Abstract
Purpose
Nasoenteric, gastrojejunostomy, and jejunostomy tubes are methods of enteral nutrition in patients with functioning gastrointestinal tracts who cannot maintain adequate oral intake. Current placements; however, may be complicated by redundant wire and catheter loops within the stomach preventing operators from optimal feeding tube placement and predisposing patients to feeding tube prolapse. This report describes the occlusion balloon reduction technique for salvage of malpositioned tubes and placement of new enteric tubes in the setting of redundant loops.
Materials and Methods
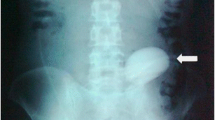
Five patients underwent the occlusion balloon reduction technique for jejunostomy (n = 3), gastrojejunostomy (n = 1), or nasojejunal tube placement (n = 1). All patients (n = 5) had redundant wires coiled within the stomach. In all patients (n = 5), a 9-French × 32 mm × 120 cm Coda balloon was inserted over the wire and passed into the small bowel. The balloon was inflated after which reduction of redundancy in the upper gastrointestinal tract was performed. Feeding tubes were then placed with tips in the distal jejunum. Technical success of the occlusion balloon reduction technique, successful placement of enteric tube, complications, and follow-up were recorded.
Results
The occlusion balloon reduction was technically successful in all patients (n = 5). Feeding tube placement was successful in all patients (n = 5). No minor or major complication occurred. Mean follow-up was 56 days.
Conclusion
The occlusion balloon reduction technique provides a method for reduction of redundant wire and catheter loops within the stomach during enteric tube placement or repositioning.


Similar content being viewed by others
References
Russell M, Stieber M, Brantley S, Freeman AM, Lefton J, Malone AM, Roberts S, Skates J, Young LS. American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) and American Dietetic Association (ADA): standards of practice and standards of professional performance for registered dietitians (generalist, specialty, and advanced) in nutrition support. Nutr Clin Pract. 2007;22:558–586.
Lochs H, Dejong C, Hammarqvist F, Hebuterne X, Leon-Sanz M, Schütz T, van Gemert W, van Gossum A, Valentini L, Lübke H, et al. ESPEN Guidelines on Enteral Nutrition: Gastroenterology. Clin Nutr. 2006;25:260–274.
Niv E, Fireman Z, Vaisman N. Post-pyloric feeding. World J Gastroenterol. 2009;15(11):1281-8.
Srinivasa RN, Chick JFB, Hage AN, Shields JJ, Saad WE, Majdalany BS, et al. Transnasal Snare Technique for Retrograde Primary Jejunostomy Placement After Surgical Gastrojejunostomy. Cardiovascular and Interventional Radiology. 2017; 40(12):1940–4.
Adeleke A, Rammohan G, Jeanomond R. Retrograde Gastrojejunostomy Tube Migration. Case Reports in Emergency Medicine, 2014: 1–3.
Itkin M, DeLegge MH, Fang JC, McClave SA, Kundu S, d’Othee BJ, Martinez-Salazar GM, Sacks D, Swan TL, Towbin RB, Walker TG, Wojak JC, Zuckerman DA, Cardella JF. Multidisciplinary practical guidelines for gastrointestinal access for enteral nutrition and decompression from the Society of Interventional Radiology and American Gastroenterological Association (AGA) Institute, with endorsement by Canadian Interventional Radiological Association (CIRA) and cardiovascular and Interventional Radiological Society of Europe (CIRSE). Journal of Vascular and Interventional Radiology, 2011; 22(8): 1089–1106.
Kalkan IH, Dişibeyaz S, Önder FO, Oztas E, Odemis B, Ozogul Y, Parlak E. A rare complication of percutaneous endoscopic gastrojejunostomy (PEG-J): duodenal bulb perforation due to retrograde migration, Acta Gastro-Enterologica Belgica, 2012; 75(2): 276–277.
Zschau N, Nguyen N, Tam W, Schoeman M. Intestinal perforation: a rare complication of percutaneous endoscopic jejunostomy removal. Endoscopy, 2008; 40(2): article E178.
Weltz AS, Harris DG, O’Neill NA, O’Meara LB, Brenner ML, Diaz JJ. The use of resuscitative endovascular balloon occlusion of the aorta to control hemorrhagic shock during vídeo-assisted retroperitoneal debridement or infected necrotizing pancreatitis. Int J Surg Case Rep, 2015; 13: 15-18, 2015.
Keller BA, Salcedo ES, Williams TK, Neff LP, Carden AJ, Li Y, Gotlib O, Tran NK, Galante JM. Design of a cost-effective, hemodynamically adjustable model for resuscitative endovascular balloon occlusion of the aorta (REBOA) stimulation. J Trauma Acute Care Surg, 2016; 81(3): 606-11.
Doig F, Naidoo R, Sharma V, Tesar P. A unique hybrid approach to complex re-do aortic root surgery. Heart Lung Circ, 2017; 26(11): e68-e70.
Author information
Authors and Affiliations
Contributions
All authors have read and contributed to this manuscript.
Corresponding author
Ethics declarations
Confict of interest
Authors have no relevant disclosures.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chick, J.F.B., Jairath, N., Bundy, J.J. et al. The occlusion balloon reduction technique for de novo placement and salvage of malpositioned enteric tubes. Abdom Radiol 44, 2916–2920 (2019). https://doi.org/10.1007/s00261-019-02029-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02029-9