. 1984.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988:837–45.
Zou KH, Warfield SK, Bharatha A, Tempany CM, Kaus MR, Haker SJ, Wells III WM, Jolesz FA, Kikinis R. Statistical validation of image segmentation quality based on a spatial overlap index1: scientific reports. Academic radiology. 2004;11(2):178-89.
Costantini TW, Coimbra R, Holcomb JB, Podbielski JM, Catalano R, Blackburn A, Scalea TM, Stein DM, Williams L, Conflitti J. Current management of hemorrhage from severe pelvic fractures: results of an American Association for the Surgery of Trauma multi-institutional trial. Journal of Trauma and Acute Care Surgery. 2016;80(5):717-25.
Dreizin D, Bodanapally UK, Munera F. MDCT of complications and common postoperative findings following penetrating torso trauma. Emergency radiology. 2015;22(5):553-63.
Becker CD, Gal I, Baer HU, Vock P. Blunt hepatic trauma in adults: correlation of CT injury grading with outcome. Radiology. 1996;201(1):215-20.
Dreizin D, Bodanapally U, Boscak A, Tirada N, Issa G, Nascone JW, Bivona L, Mascarenhas D, O’Toole RV, Nixon E. CT prediction model for major arterial injury after blunt pelvic ring disruption. Radiology. 2018;287(3):1061-9.
Dreizin D, Bodanapally UK, Neerchal N, Tirada N, Patlas M, Herskovits E. Volumetric analysis of pelvic hematomas after blunt trauma using semi-automated seeded region growing segmentation: a method validation study. Abdominal Radiology. 2016;41(11):2203-8.
Miller PR, Croce MA, Bee TK, Qaisi WG, Smith CP, Collins GL, Fabian TC. ARDS after pulmonary contusion: accurate measurement of contusion volume identifies high-risk patients. Journal of Trauma and Acute Care Surgery. 2001;51(2):223-30.
Yoon W, Jeong YY, Kim JK, Seo JJ, Lim HS, Shin SS, Kim JC, Jeong SW, Park JG, Kang HK. CT in blunt liver trauma. Radiographics. 2005;25(1):87-104.
Dreizin D, Zhou Y, Zhang Y, Tirada N, Yuille AL. Performance of a Deep Learning Algorithm for Automated Segmentation and Quantification of Traumatic Pelvic Hematomas on CT. Journal of digital imaging. 2019:1–9.
Christ PF, Elshaer MEA, Ettlinger F, Tatavarty S, Bickel M, Bilic P, Rempfler M, Armbruster M, Hofmann F, D’Anastasi M, editors. Automatic liver and lesion segmentation in CT using cascaded fully convolutional neural networks and 3D conditional random fields. International Conference on Medical Image Computing and Computer-Assisted Intervention; 2016: Springer.
Kozar RA, Crandall M, Shanmuganathan K, Zarzaur BL, Coburn M, Cribari C, Kaups K, Schuster K, Tominaga GT, Committee tAPA. Organ injury scaling 2018 update: Spleen, liver, and kidney. Journal of Trauma and Acute Care Surgery. 2018;85(6):1119–22.
Fang J-F, Wong Y-C, Lin B-C, Hsu Y-P, Chen M-F. The CT risk factors for the need of operative treatment in initially hemodynamically stable patients after blunt hepatic trauma. Journal of Trauma and Acute Care Surgery. 2006;61(3):547-54.
Battey TW, Dreizin D, Bodanapally UK, Wnorowski A, Issa G, Iacco A, Chiu W. A comparison of segmented abdominopelvic fluid volumes with conventional CT signs of abdominal compartment syndrome in a trauma population. Abdominal Radiology. 2019:1–8.
Funding
NIBIB NIH K08 EB027141-01A1 (PI: David Dreizin, MD). Accelerated Translational Incubator Pilot (ATIP) award, University of Maryland (PI: David Dreizin, MD). RSNA medical student research grant (Tina Chen).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
David Dreizin is co-founder of TraumaVisual, LLC.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dreizin, D., Chen, T., Liang, Y. et al. Added value of deep learning-based liver parenchymal CT volumetry for predicting major arterial injury after blunt hepatic trauma: a decision tree analysis. Abdom Radiol 46, 2556–2566 (2021). https://doi.org/10.1007/s00261-020-02892-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02892-x