Abstract
Purpose
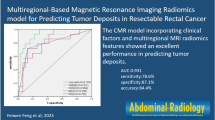
To establish and validate two predictive radiomics models for preoperative prediction of lymph node metastases (LNMs) and tumor deposits (TDs) respectively in rectal cancer (RC) patients.
Methods
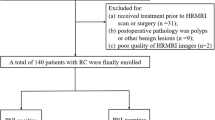
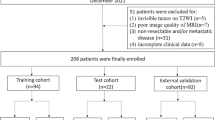
A total of 139 RC patients (98 in the training cohort and 41 in the validation cohort) were enrolled in the present study. High-resolution magnetic resonance images (HRMRI) were retrieved for tumor segmentation and feature extraction. HRMRI findings of RC were assessed by three experienced radiologists. Two radiomics nomograms were established by integrating the clinical risk factors, HRMRI findings and radiomics signature.
Results
The predictive nomogram of LNMs showed good predictive performance (area under the curve [AUC], 0.90; 95% confidence interval [CI] 0.83–0.96) which was better than clinico-radiological (AUC, 0.83; 95% CI 0.74–0.93; Delong test, p = 0.017) or radiomics signature-only model (AUC, 0.77; 95% CI 0.67–0.86; Delong test, p = 0.003) in training cohort. Application of the nomogram in the validation cohort still exhibited good performance (AUC, 0.87; 95% CI 0.76–0.98). The accuracy, sensitivity and specificity of the combined model in predicting LNMs was 0.86,0.79 and 0.91 in training cohort and 0.83,0.85 and 0.82 in validation cohort. As for TDs, the predictive efficacy of the nomogram (AUC, 0.82; 95% CI 0.71–0.93) was not significantly higher than radiomics signature-only model (AUC, 0.80; 95% CI 0.69–0.92; Delong test, p = 0.71). Radiomics signature-only model was adopted to predict TDs with accuracy=0.76, sensitivity=0.72 and specificity=0.94 in training cohort and 0.68, 0.62 and 0.97 in validation cohort.
Conclusion
HRMRI-based radiomics models could be helpful for the prediction of LNMs and TDs preoperatively in RC patients.






Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69 (1):7-34. https://doi.org/10.3322/caac.21551
Keum N, Giovannucci E (2019) Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nature reviews Gastroenterology & hepatology 16 (12):713-732. https://doi.org/10.1038/s41575-019-0189-8
Virostko J, Capasso A, Yankeelov TE, Goodgame B (2019) Recent trends in the age at diagnosis of colorectal cancer in the US National Cancer Data Base, 2004-2015. Cancer 125 (21):3828-3835. https://doi.org/10.1002/cncr.32347
Amin MB, Edge SB, Greene FL, Byrd DR, Brookland RK (2017) AJCC cancer staging manual. 8th ed. Springer, New York.
Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen YJ, Ciombor KK, Cohen S, Cooper HS, Deming D, Garrido-Laguna I, Grem JL, Hoffe S, Hubbard J, Hunt S, Kamel A, Kirilcuk N, Krishnamurthi S, Messersmith WA, Meyerhardt J, Miller ED, Mulcahy MF, Nurkin S, Overman MJ, Parikh A, Pate H, Pedersen K, Saltz L, Schneider C, Shibata D, Skibber JM, Sofocleous CT, Stoffel EM, Stotsky-Himelfarb E, Willett CG (2019) National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology. Rectal cancer, Version3. 2019.https://www.nccn.org/patients/guidelines/cancers.aspx#rectal/. Accessed November 27,2019.
