Abstract
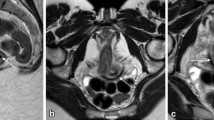
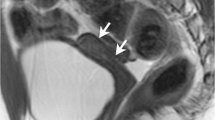
The high contrast resolution provided by magnetic resonance imaging (MRI) compared to all other modalities allows the interpreting radiologist to make a specific diagnosis for many common and uncommon findings. In some cases, the diagnosis can be so certain that there is no differential diagnosis. In this article, we review the most classically recognized findings when interpreting MRI of the pelvis including the following: Ovaries: Simple cyst, hemorrhagic cyst, corpus luteum, dermoid, fibroma/fibrothecoma. Uterus: C-section scar, adenomyosis, endometriosis, fibroid, congenital uterine anomalies. Cervix: nabothian cyst, cervical cancer. Vagina/Vulva: Gardener’s duct cyst, Bartholin’s gland cyst. Urethra: skene gland cyst, urethral diverticulum. Prostate: utricle cyst, Mullerian duct cyst, benign prostatic hyperplasia, prostate cancer.
























Similar content being viewed by others
Availability of data and material
Not applicable.
References
Levine D, Brown DL, Andreotti RF, et al. Management of asymptomatic ovarian and other adnexal cysts imaged at US: Society of radiologists in ultrasound consensus conference statement. Radiology. 2010;256(3):943-954. https://www.ncbi.nlm.nih.gov/pubmed/20505067. https://doi.org/10.1148/radiol.10100213.
Levine D, Patel MD, Suh-Burgmann EJ, et al. Simple adnexal cysts: SRU consensus conference update on follow-up and reporting. Radiology. 2019;293(2):359-371. https://search.proquest.com/docview/2296664852. https://doi.org/10.1148/radiol.2019191354.
Andreotti RF, Timmerman D, Benacerraf BR, et al. Ovarian-adnexal reporting lexicon for ultrasound: A white paper of the ACR ovarian-adnexal reporting and data system committee. Journal of the American College of Radiology. 2018;15(10):1415-1429. https://doi.org/10.1016/j.jacr.2018.07.004. https://doi.org/10.1016/j.jacr.2018.07.004.
Andreotti RF, Timmerman D, Strachowski LM, et al. O-RADS US risk stratification and management system: A consensus guideline from the ACR ovarian-adnexal reporting and data system committee. Radiology. 2020;294(1):168-185. https://www.ncbi.nlm.nih.gov/pubmed/31687921. https://doi.org/10.1148/radiol.2019191150.
Thomassin-Naggara I, Poncelet E, Jalaguier-Coudray A, et al. Ovarian-adnexal reporting data system magnetic resonance imaging (O-RADS MRI) score for risk stratification of sonographically indeterminate adnexal masses. JAMA network open. 2020;3(1):e1919896. https://www.ncbi.nlm.nih.gov/pubmed/31977064. https://doi.org/10.1001/jamanetworkopen.2019.19896.
Thomassin-Naggara I, Aubert E, Rockall A, et al. Adnexal masses: Development and preliminary validation of an MR imaging scoring system. Radiology. 2013;267(2):432-443. https://www.ncbi.nlm.nih.gov/pubmed/23468574. https://doi.org/10.1148/radiol.13121161.
Outwater EK, Siegelman ES, Hunt JL. Ovarian teratomas: Tumor types and imaging characteristics. Radiographics. 2001;21(2):475-490. Accessed Feb 8, 2020. https://doi.org/10.1148/radiographics.21.2.g01mr09475.
Shinagare AB, Meylaerts LJ, Laury AR, Mortele KJ. MRI features of ovarian fibroma and fibrothecoma with histopathologic correlation. AJR Am J Roentgenol. 2012;198(3):296. Accessed Feb 8, 2020. https://doi.org/10.2214/ajr.11.7221.
Rodgers SK, Kirby CL, Smith RJ, Horrow MM. Imaging after cesarean delivery: Acute and chronic complications. Radiographics. 2012;32(6):1693-1712. Accessed Feb 8, 2020. https://doi.org/10.1148/rg.326125516.
Novellas S, Chassang M, Delotte J, et al. MRI characteristics of the uterine junctional zone: From normal to the diagnosis of adenomyosis. AJR. American journal of roentgenology. 2011;196(5):1206-1213. https://www.ncbi.nlm.nih.gov/pubmed/21512093. https://doi.org/10.2214/ajr.10.4877.
