Abstract
Objectives
To compare the diagnostic performance of gadoxetic acid-enhanced magnetic resonance imaging (MRI), ultrasonography (US)—based elastography, and serologic fibrosis markers in assessing the stage of liver fibrosis.
Materials and methods
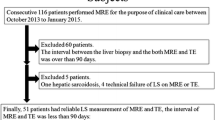
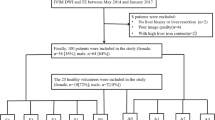
This retrospective study included 67 patients (55 male and 12 female; mean age 62.5 years) who underwent gadoxetic acid-enhanced MRI and liver stiffness measurements before liver biopsy or surgery between January 2014 and January 2018. Measurements were performed using transient elastography (TE), ultrasound shear wave elastography point quantification (ElastPQ), and blood tests. The following MRI-based fibrosis markers were assessed: contrast enhancement index (CEI), liver–spleen contrast ratio (LSC), liver–portal vein contrast ratio (LPC), and signal intensity ratio (SIR). The diagnostic performances of fibrosis markers were compared using the area under the receiver operating characteristic curve (AUC), with histopathologic fibrosis stage as the reference standard.
Results
The fibrosis stages were F0–F1 (n = 17), F2 (n = 7), F3 (n = 20), and F4 (n = 23). MRI-based fibrosis markers negatively correlated with histologic stage: CEI (r = –0.786); LSC (r = − 0.718); LPC (r = − 0.448); and SIR (r = − 0.617; all P < 0.001). For diagnosis of either significant liver fibrosis (≥ F2) or cirrhosis (F4), the CEI provided better diagnostic accuracy (AUC = 0.898 and 0.881) than the aspartate aminotransferase-to-platelet ratio index (APRI) (AUC = 0.699 and 0.715; all P < 0.05). The CEI displayed similar diagnostic accuracy for ≥ F2 or F4 when using TE (AUC = 0.866 and 0.884, both P > 0.05) or ElastPQ [AUC = 0.751 (P = 0.021) and AUC = 0.786 (P = 0.234)].
Conclusions
The CEI measured by gadoxetic acid-enhanced MRI allows the staging of liver fibrosis, with a diagnostic accuracy comparable to that of TE and superior to that of ElastPQ or APRI.




Similar content being viewed by others
Abbreviations
- MRI:
-
Magnetic resonance imaging
- TE:
-
Transient elastography
- ElastPQ:
-
Ultrasound shear wave elastography point quantification
- CEI:
-
Contrast enhancement index
- LSC:
-
Liver–spleen contrast ratio
- LPC:
-
Liver–portal vein contrast ratio
- SIR:
-
Signal intensity ratio
- AUC:
-
Area under the receiver operating characteristic curve
- APRI:
-
Aspartate aminotransferase-to-platelet ratio index
- US:
-
Ultrasound
- MRE:
-
Magnetic resonance elastography
- AST:
-
Aspartate aminotransferase
- SD:
-
Standard deviation
- HBP:
-
Hepatobiliary phase
- PACS:
-
Picture archiving and communication system
- ROI:
-
Region-of-interest
- CBD:
-
Common bile duct
- SI:
-
Signal intensity
- ROC:
-
Receiver operating characteristic
References
Motosugi U, Ichikawa T, Oguri M, Sano K, Sou H, Muhi A, Matsuda M, Fujii H, Enomoto N, Araki T (2011) Staging liver fibrosis by using liver-enhancement ratio of gadoxetic acid-enhanced MR imaging: comparison with aspartate aminotransferase-to-platelet ratio index. Magn Reson Imaging 29:1047-1052. https://doi.org/10.1016/j.mri.2011.05.007
