Abstract
Purpose
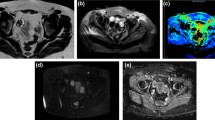
To determine if the presence of a dark cortical rim around the ovary on magnetic resonance imaging (MRI) is associated with polycystic ovarian syndrome (PCOS).
Materials and methods
This retrospective study included 52 PCOS patients with 98 total ovaries and 52 age-matched controls with 104 total ovaries. The ovaries were evaluated on MRI with at least two orthogonal views on T2-weighted sequences. Ovarian volume and follicular count per ovary were measured. Each ovary was also assessed for a dark cortical rim around the ovary on T2-weighted imaging which involved equal to or more than 50% of the ovarian circumference. The degree of rim continuity was classified as continuous if the rim involved greater than 75% of the ovarian circumference, discontinuous if 50–75% of the ovarian circumference was covered, or absent if less than 50% of the ovarian circumference was involved. The rim thickness was measured if present. T test and χ2 tests were performed to compare continuous and categorical variables, correspondingly, between cases and controls. ROC curves and area under the curve (AUC) were used to assess predictive performance and DeLong’s paired test was used to compare AUCs.
Results
A higher percentage of PCOS patients exhibited a continuous cortical rim about the ovary (71%) and a lower percentage of an absent cortical rim (8%) compared to controls (25% and 37%, respectively) (p < 0.001). A continuous cortical ovarian rim has a sensitivity and specificity of 71% and 75%, respectively, for diagnosing PCOS. Mean cortical rim thickness is significantly higher in the PCOS group (1.4 mm) compared with controls (0.8 mm) (p < 0.001). Cortical rim thickness and presence of a continuous cortical rim are strongly correlated. Cortical rim thickness of 1.2 mm provides a sensitivity and specificity of 75% and 60%, correspondingly, for a diagnosis of PCOS. Cortical rim thickness combined with cortical rim continuity has an AUC of 0.77 for diagnosing PCOS, which is similar to conventional imaging features of ovarian volume and follicular count combined.
Conclusion
A dark cortical rim around the ovary is an MRI feature that can be used to support a diagnosis of PCOS.






Similar content being viewed by others
Data availability
The original data are available with the senior author (KSL).
References
Azziz R, Woods KS, Reyna R, et al (2004) The prevalence and features of the polycystic ovary syndrome in an unselected population. J Clin Endocrinol Metab 89:2745–2749. https://doi.org/10.1210/jc.2003-032046
Ibáñez L, Oberfield SE, Witchel S, et al (2017) An International Consortium Update: Pathophysiology, Diagnosis, and Treatment of Polycystic Ovarian Syndrome in Adolescence. Horm Res Paediatr 88:371–395. https://doi.org/10.1159/000479371
Daniilidis A, Dinas K (2009) Long term health consequences of polycystic ovarian syndrome: a review analysis. Hippokratia 13:90–2
Goodman NF, Cobin RH, Futterweit W, et al (2015) American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and Pcos Society Disease State Clinical Review: Guide To the Best Practices in the Evaluation and Treatment of Polycystic Ovary Syndrome - Part 1. Endocr Pract 21:1291–1300. https://doi.org/10.4158/EP15748.DSC
Dewailly D, Lujan ME, Carmina E, et al (2014) Definition and significance of polycystic ovarian morphology: A task force report from the androgen excess and polycystic ovary syndrome society. Hum Reprod Update 20:334–352. https://doi.org/10.1093/humupd/dmt061
Balen AH, Laven JSE, Tan SL, Dewailly D (2003) Ultrasound assessment of the polycystic ovary: International consensus definitions. Hum Reprod Update 9:505–514. https://doi.org/10.1093/humupd/dmg044
Fauser BCJM (2004) Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril 81:19–25. https://doi.org/10.1016/j.fertnstert.2003.10.004
Randeva HS, Tan BK, Weickert MO, et al (2012) Cardiometabolic aspects of the polycystic ovary syndrome. Endocr Rev 33:812–841. https://doi.org/10.1210/er.2012-1003
Mitchell DG, Gefter WB, Spritzer CE, et al (1986) Polycystic ovaries: MR imaging. Radiology 160:425–42. https://doi.org/10.1148/radiology.160.2.3726121
Yoo RY, Sirlin CB, Gottschalk M, Chang RJ (2005) Ovarian imaging by magnetic resonance in obese adolescent girls with polycystic ovary syndrome: A pilot study. Fertil Steril 84:985–995. https://doi.org/10.1016/j.fertnstert.2005.04.039
Fondin M, Rachas A, Huynh V, et al (2017) Polycystic ovary syndrome in adolescents: Which MR Imaging–based Diagnostic Criteria? Radiology 285:961–970. https://doi.org/10.1016/j.bpobgyn.2017.08.008
Kenigsberg L, Agarwal C, Sin S, et al (2015) Clinical Utility of Magnetic Resonance Imaging (MRI) and Ultrasonography (US) for Diagnosis of Polycystic Ovary Syndrome (PCOS) in Adolescent Girls. Fertil Steril 104:1302–1309. https://doi.org/10.1002/jmri.23741.Proton
Lunde O, Hoel PS, Sandvik L (1988) Ovarian morphology in patients with polycystic ovaries and in an age-matched reference material: A statistical evaluation of 149 cases. Gynecol Obstet Invest 25:192–201. https://doi.org/10.1159/000293771
Hughesdon PE (1982) Morphology and Morphogenesis of Stein-Leventhal Ovary and of So-called “Hypethecosis.” Obstet Gynecol Surv 37:52–77
Gyves MT (1970) The Significance of Peripheral Sclerosis in the Stein-Leventhal Syndrome**Work done during a 4th year student elective in Obstetric and Gynecologic Pathology. Fertil Steril 21:502–507. https://doi.org/10.1016/S0015-0282(16)37566-5
Shinagare AB, Meylaerts LJ, Laury AR, Mortele KJ (2012) MRI features of ovarian fibroma and fibrothecoma with histopathologic correlation. Am J Roentgenol 198:296–303. https://doi.org/10.2214/AJR.11.7221
Maubon A, Courtieu C, Vivens F, et al (1993) Magnetic Resonance Imaging of Normal and Polycystic Ovaries. Ann Newe York Acad Sci 687:224–229. https://doi.org/10.1111/j.1600-0714.2007.00540.x
Umehara T, Richards JAS, Shimada M (2018) The stromal fibrosis in aging ovary. Aging (Albany NY) 10:9–10. https://doi.org/10.18632/aging.101370
Bazot M, Robert Y, Mestdagh P, et al (2000) Ovarian functional disorders. J Radiol 81:1801–18
Funding
This manuscript is not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Badeeb, A., Brook, A. & Lee, K.S. Dark cortical rim: an MRI feature of polycystic ovarian syndrome. Abdom Radiol 46, 1148–1156 (2021). https://doi.org/10.1007/s00261-020-02749-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02749-3