Siegelman ES, Oliver ER. MR imaging of endometriosis: Ten imaging pearls. Radiographics. 2012;32(6):1675-1691. Accessed Feb 8, 2020. https://doi.org/10.1148/rg.326125518.
Wilde S, Scott-Barrett S. Radiological appearances of uterine fibroids. Indian J Radiol Imaging. 2009;19(3):222–231. Accessed June 2, 2020. https://doi.org/10.4103/0971-3026.54887.
Deshmukh SP, Gonsalves CF, Guglielmo FF, Mitchell DG. Role of MR imaging of uterine leiomyomas before and after embolization. Radiographics. 2012;32(6):251. Accessed Feb 8, 2020. https://doi.org/10.1148/rg.326125517.
Verma SK, Bergin D, Gonsalves CF, Mitchell DG, Lev-Toaff AS, Parker L. Submucosal fibroids becoming endocavitary following uterine artery embolization: Risk assessment by MRI. American Journal of Roentgenology. 2008;190(5):1220-1226. http://www.ajronline.org/cgi/content/abstract/190/5/1220. https://doi.org/10.2214/ajr.07.3312.
Behr SC, Courtier JL, Qayyum A. Imaging of müllerian duct anomalies. Radiographics. 2012;32(6):233. Accessed Feb 8, 2020. https://doi.org/10.1148/rg.326125515.
Susan J. Freeman, MRCP, FRCR Ahmed M. Aly, et al. The revised FIGO staging system for uterine malig- nancies: Implications for MR Imaging1. RadioGraphics. 2012;32(6):1805-1828. https://pubs.rsna.org/doi/10.1148/rg.326125519. Accessed 2/8/2020. https://doi.org/10.1148/rg.326125519.
Mahajan M, Kuber R, Chaudhari K, Chaudhari P, Ghadage P, Naik R. MR imaging of carcinoma cervix. The Indian journal of radiology & imaging. 2013;23(3):247-252. https://www.ncbi.nlm.nih.gov/pubmed/24347856, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3843334/. https://doi.org/10.4103/0971-3026.120257.
Chaudhari VV, Patel MK, Douek M, Raman SS. MR imaging and US of female urethral and periurethral disease. Radiographics. 2010;30(7):1857-1874. Accessed Feb 8, 2020. https://doi.org/10.1148/rg.307105054.
Chou C, Levenson RB, Elsayes KM, et al. Imaging of female urethral diverticulum: An update. Radiographics. 2008;28(7):1917-1930. Accessed Feb 8, 2020. https://doi.org/10.1148/rg.287075076.
Dwarkasing RS, Dinkelaar W, Hop WCJ, Steensma AB, Dohle GR, Krestin GP. MRI evaluation of urethral diverticula and differential diagnosis in symptomatic women. AJR Am J Roentgenol. 2011;197(3):676-682. Accessed Feb 8, 2020. https://doi.org/10.2214/ajr.10.6144.
Shebel HM, Farg HM, Kolokythas O, El-Diasty T. Cysts of the lower male genitourinary tract: Embryologic and anatomic considerations and differential diagnosis. Radiographics. 2013;33(4):1125-1143. Accessed Feb 8, 2020. https://doi.org/10.1148/rg.334125129.
Kitzing YX, Prando A, Varol C, Karczmar GS, Maclean F, Oto A. Benign conditions that mimic prostate carcinoma: MR imaging features with histopathologic correlation. Radiographics. 2016;36(1):162-175. Accessed Feb 8, 2020. https://doi.org/10.1148/rg.2016150030.
Turkbey B, Rosenkrantz AB, Haider MA, et al. Prostate imaging reporting and data system version 2.1: 2019 update of prostate imaging reporting and data system version 2. Eur Urol. 2019;76(3):340-351. Accessed Feb 8, 2020. https://doi.org/10.1016/j.eururo.2019.02.033.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose. There was no original research conducted for the production of this manuscript. Informed consent was not required. Images were de-identified from the PACS prior to inclusion in the article.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Ethics approval
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kania, L.M., Guglielmo, F. & Mitchell, D. Interpreting body MRI cases: classic findings in pelvic MRI. Abdom Radiol 45, 2916–2930 (2020). https://doi.org/10.1007/s00261-020-02615-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02615-2