Yoshida H, Shiratori Y, Moriyama M, Arakawa Y, Ide T, Sata M, Inoue O, Yano M, Tanaka M, Fujiyama S, Nishiguchi S, Kuroki T, Imazeki F, Yokosuka O, Kinoyama S, Yamada G, Omata M (1999) Interferon therapy reduces the risk for hepatocellular carcinoma: national surveillance program of cirrhotic and noncirrhotic patients with chronic hepatitis C in Japan. IHIT Study Group. Inhibition of Hepatocarcinogenesis by Interferon Therapy. Ann Intern Med 131:174-181
Regev A, Berho M, Jeffers LJ, Milikowski C, Molina EG, Pyrsopoulos NT, Feng ZZ, Reddy KR, Schiff ER (2002) Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. Am J Gastroenterol 97:2614-2618. https://doi.org/10.1111/j.1572-0241.2002.06038.x
Bedossa P, Carrat F (2009) Liver biopsy: the best, not the gold standard. J Hepatol 50:1-3. https://doi.org/10.1016/j.jhep.2008.10.014
Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD (2009) Liver biopsy. Hepatology 49:1017-1044. https://doi.org/10.1002/hep.22742
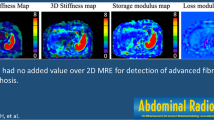
Horowitz JM, Venkatesh SK, Ehman RL, Jhaveri K, Kamath P, Ohliger MA, Samir AE, Silva AC, Taouli B, Torbenson MS, Wells ML, Yeh B, Miller FH (2017) Evaluation of hepatic fibrosis: a review from the society of abdominal radiology disease focus panel. Abdom Radiol (NY) 42:2037-2053. https://doi.org/10.1007/s00261-017-1211-7
Singh S, Venkatesh SK, Wang Z, Miller FH, Motosugi U, Low RN, Hassanein T, Asbach P, Godfrey EM, Yin M, Chen J, Keaveny AP, Bridges M, Bohte A, Murad MH, Lomas DJ, Talwalkar JA, Ehman RL (2015) Diagnostic performance of magnetic resonance elastography in staging liver fibrosis: a systematic review and meta-analysis of individual participant data. Clin Gastroenterol Hepatol 13:440-451.e446. https://doi.org/10.1016/j.cgh.2014.09.046
Venkatesh SK, Yin M, Ehman RL (2013) Magnetic resonance elastography of liver: technique, analysis, and clinical applications. J Magn Reson Imaging 37:544-555. https://doi.org/10.1002/jmri.23731
Venkatesh SK, Ehman RL (2015) Magnetic resonance elastography of abdomen. Abdom Imaging 40:745–759. https://doi.org/10.1007/s00261-014-0315-6
Rockey DC, Bissell DM (2006) Noninvasive measures of liver fibrosis. Hepatology 43:S113–120. https://doi.org/10.1002/hep.21046
Kennedy P, Wagner M, Castera L, Hong CW, Johnson CL, Sirlin CB, Taouli B (2018) Quantitative Elastography Methods in Liver Disease: Current Evidence and Future Directions. Radiology 286:738-763. https://doi.org/10.1148/radiol.2018170601
Asayama Y, Tajima T, Nishie A, Ishigami K, Kakihara D, Nakayama T, Okamoto D, Fujita N, Aishima S, Shirabe K, Honda H (2011) Uptake of Gd-EOB-DTPA by hepatocellular carcinoma: radiologic-pathologic correlation with special reference to bile production. Eur J Radiol 80:e243-248. https://doi.org/10.1016/j.ejrad.2010.10.032
Kobayashi S, Matsui O, Gabata T, Koda W, Minami T, Ryu Y, Kozaka K, Kitao A (2012) Relationship between signal intensity on hepatobiliary phase of gadolinium ethoxybenzyl diethylenetriaminepentaacetic acid (Gd-EOB-DTPA)-enhanced MR imaging and prognosis of borderline lesions of hepatocellular carcinoma. Eur J Radiol 81:3002-3009. https://doi.org/10.1016/j.ejrad.2012.03.029
Akai H, Matsuda I, Kiryu S, Tajima T, Takao H, Watanabe Y, Imamura H, Kokudo N, Akahane M, Ohtomo K (2012) Fate of hypointense lesions on Gd-EOB-DTPA-enhanced magnetic resonance imaging. Eur J Radiol 81:2973-2977. https://doi.org/10.1016/j.ejrad.2012.01.007
Verloh N, Haimerl M, Rennert J, Muller-Wille R, Niessen C, Kirchner G, Scherer MN, Schreyer AG, Stroszczynski C, Fellner C, Wiggermann P (2013) Impact of liver cirrhosis on liver enhancement at Gd-EOB-DTPA enhanced MRI at 3 Tesla. Eur J Radiol 82:1710-1715. https://doi.org/10.1016/j.ejrad.2013.05.033