Glynne-Jones R, Wyrwicz L, Tiret E, Brown G, Rodel C, Cervantes A, Arnold D (2018) Rectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of oncology : official journal of the European Society for Medical Oncology 29 (Suppl 4):iv263. https://doi.org/10.1093/annonc/mdy161
Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, Hasegawa K, Hotta K, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kinugasa Y, Murofushi K, Nakajima TE, Oka S, Tanaka T, Taniguchi H, Tsuji A, Uehara K, Ueno H, Yamanaka T, Yamazaki K, Yoshida M, Yoshino T, Itabashi M, Sakamaki K, Sano K, Shimada Y, Tanaka S, Uetake H, Yamaguchi S, Yamaguchi N, Kobayashi H, Matsuda K, Kotake K, Sugihara K (2020) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol 25 (1):1-42. https://doi.org/10.1007/s10147-019-01485-z
Diagnosis, Treatment Guidelines For Colorectal Cancer Working Group C (2019) Chinese Society of Clinical Oncology (CSCO) diagnosis and treatment guidelines for colorectal cancer 2018 (English version). Chin J Cancer Res 31 (1):117-134. https://doi.org/10.21147/j.issn.1000-9604.2019.01.07
Jin M, Frankel WL (2018) Lymph Node Metastasis in Colorectal Cancer. Surg Oncol Clin N Am 27 (2):401-412. https://doi.org/10.1016/j.soc.2017.11.011
Kim HJ, Choi GS (2019) Clinical Implications of Lymph Node Metastasis in Colorectal Cancer: Current Status and Future Perspectives. Ann Coloproctol 35 (3):109-117. https://doi.org/10.3393/ac.2019.06.12
Yagi R, Shimada Y, Kameyama H, Tajima Y, Okamura T, Sakata J, Kobayashi T, Kosugi SI, Wakai T, Nogami H, Maruyama S, Takii Y, Kawasaki T, Honma KI (2016) Clinical Significance of Extramural Tumor Deposits in the Lateral Pelvic Lymph Node Area in Low Rectal Cancer: A Retrospective Study at Two Institutions. Ann Surg Oncol 23 (Suppl 4):552-558. https://doi.org/10.1245/s10434-016-5379-9
Nagtegaal ID, Knijn N, Hugen N, Marshall HC, Sugihara K, Tot T, Ueno H, Quirke P (2017) Tumor Deposits in Colorectal Cancer: Improving the Value of Modern Staging-A Systematic Review and Meta-Analysis. J Clin Oncol 35 (10):1119-1127. https://doi.org/10.1200/jco.2016.68.9091
Bouquot M, Creavin B, Goasguen N, Chafai N, Tiret E, Andre T, Flejou JF, Parc Y, Lefevre JH, Svrcek M (2018) Prognostic value and characteristics of N1c colorectal cancer. Colorectal Dis 20 (9):O248-o255. https://doi.org/10.1111/codi.14289
Lord AC, D’Souza N, Pucher PH, Moran BJ, Abulafi AM, Wotherspoon A, Rasheed S, Brown G (2017) Significance of extranodal tumour deposits in colorectal cancer: A systematic review and meta-analysis. European journal of cancer (Oxford, England : 1990) 82:92-102. https://doi.org/10.1016/j.ejca.2017.05.027
Hoshino N, Murakami K, Hida K, Sakamoto T, Sakai Y (2019) Diagnostic accuracy of magnetic resonance imaging and computed tomography for lateral lymph node metastasis in rectal cancer: a systematic review and meta-analysis. Int J Clin Oncol 24 (1):46-52. https://doi.org/10.1007/s10147-018-1349-5
Li XT, Sun YS, Tang L, Cao K, Zhang XY (2015) Evaluating local lymph node metastasis with magnetic resonance imaging, endoluminal ultrasound and computed tomography in rectal cancer: a meta-analysis. Colorectal Dis 17 (6):O129-135. https://doi.org/10.1111/codi.12909
Liu Y, Wen Z, Yang X, Lu B, Xiao X, Chen Y, Yu S (2019) Lymph node metastasis in rectal cancer: comparison of MDCT and MR imaging for diagnostic accuracy. Abdom Radiol (NY) 44 (11):3625-3631. https://doi.org/10.1007/s00261-019-02240-8
Gao Y, Li J, Ma X, Wang J, Wang B, Tian J, Chen G (2019) The value of four imaging modalities in diagnosing lymph node involvement in rectal cancer: an overview and adjusted indirect comparison. Clin Exp Med 19 (2):225-234. https://doi.org/10.1007/s10238-019-00552-z
Langman G, Patel A, Bowley DM (2015) Size and distribution of lymph nodes in rectal cancer resection specimens. Diseases of the colon and rectum 58 (4):406-414. https://doi.org/10.1097/dcr.0000000000000321