Ryeom HK, Kim SH, Kim JY, Kim HJ, Lee JM, Chang YM, Kim YS, Kang DS (2004) Quantitative evaluation of liver function with MRI Using Gd-EOB-DTPA. Korean J Radiol 5:231-239. https://doi.org/10.3348/kjr.2004.5.4.231
Tamada T, Ito K, Higaki A, Yoshida K, Kanki A, Sato T, Higashi H, Sone T (2011) Gd-EOB-DTPA-enhanced MR imaging: evaluation of hepatic enhancement effects in normal and cirrhotic livers. Eur J Radiol 80:e311-316. https://doi.org/10.1016/j.ejrad.2011.01.020
Nishie A, Asayama Y, Ishigami K, Tajima T, Kakihara D, Nakayama T, Takayama Y, Okamoto D, Taketomi A, Shirabe K, Fujita N, Obara M, Yoshimitsu K, Honda H (2012) MR prediction of liver fibrosis using a liver-specific contrast agent: Superparamagnetic iron oxide versus Gd-EOB-DTPA. J Magn Reson Imaging 36:664-671. https://doi.org/10.1002/jmri.23691
Tsuda N, Okada M, Murakami T (2010) New proposal for the staging of nonalcoholic steatohepatitis: evaluation of liver fibrosis on Gd-EOB-DTPA-enhanced MRI. Eur J Radiol 73:137-142. https://doi.org/10.1016/j.ejrad.2008.09.036
Lee S, Choi D, Jeong WK (2016) Hepatic enhancement of Gd-EOB-DTPA-enhanced 3 Tesla MR imaging: Assessing severity of liver cirrhosis. J Magn Reson Imaging 44:1339-1345. https://doi.org/10.1002/jmri.25288
Goshima S, Kanematsu M, Watanabe H, Kondo H, Kawada H, Moriyama N, Bae KT (2012) Gd-EOB-DTPA-enhanced MR imaging: prediction of hepatic fibrosis stages using liver contrast enhancement index and liver-to-spleen volumetric ratio. J Magn Reson Imaging 36:1148-1153. https://doi.org/10.1002/jmri.23758
Zhang W, Wang X, Miao Y, Hu C, Zhao W (2018) Liver function correlates with liver-to-portal vein contrast ratio during the hepatobiliary phase with Gd-EOB-DTPA-enhanced MR at 3 Tesla. Abdom Radiol (NY) 43:2262-2269. https://doi.org/10.1007/s00261-018-1462-y
Noda Y, Goshima S, Kajita K, Kawada H, Kawai N, Koyasu H, Matsuo M, Bae KT (2016) Biliary tract enhancement in gadoxetic acid-enhanced MRI correlates with liver function biomarkers. Eur J Radiol 85:2001-2007. https://doi.org/10.1016/j.ejrad.2016.09.003
Lin ZH, Xin YN, Dong QJ, Wang Q, Jiang XJ, Zhan SH, Sun Y, Xuan SY (2011) Performance of the aspartate aminotransferase-to-platelet ratio index for the staging of hepatitis C-related fibrosis: an updated meta-analysis. Hepatology 53:726-736. https://doi.org/10.1002/hep.24105
Motosugi U, Ichikawa T, Sou H, Sano K, Tominaga L, Kitamura T, Araki T (2009) Liver parenchymal enhancement of hepatocyte-phase images in Gd-EOB-DTPA-enhanced MR imaging: which biological markers of the liver function affect the enhancement? J Magn Reson Imaging 30:1042-1046. https://doi.org/10.1002/jmri.21956
Bedossa P, Poynard T (1996) An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology 24:289-293. https://doi.org/10.1002/hep.510240201
Group FMCS (1994) Intraobserver and interobserver variations in liver biopsy interpretation in patients with chronic hepatitis C. The French METAVIR Cooperative Study Group. Hepatology 20:15-20
Koo TK, Li MY (2016) A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med 15:155-163. https://doi.org/10.1016/j.jcm.2016.02.012
Verloh N, Utpatel K, Haimerl M, Zeman F, Fellner C, Fichtner-Feigl S, Teufel A, Stroszczynski C, Evert M, Wiggermann P (2015) Liver fibrosis and Gd-EOB-DTPA-enhanced MRI: A histopathologic correlation. Sci Rep 5:15408. https://doi.org/10.1038/srep15408
Choi YR, Lee JM, Yoon JH, Han JK, Choi BI (2013) Comparison of magnetic resonance elastography and gadoxetate disodium-enhanced magnetic resonance imaging for the evaluation of hepatic fibrosis. Invest Radiol 48:607-613. https://doi.org/10.1097/RLI.0b013e318289ff8f
Feier D, Balassy C, Bastati N, Stift J, Badea R, Ba-Ssalamah A (2013) Liver fibrosis: histopathologic and biochemical influences on diagnostic efficacy of hepatobiliary contrast-enhanced MR imaging in staging. Radiology 269:460-468. https://doi.org/10.1148/radiol.13122482
Noren B, Forsgren MF, Dahlqvist Leinhard O, Dahlstrom N, Kihlberg J, Romu T, Kechagias S, Almer S, Smedby O, Lundberg P (2013) Separation of advanced from mild hepatic fibrosis by quantification of the hepatobiliary uptake of Gd-EOB-DTPA. Eur Radiol 23:174-181. https://doi.org/10.1007/s00330-012-2583-2
Pascolo L, Cupelli F, Anelli PL, Lorusso V, Visigalli M, Uggeri F, Tiribelli C (1999) Molecular mechanisms for the hepatic uptake of magnetic resonance imaging contrast agents. Biochem Biophys Res Commun 257:746-752. https://doi.org/10.1006/bbrc.1999.0454
Tsuboyama T, Onishi H, Kim T, Akita H, Hori M, Tatsumi M, Nakamoto A, Nagano H, Matsuura N, Wakasa K, Tomoda K (2010) Hepatocellular carcinoma: hepatocyte-selective enhancement at gadoxetic acid-enhanced MR imaging--correlation with expression of sinusoidal and canalicular transporters and bile accumulation. Radiology 255:824-833. https://doi.org/10.1148/radiol.10091557
Tsuda N, Matsui O (2010) Cirrhotic rat liver: reference to transporter activity and morphologic changes in bile canaliculi--gadoxetic acid-enhanced MR imaging. Radiology 256:767-773. https://doi.org/10.1148/radiol.10092065
van Montfoort JE, Stieger B, Meijer DK, Weinmann HJ, Meier PJ, Fattinger KE (1999) Hepatic uptake of the magnetic resonance imaging contrast agent gadoxetate by the organic anion transporting polypeptide Oatp1. J Pharmacol Exp Ther 290:153-157
Weinmann HJ, Bauer H, Frenzel T, Muhler A, Ebert W (1996) Mechanism of hepatic uptake of gadoxetate disodium. Acad Radiol 3 Suppl 2:S232-234
Lee NK, Kim S, Kim GH, Heo J, Seo HI, Kim TU, Kang DH (2012) Significance of the "delayed hyperintense portal vein sign" in the hepatobiliary phase MRI obtained with Gd-EOB-DTPA. J Magn Reson Imaging 36:678-685. https://doi.org/10.1002/jmri.23700
Ni Y, Marchal G, Lukito G, Yu J, Muhler A, Baert AL (1994) MR imaging evaluation of liver enhancement by Gd-EOB-DTPA in selective and total bile duct obstruction in rats: correlation with serologic, microcholangiographic, and histologic findings. Radiology 190:753-758. https://doi.org/10.1148/radiology.190.3.8115623
Kim T, Murakami T, Hasuike Y, Gotoh M, Kato N, Takahashi M, Miyazawa T, Narumi Y, Monden M, Nakamura H (1997) Experimental hepatic dysfunction: evaluation by MRI with Gd-EOB-DTPA. J Magn Reson Imaging 7:683-688
Watanabe H, Kanematsu M, Goshima S, Kondo H, Onozuka M, Moriyama N, Bae KT (2011) Staging hepatic fibrosis: comparison of gadoxetate disodium-enhanced and diffusion-weighted MR imaging--preliminary observations. Radiology 259:142-150. https://doi.org/10.1148/radiol.10100621