Aerts HJ, Velazquez ER, Leijenaar RT, Parmar C, Grossmann P, Carvalho S, Bussink J, Monshouwer R, Haibe-Kains B, Rietveld D, Hoebers F, Rietbergen MM, Leemans CR, Dekker A, Quackenbush J, Gillies RJ, Lambin P (2014) Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun 5:4006. https://doi.org/10.1038/ncomms5006
Lambin P, Leijenaar RTH, Deist TM, Peerlings J, de Jong EEC, van Timmeren J, Sanduleanu S, Larue R, Even AJG, Jochems A, van Wijk Y, Woodruff H, van Soest J, Lustberg T, Roelofs E, van Elmpt W, Dekker A, Mottaghy FM, Wildberger JE, Walsh S (2017) Radiomics: the bridge between medical imaging and personalized medicine. Nature reviews Clinical oncology 14 (12):749-762. https://doi.org/10.1038/nrclinonc.2017.141
Huang YQ, Liang CH, He L, Tian J, Liang CS, Chen X, Ma ZL, Liu ZY (2016) Development and Validation of a Radiomics Nomogram for Preoperative Prediction of Lymph Node Metastasis in Colorectal Cancer. J Clin Oncol 34 (18):2157-2164. https://doi.org/10.1200/jco.2015.65.9128
Horvat N, Carlos Tavares Rocha C, Clemente Oliveira B, Petkovska I, Gollub MJ (2019) MRI of Rectal Cancer: Tumor Staging, Imaging Techniques, and Management. Radiographics 39 (2):367-387. https://doi.org/10.1148/rg.2019180114
Nougaret S, Jhaveri K, Kassam Z, Lall C, Kim DH (2019) Rectal cancer MR staging: pearls and pitfalls at baseline examination. Abdom Radiol (NY) 44 (11):3536-3548. https://doi.org/10.1007/s00261-019-02024-0
Gollub MJ, Arya S, Beets-Tan RG, dePrisco G, Gonen M, Jhaveri K, Kassam Z, Kaur H, Kim D, Knezevic A, Korngold E, Lall C, Lalwani N, Blair Macdonald D, Moreno C, Nougaret S, Pickhardt P, Sheedy S, Harisinghani M (2018) Use of magnetic resonance imaging in rectal cancer patients: Society of Abdominal Radiology (SAR) rectal cancer disease-focused panel (DFP) recommendations 2017. Abdom Radiol (NY) 43 (11):2893-2902. https://doi.org/10.1007/s00261-018-1642-9
Xie C, Du R, Ho JW, Pang HH, Chiu KW, Lee EY, Vardhanabhuti V (2020) Effect of machine learning re-sampling techniques for imbalanced datasets in (18)F-FDG PET-based radiomics model on prognostication performance in cohorts of head and neck cancer patients. European journal of nuclear medicine and molecular imaging. https://doi.org/10.1007/s00259-020-04756-4
Jiang C, Luo Y, Yuan J, You S, Chen Z, Wu M, Wang G, Gong J (2020) CT-based radiomics and machine learning to predict spread through air space in lung adenocarcinoma. European radiology. https://doi.org/10.1007/s00330-020-06694-z
Weng Q, Zhou L, Wang H, Hui J, Chen M, Pang P, Zheng L, Xu M, Wang Z, Ji J (2019) A radiomics model for determining the invasiveness of solitary pulmonary nodules that manifest as part-solid nodules. Clinical radiology 74 (12):933-943. https://doi.org/10.1016/j.crad.2019.07.026
Lopez NE, Peterson CY (2016) Advances in Biomarkers: Going Beyond the Carcinoembryonic Antigen. Clin Colon Rectal Surg 29 (3):196-204. https://doi.org/10.1055/s-0036-1584289
Verberne CJ, Zhan Z, van den Heuvel E, Grossmann I, Doornbos PM, Havenga K, Manusama E, Klaase J, van der Mijle HC, Lamme B, Bosscha K, Baas P, van Ooijen B, Nieuwenhuijzen G, Marinelli A, van der Zaag E, Wasowicz D, de Bock GH, Wiggers T (2015) Intensified follow-up in colorectal cancer patients using frequent Carcino-Embryonic Antigen (CEA) measurements and CEA-triggered imaging: Results of the randomized “CEAwatch” trial. Eur J Surg Oncol 41 (9):1188-1196. https://doi.org/10.1016/j.ejso.2015.06.008
Funding
This study has received funding by Nantong University Clinical Research Project (NO. 2019LQ014).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yang, Ys., Feng, F., Qiu, Yj. et al. High-resolution MRI-based radiomics analysis to predict lymph node metastasis and tumor deposits respectively in rectal cancer. Abdom Radiol 46, 873–884 (2021). https://doi.org/10.1007/s00261-020-02733-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02733-x