Takatsu Y, Kobayashi S, Miyati T, Shiozaki T (2016) A novel method for evaluating enhancement using gadolinium-ethoxybenzyl-diethylenetriamine penta-acetic acid in the hepatobiliary phase of magnetic resonance imaging. Clin Imaging 40:1112-1117. https://doi.org/10.1016/j.clinimag.2016.07.001
Dahlqvist Leinhard O, Dahlstrom N, Kihlberg J, Sandstrom P, Brismar TB, Smedby O, Lundberg P (2012) Quantifying differences in hepatic uptake of the liver specific contrast agents Gd-EOB-DTPA and Gd-BOPTA: a pilot study. Eur Radiol 22:642-653. https://doi.org/10.1007/s00330-011-2302-4
Esterson YB, Flusberg M, Oh S, Mazzariol F, Rozenblit AM, Chernyak V (2015) Improved parenchymal liver enhancement with extended delay on Gd-EOB-DTPA-enhanced MRI in patients with parenchymal liver disease: associated clinical and imaging factors. Clin Radiol 70:723-729. https://doi.org/10.1016/j.crad.2015.03.005
Lu Q, Lu C, Li J, Ling W, Qi X, He D, Liu J, Wen T, Wu H, Zhu H, Luo Y (2016) Stiffness Value and Serum Biomarkers in Liver Fibrosis Staging: Study in Large Surgical Specimens in Patients with Chronic Hepatitis B. Radiology 280:290-299. https://doi.org/10.1148/radiol.2016151229
Shaheen AA, Myers RP (2007) Diagnostic accuracy of the aspartate aminotransferase-to-platelet ratio index for the prediction of hepatitis C-related fibrosis: a systematic review. Hepatology 46:912-921. https://doi.org/10.1002/hep.21835
Yilmaz Y, Yonal O, Kurt R, Bayrak M, Aktas B, Ozdogan O (2011) Noninvasive assessment of liver fibrosis with the aspartate transaminase to platelet ratio index (APRI): Usefulness in patients with chronic liver disease: APRI in chronic liver disease. Hepat Mon 11:103-106
Barr RG, Ferraioli G, Palmeri ML, Goodman ZD, Garcia-Tsao G, Rubin J, Garra B, Myers RP, Wilson SR, Rubens D, Levine D (2015) Elastography Assessment of Liver Fibrosis: Society of Radiologists in Ultrasound Consensus Conference Statement. Radiology 276:845-861. https://doi.org/10.1148/radiol.2015150619
Friedrich-Rust M, Ong MF, Martens S, Sarrazin C, Bojunga J, Zeuzem S, Herrmann E (2008) Performance of transient elastography for the staging of liver fibrosis: a meta-analysis. Gastroenterology 134:960-974. https://doi.org/10.1053/j.gastro.2008.01.034
Funding
We declare no sources of financial support or funding received from any organization including National Institutes of Health (NIH); Wellcome Trust; Howard Hughes Medical Institute (HHMI).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All author declares that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was waived for retrospective nature of clinical and imaging data collection in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (TIFF 2245 kb)
Supplementary Figure 1. Receiver operating characteristic curves of MRI-based fibrosis markers for differentiating (a) significant liver fibrosis and (b) cirrhosis. Values were based on the liver stiffness measured with the contrast enhancement index (CEI), liver–spleen contrast ratio (LSC), liver–portal vein contrast ratio (LPC), and signal intensity ratio (SIR).
Rights and permissions
About this article
Cite this article
Jang, H.J., Min, J.H., Lee, J.E. et al. Assessment of liver fibrosis with gadoxetic acid-enhanced MRI: comparisons with transient elastography, ElastPQ, and serologic fibrosis markers. Abdom Radiol 44, 2769–2780 (2019). https://doi.org/10.1007/s00261-019-02041-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02041-z